Pulmonary Embolism
Overview
A pulmonary embolism is a blood clot that blocks and stops or prevents blood flow to the artery in a lung. In most cases, the blood clot begins in a deep vein in the leg and travels to the lungs. Rarely, does the clot form in a vein in another part of a body. When a blood clot forms in one or more of the deep veins in the body, it is known as a DVT(deep vein thrombosis). Because one or more blood clots block or stop the blood flow to the lungs, pulmonary embolism can be life-threatening. Although, prompt treatment greatly decreases the risk of death. Taking measures to prevent blood clots in the legs will assist protect against pulmonary embolism. If people have a pulmonary embolism, their blood oxygen level will be lower than normal. A pulse oximeter device is usually clipped onto the finger and measures the blood oxygen saturation level using red and infrared light through the tissue in the finger. A blood oxygen saturation level of less than 90 percent is abnormal.
What is a Pulmonary embolism?
A pulmonary embolism (PE) is a blood clot in the blood vessels of the lung. This occurs when a clot in another part of the body (often the leg or the arm) moves through the veins to the lungs. A pulmonary embolism restricts blood flow to your lungs, lowers oxygen levels in the lungs, and increases blood pressure in the pulmonary arteries. Pulmonary embolism (PE) happens equally in women and men. The risk increases with age. For every ten years after age 60, the risk of having Pulmonary embolism doubles. Certain inherited conditions, such as factor V Leiden, raise the risk of blood clotting and Pulmonary embolism.
A blood clot that forms in a blood vessel in one area of a body breaks off, and travels to another area of the body in the blood is called an embolus. An embolus can lodge itself in the blood vessel. This could block the blood supply to a particular organ. This blockage of the blood vessel by the embolus is named an embolism. Septic pulmonary embolism (SPE) is an uncommon but serious complication resulting from an infection of the blood. Gram-positive cocci, including methicillin-susceptible Staphylococcus aureus and methicillin-resistant Staphylococcus aureus, are the most common causative organisms of Septic pulmonary embolism.
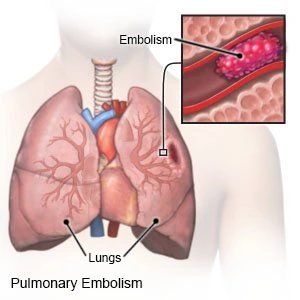
The heart, arteries, capillaries, and veins make up a body’s circulatory system. Blood is pumped with great force from the heart into arteries. From there blood flows into the capillaries (small blood vessels in the tissues). Blood back to the heart through or via the veins. As it moves via the veins back to the heart, blood flow slows. Sometimes this slower blood flow might lead to clot formation. Without quick treatment, a pulmonary embolism can lead to heart or lung damage and even death. A pulmonary embolus is most frequently caused by a blood clot that develops in a vein outside the lungs. The most common blood clot is one in a deep vein of the thigh or the pelvis (hip area). This type of clot is named deep vein thrombosis (DVT). A blood clot breaks off and travels to the lungs where it lodges.
What is the Pathophysiology of pulmonary embolism?
Pulmonary embolism happens when deep venous thrombi detach and embolize the pulmonary circulation. Pulmonary vascular occlusion happens and impairs gas exchange and circulation. In the lungs, the lower lobes are more often affected than the upper, with bilateral lung involvement being common. Larger emboli wedge in a main pulmonary artery, while smaller emboli impede the peripheral arteries. Peripheral pulmonary embolism could lead to pulmonary infarction, and manifested by intra-alveolar hemorrhage. Pulmonary infarction occurs in about 10% of patients without underlying cardiopulmonary disease. The obstruction of the pulmonary arteries makes dead space ventilation as alveolar ventilation exceeds pulmonary capillary blood flow. These contribute to ventilation-perfusion mismatch, with vascular occlusion of the arteries raising pulmonary vascular resistance. In addition, humoral mediators, like serotonin and thromboxane, are released from activated platelets and might trigger vasoconstriction in unaffected areas or parts of a lung. As the pulmonary artery systolic pressure raises, right ventricular afterload raises, leading to right ventricular failure. As right ventricular failure progresses, an impairment in left ventricular filling might develop. Rapid progression to myocardial ischemia might occur secondary to inadequate coronary artery filling, with a potential for hypotension, syncope, electromechanical dissociation, or sudden death.
What are the different types of pulmonary embolisms?
Doctors classify pulmonary embolisms based on severity and location. The severity of pulmonary embolism relates to the risk of serious complications or death. that is measured as low, moderate, or high. Doctors use many criteria to determine the severity:
- symptoms
- lung function
- blood pressure
- blood test results
- oxygen requirements
- imaging exam results, especially echocardiogram results
Doctors may also refer to a high-risk case as a “massive” pulmonary embolism and an intermediate-risk case as a “submassive” pulmonary embolism. Location refers to where the clot is lodged in the lungs. Doctors classify three types of pulmonary embolism by location:
- Saddle pulmonary embolism: In this type, a clot lodges in the main pulmonary artery or one of its left main branches or right main branches. This is a central pulmonary embolism.
- Lobar pulmonary embolism: With this type, a clot lodges in a lobar artery. Each left or right main pulmonary artery branch divides into 2 lobar arteries. Two lobar arteries in each lung supply two lobes in the left lung and three lobes in the right lung. This is also a central pulmonary embolism.
- Distal pulmonary embolism: In this type, a clot lodges in a segmental or subsegmental artery. These are the arteries that supply each or every segment of the lung. The segment is a subsection of a lobe. There are eight segments in the left lung and ten segments in the right lung. This clot is a peripheral pulmonary embolism.
Types of Pulmonary Embolism
Pulmonary emboli can present as acute pulmonary embolism or chronic pulmonary embolism.
Acute pulmonary embolism. it is a new obstruction leading to acute onset heart strain. Acute pulmonary embolism usually requires immediate treatment with clot busters and blood thinning medications.
Chronic pulmonary embolism. it is a more insidious presentation that includes heart failure with gradual progressive symptoms. Chronic pulmonary embolism is caused by an older residual obstruction resulting from an undissolved clot in the pulmonary circulation left over from previous acute pulmonary emboli. In addition, in a small percentage of patients, chronic pulmonary embolism can lead to raised blood pressure in the pulmonary arteries over time, developing into chronic thromboembolic pulmonary hypertension (CTEPH), a rare type of pulmonary hypertension.
To understand CTEPH( chronic thromboembolic pulmonary hypertension ), it is helpful to understand the name:
- Chronic means a condition that lasts a long time, like months or/and years.
- Thromboembolic means that a blood clot, or thrombus, forms in a blood vessel in the body and travels through the arms, the legs, or a vein into blood vessels in the lungs, where it clogs the arteries. A blood clot in the lung is named a pulmonary embolism(PE).
- Pulmonary is a medical term that refers to a lung.
- Hypertension means high blood pressure — in this case, it refers to high blood pressure in the lungs.
Acute Pulmonary Embolism
An acute pulmonary embolism is a sudden blockage in the arteries of the lungs. The blockage begins as a clot in a vein somewhere in the body that travels to a lung. Acute pulmonary embolism is the third most common lead to death from cardiovascular disease after a heart attack and stroke. Approximately 25 to 30 percent of patients will die without immediate treatment.
Clinical Presentation of Acute pulmonary embolism
The clinical presentation of an acute pulmonary embolism is:
- Shortness of breath
- Chest pain
- Rapid or irregular heartbeat
- Fainting episodes
- Lightheadedness
What are the causes and risk factors of acute pulmonary embolism?
DVT blood clots typically develop in a deep vein of the thigh or the pelvis. Most cases of acute pulmonary embolism involve multiple clots that travel from those areas to the lungs but not necessarily all at once. When a lung artery becomes blocked, the areas of the lung the artery feeds do not receive enough blood and can die. this condition called pulmonary infarction makes it more difficult (or hard) for the lungs to provide oxygen to the rest of the body.
Blockages in the blood vessels can a few times result from substances other than blood clots, such as:
- Fat from the marrow of the broken long bone
- Collagen or other tissue
- Part of a tumor
- Air bubbles
Anyone can develop blood clots that cause an acute pulmonary embolism, but certain factors can raise the risk, such as:
- The family medical history of blood clots or pulmonary embolism
- Heart disease, especially heart failure
- Inherited disorders that make the blood more likely to a clot
- Certain cancers, specifically pancreatic, ovarian, and lung cancer, or cancers that have spread (metastatic cancer)
- Surgery, especially bone, brain, or joint surgery
- Long-term immobility like bed rest or inactivity during long plane or car trips.
- Smoking
- Excess weight or obesity
- Pregnancy
- Birth control pills or estrogen therapy
What are the symptoms of acute pulmonary embolism?
Symptoms of an acute pulmonary embolism vary depending on the size of the blood clots, the amount of lung tissue affected, and whether the patient also has heart or lung disease. and the most common symptom is chest pain that:
- Occurs under a breastbone or on one side
- Is sharp or stabbing
- Burns aches or feel dull and heavy
- Worsens with deep breathing
Other signs and symptoms include:
- Sudden cough that can produce blood or/and bloody mucus.
- Shortness of breath that begins suddenly during sleep or on exertion.
- Dizziness, lightheadedness, or fainting
- Low oxygen level in the blood (hypoxemia)
- Fast breathing or wheezing
- Fast heart rate
- Feeling of anxiety
- Leg pain, redness, or swelling
- Low blood pressure
- Low-grade fever
- Clammy or bluish skin (cyanosis)
An acute pulmonary embolism can be life-threatening, so individuals who experience these symptoms should seek immediate medical attention. A condition could also lead to pulmonary hypertension, which is high blood pressure in the lungs and right side of the heart. In rare cases, the clots don’t dissolve over time and become “scarred” in the blood vessels of a lung, leading to chronic thromboembolic pulmonary hypertension.
Chronic Pulmonary Embolism and CTEPH
A chronic pulmonary embolism is a blockage of the pulmonary arteries that occurs when prior clots in these vessels do not dissolve over time despite treatment of an acute pulmonary embolism or the result of an undetected or not treated acute pulmonary embolism. Chronic blood clot accumulation could lead to scar tissue formation in the blood vessels of the lungs, which blocks normal blood flow and makes the right side of the heart work harder. The result is a rare but typically treatable type of severe pulmonary hypertension (high blood pressure in the blood vessels of the lungs) known as chronic thromboembolic pulmonary hypertension (CTEPH). While pulmonary emboli are common, chronic thromboembolic pulmonary hyper ten affects only 2-4 percent of chronic pulmonary embolism patients.
Clinical Presentation of Chronic PE and CTEPH
A clinical presentation of chronic pulmonary embolism is:
- Progressively worsening shortness of breath
- Rapid or irregular heartbeat
- Fainting episodes
- Lightheadedness
- Cough that may produce bloody sputum
If you have unexplained shortness of breath, ask your doctor about getting evaluated for chronic thromboembolic pulmonary hypertension (CTEPH). A ventilation-perfusion scan is a quick, non-invasive screening tool to look for chronic thromboembolic pulmonary hypertension (CTEPH).
How common is a Pulmonary embolism?
Pulmonary embolism is one of the most common blood vessel diseases and heart diseases in the world. It ranks 3rd behind heart attack and stroke. In the united states, about 350,000 individuals a year get Pulmonary embolisms.
What are the signs and symptoms of a Pulmonary embolism?
Pulmonary embolism symptoms can vary greatly, depending on how much of the lung is involved, the size of the clots, and whether you have underlying lung or heart disease. the symptoms of pulmonary embolism vary, depending on the severity of clotting. Although most individuals with a pulmonary embolism experience symptoms, some do not. Pulmonary embolism common symptoms may include:
- Sudden shortness of breath. This symptom typically appears suddenly. Trouble catching your breath occurs even when resting and gets worse with physical activity. whether you have been active or at rest.
- Chest pain. You may feel like people are having a heart attack. The pain is usually sharp and felt when you breathe in deeply. The pain can stop people from being able to take a deep breath. You also may feel it when people cough, bend or lean over. Not explained sharp pain in the chest, arm, shoulder, neck, or jaw. The pain might also be similar to symptoms of a heart attack.
- Fainting. You may pass out if the heart rate or the blood pressure drops suddenly. This is called syncope.
- Cough with or without bloody mucus.
- Pale, clammy, or bluish skin.
- Rapid heartbeat (pulse).
- Excessive sweating.
- In a few cases, feeling anxious, lightheaded, faint, or pass out.
- Wheezing.
Symptoms of a pulmonary embolism generally come on suddenly, and you should seek urgent medical attention if you experience the following:
- A cough, which may contain blood
- A heavy feeling in the chest, or the chest pain
- Dizziness or a feeling of being ‘light-headed’
- Pain in your back
- Rapid heart rate
- Shortness of breath
- Sweating is more than usual.
Symptoms of a DVT(Deep vein thrombosis) include the following:
- An area on either the arm or the leg that feels warm or hot to touch
- Leg pain or tenderness, especially in a calf
- Redness of the skin in the affected arm or the leg
- Swelling in either an arm or leg
- Veins in the arm or the leg that are larger than normal.
If a DVT(Deep vein thrombosis) is found earlier enough, doctors can decrease the risk of a pulmonary embolism. You must seek urgent medical attention if you experience any of the above DVT(Deep vein thrombosis) symptoms as well. Other symptoms that can happen with pulmonary embolism include:
- A cough that may include bloody or/and blood-streaked mucus
- Rapid or irregular heartbeat
- Lightheadedness or dizziness
- Excessive sweating
- Fever
- Leg pain or swelling, or both, typically in the back of a lower leg
- Clammy or discolored skin, called cyanosis
Vital signs (blood pressure, heart rate, respiratory rate, and oxygen saturation) might be normal or abnormal, depending upon the size of the embolus and how much lung tissue is affected. The larger the clot burden (or load), the less stable vital signs. Abnormal vital signs may include:
- Tachycardia: elevated heart rate (tachy=fast + cardia=heart);
- Tachypnea: elevated or raised respiratory (breathing) rate.(tachy=fast + pnea= breathing);
- Hypotension: decreased or reduced blood pressure (hypo=low + tension=blood pressure);
- Hypoxia: decreased SaO2. Oxygen saturation described how many hemoglobin molecules are carrying or taking oxygen. Normal oxygen level is generally greater than 92%-93%.
The condition progresses as follows:
- The heart rate and the respiratory rate may raise as the body tries to compensate for the decreased oxygen transfer capabilities in the lung. This allows the oxygen that is available to be circulated more quickly, supplying the body’s organ and tissue requirements as best as possible.
- This might lead to anxiety, weakness, and lightheadedness as the body’s organs are deprived of the necessary oxygen to function.
- If the clot burden is large enough, it might make it harder for the heart to pump blood through the blocked pulmonary arteries. This raises the work that the heart has to do, raising pressures inside the heart and straining the heart muscle itself.
Sudden death is an initial sign of a condition in up to 25% of cases. The person collapses, stops or prevents breathing, and people heart stops beating (cardiac arrest) without prior symptoms. Pulmonary embolus is the second leading cause of sudden death and is behind coronary artery disease. If people have any symptoms of pulmonary embolism, get medical attention immediately. Because you can have a blood clot and not have any symptoms, discuss the risk factors with the healthcare provider.
What are the warning signs of PE(pulmonary embolism)?
The first signs of pulmonary embolism are commonly shortness of breath and chest pains that get worse if you exert yourself or take a deep breath. You might cough up bloody mucus. If people have these types of symptoms, get medical attention right away. Pulmonary embolism is serious but very treatable. Quick treatment greatly decreases the chance of death.
What causes a pulmonary embolism?
A pulmonary embolism happens when a clump of material, most frequently a blood clot, gets stuck in an artery in the lungs, blocking the flow of blood. Blood clots most typically come from the deep veins of the legs, a condition known as deep vein thrombosis. In Several cases, multiple clots are involved. The portions of the lung served by each blocked artery can not get blood and may die. This is known as a pulmonary infarction. This makes it more difficult or challenging for the lungs to provide oxygen to the rest of the body.Generally, a pulmonary embolism is caused by a blood clot traveling up from one of the deep veins in your body, usually in the leg. This kind of blood clot is named deep vein thrombosis (DVT). In a few cases, the blood clot happens because of a change in the physical condition, such as pregnancy or recent surgery. Occasionally, blockages in the blood vessels are led to by substances other than blood clots, such as:
- A Fat from the inside of a broken long bone
- Part of a tumor
- Air bubbles
Pulmonary embolism causes include:
- Blood collecting or “pooling” in a certain part of the body (typically an arm or leg). Blood typically pools after long periods of inactivity, such as after surgery or bed rest.
- Injuries to a vein, such as from a fracture or surgery (specifically in the pelvis, hip, knee, or leg).
- Other medical conditions, like cardiovascular disease (including congestive heart failure, atrial fibrillation, heart attack, or stroke).
- Generally, a pulmonary embolism is caused by a blood clot traveling up from one of the deep veins in your body, usually in the leg. This kind of blood clot is named deep vein thrombosis (DVT). In a few cases, the blood clot happens because of a change in the physical condition, such as pregnancy or recent surgery.
- An increase or decrease in the blood’s clotting factors. Elevated clotting factors can happen with some types of cancer or in some individuals taking hormone replacement therapy or birth control pills. Abnormal or low clotting factors might also happen as a result of blood clotting disorders.
- Blood clotting is a normal process to prevent or stop bleeding. people’s body makes blood clots and then breaks them down. Under certain circumstances, the body might be unable to break down a clot. These might result in serious health problems (or issues).
- When blood clots in a vein, it might be due to slowed blood flow, an abnormality in clot forming, or an injury to the blood vessel wall.
- Blood clots can form in arteries and veins. Clots formed in veins. that are called venous clots. Veins of the legs can be superficial veins (close to the surface of the skin) or/and deep veins (located near the bone and surrounded by muscle).
- Venous clots most frequently happen in the deep veins of the legs. This is called deep vein thrombosis (DVT). Once a clot has formed in the deep veins of a leg, there is a potential for part of the clot to break off and travel via the blood to another area of the body, frequently the lung. deep vein thrombosis is the most common lead to pulmonary embolism. Almost all pulmonary embolisms are caused by a blood clot that originates in the deep veins of the legs or the pelvis. When a blood clot forms in the deep veins of the legs or the pelvis, this is a condition known as deep vein thrombosis (DVT). A pulmonary embolism is caused when a blood clot, or part of a blood clot, breaks off and travels through the bloodstream, eventually leading to a blockage in the arteries of the lungs.
- Other less frequent sources of pulmonary embolism are a fat embolus (frequently linked to the breaking of a large bone), amniotic fluid embolus, air bubbles, and deep vein thrombosis in the upper body. the clots might also form on the end of an indwelling intravenous (IV) catheter, break off, and travel to the lungs.
How serious is a pulmonary embolism?
With proper diagnosis and treatment, pulmonary embolism is seldom fatal. Although, untreated or nontreated pulmonary embolism can be serious, leading to other medical complications, including death. About 33% of individuals with a pulmonary embolism die before they get the diagnosis and the treatment. A pulmonary embolism can:
- Cause damage to the lungs.
- Cause strain on the heart, leading to heart failure.
- Be life-threatening, depending on the size of a clot.
Risk factors
- Although anyone can develop blood clots that result in a pulmonary embolism, certain factors can raise the risk.
- History of blood clots
- You are at a higher risk if you or any of the blood relatives, such as a parent or sibling, have had venous blood clots or a pulmonary embolism in the past.
Who is at risk for a pulmonary embolism?
Several factors raise the risk of developing pulmonary embolism, but not all individuals with risk factors will develop one. Individuals at risk of developing pulmonary embolism include those who:
- Have a blood clot in that leg, or deep vein thrombosis (DVT).
- Genetic conditions that raise the risk of blood clot formation
- A family history of blood clotting disorders
- Surgery or injury (specifically to the legs) or orthopedic surgery
- Situations in which mobility is limited, such as extended bed rest, flying or riding long distances, or/and paralysis
- Previous history of clots
- Older age. The risk raises with age.
- Cancer and cancer therapy
- Certain medical conditions, like heart failure, COPD(chronic obstructive pulmonary disease), high blood pressure, stroke, and inflammatory bowel disease.
- Certain medicines, like birth control pills and estrogen replacement therapy
- During and after pregnancy, including after a cesarean section
- Enlarged veins in the legs (varicose veins)
- Cigarette smoking
- Are inactive for long periods while traveling via motor vehicle, train, or plane (such as a long, cross-country car ride).
- Have recently had trauma or an injury to a vein, possibly after a recent surgery, fracture, or from varicose veins.
- Are taking birth control pills (oral contraceptives) or/and hormone replacement therapy?
- Have a history of heart failure or/and stroke.
- Have overweight (a Body Mass Index or BMI greater than 25)/obesity (a BMI greater than 30).
- Are pregnant or/and have given birth in the previous six weeks?
- Received a central venous catheter through their arm or their leg.
- Central venous catheters: This tubing is placed in a large vein, typically for long-term delivery of medications, fluids, or nutrients.
- Chronic conditions: These include cancer, heart or lung disease, and inflammatory bowel disease.
- High estrogen levels: The raised estrogen levels may be from oral contraceptives or hormone therapy. The body also produces higher levels of estrogen up to three months after giving birth.
- History of clotting disorders: This includes a personal or family history of deep vein thrombosis or pulmonary embolisms.
- Long periods of immobility: Several factors can limit mobility and blood flow. These can include prolonged bed rest after surgery or due to medical conditions, and sitting for long periods such as on long trips by car or airplane.
- Traumatic injury: This includes trauma from a motor vehicle accident, fall, or/and another traumatic injury.
- Severe illness: This includes infections that might predispose someone to venous thrombosis.
- Vascular issues: These include varicose veins or injury to a vein due to fracture or major surgery.
- Other health concerns: These include obesity or/and smoking.
If you have any of these risk factors and you have had a blood clot, talk with the healthcare provider so they can take steps to decrease the risk.
Other risk factors
- Smoking. For reasons that are not well understood, tobacco use raises the risk of blood clots in a few people, specifically those who have other risk factors.
- Being overweight. Excess weight raises the risk of blood clots — particularly in individuals with other risk factors.
- Supplemental estrogen. The estrogen in birth control pills and hormone replacement therapy can raise clotting factors in the blood, specifically in those who smoke or are overweight.
- Pregnancy. The weight of a baby pressing on veins in the pelvis could slow blood return from the legs. Clots are more such as forming when blood slows or pools.
When to see a doctor
- A pulmonary embolism can be life-threatening. Seek urgent medical attention if people experience unexplained shortness of breath, chest pain, or fainting.
Differential Diagnosis
Pulmonary embolism might be confused with other conditions impacting the cardiopulmonary system. These conditions include:
- Acute heart failure
- Pneumonia
- Chronic obstructive pulmonary disease exacerbation
- Atrial fibrillation
- Acute myocardial infarction
How is a pulmonary embolism diagnosed?
To make a pulmonary embolism diagnosis, the doctor will take a medical history, perform an exam, and order tests. Questions the doctor may ask include:
- What symptoms are you experiencing?
- When did the symptoms start?
- Are the symptoms persist or do they come and go?
- How severe are the symptoms?
- What, if anything, seems to make the symptoms better or/and worse?
- Do you have a history of blood clots, deep vein thrombosis, or pulmonary embolisms?
- Does anyone in the family have a problem with blood clots?
- What other medical conditions do you have?
- What medications do you take?
During the exam, the doctor will listen to the heart and the lungs. It will also be important for the doctor to examine the legs for symptoms of deep vein thrombosis. This includes warmth, redness, and swelling. Tell the doctor if the leg is tender or sore. Testing is necessary because it is difficult to diagnose pulmonary embolism using symptoms alone. Pulmonary embolism (PE) is often difficult to diagnose because the symptoms of pulmonary embolism are a lot like those of many other conditions and diseases. A provider would use the following tests to make a pulmonary embolism diagnosis. Along with a complete medical history and a physical examination, the tests used to look for the pulmonary embolism might include:
- Blood tests (including the D-dimer test). This detects fragments of breakdown products of the blood clot. The higher the level, the more likely individuals have a blood clot in a vein. Unfortunately, the test can be positive in many other situations, such as if you have had recent surgery or if you are pregnant. A positive test does not, therefore, diagnose a deep vein thrombosis or a pulmonary embolism. The test may, although, indicate how likely it is that you have a blood clot (the clot can be either a deep vein thrombosis or a pulmonary embolism). This can assist decide if further tests are required. A negative D-dimer result when you are at lower risk of VTE means the chance of having a thrombus is extremely low. However, if the VTE risk is high, then a D-dimer test cannot rule out the possibility of a thrombus and you will need other tests.
- Lab tests. blood tests are used to check the blood’s clotting status, including a test named the D-dimer level test. Other blood work might include testing for genetic disorders that might contribute to abnormal clotting of the blood. Arterial blood gases might be checked to see how much oxygen is in the blood.
- Computed tomography (CT) angiogram. This type of test is an imaging test that uses X-rays and a computer to make detailed pictures of a body. The Computed tomography(CT) scan shows details of the organs, bones, muscles, and fat. Computed tomography(CT) with contrast enhances an image of the blood vessels in the lungs. Contrast is a dye-like substance injected into a vein that leads to the organ or tissue under study showing up more clearly on the scan.
- Duplex ultrasound (US). This type of vascular ultrasound is done to assess blood flow and the structure of the blood vessels in people’s legs. (Blood clots from the legs generally dislodge and travel into the lung.) Ultrasound uses high-frequency sound waves and a computer to create images of blood vessels, tissues, and organs. Ultrasound of the leg. (This assists identify blood clots in individuals’ legs, or deep vein thrombosis, which can move to the lungs and become a pulmonary embolism and cause more damage.)
- Ultrasound scan of the leg. A type of ultrasound named a duplex Doppler is used to show blood flow in the veins in the leg, and any blockage to blood flow. Ultrasound is useful because it is an easy, non-invasive test and might show up as a deep vein thrombosis. If a deep vein thrombosis is found, then a Pulmonary embolism can be assumed to lead to the other symptoms (such as breathlessness or chest pain). Treatment (with anticoagulant medication – see below) can be started immediately for both the deep vein thrombosis and the suspected Pulmonary embolism. The Treatment is commonly the same (or exact) for both. Further tests might be not necessary for this situation.
- although, if the ultrasound is negative, a deep vein thrombosis or Pulmonary embolism is not ruled out, because a few clots do not show up on ultrasound. Further tests will be needed.
- Lower limb compression venous ultrasound might be useful for pregnant women in whom irradiation from other imaging might be harmful.
- Magnetic resonance imaging (MRI). This imaging test uses a combination of a magnetic field, radio frequencies, and a computer to make detailed images of organs and structures within the body. Magnetic resonance imaging scans use magnetic waves and computers to create two-dimensional pictures and three-dimensional pictures of the inside of the body. That is an important tool for diagnosing pulmonary embolisms. Before the test begins, you receive an injection of contrast dye, which allows the doctor to see the arteries in the lungs clearly on the magnetic image. A technician takes the pictures while people lie very still. The test takes 40 minutes to 90 minutes.
- Electrocardiogram (EKG). The electrocardiogram is one of the simplest test and quickest tests used to evaluate a heart. Electrodes (small, sticky patches) are placed at specific spots on the chest, the arms, and the legs. The electrodes are connected to an Electrocardiogram machine by lead wires. The electrical activity of the heart is measured, printed out, and interpreted.
- A Ventilation/perfusion (V/Q) scans. if you are unable to get contrast for a CT scan. (This is a nuclear scan that can detect clots in the lung.)For this nuclear radiology test, a small amount of a radioactive substance is used to assist examine the lungs. A ventilation scan evaluates ventilation or the movement of air into and out of the bronchi and the bronchioles. A perfusion scan assesses blood flow within the lungs. Ventilation-perfusion scans (V/Q scans) are another less generally used test in people who cannot undergo a chest CT scan to make the diagnosis of pulmonary embolism. The scan uses inhaled gas (V) and injected dye (Q) to compare areas of a lung where air can enter with the areas of the lung that are getting blood supply. If there is a mismatch after then there is a possibility (or chance) that blood clotting exists. V/Q scans take hours to perform and are read by a radiologist as the low, medium, and high probability that a blood clot is present. A low probability result means that there is still a 5% to 15% chance that a pulmonary embolism exists. For that reason, V/Q scans are not frequently performed.
Other tests the provider may order include:
- Pulmonary angiogram. This X-ray image of the blood vessels is used to evaluate different conditions, such as aneurysm (bulging of a blood vessel), stenosis (narrowing of a blood vessel), or blockages. A dye (contrast) is injected via a thin flexible tube placed in an artery. This dye makes blood vessels show up on X-ray. Historically, a gold standard for the diagnosis of pulmonary embolus was a pulmonary angiogram, in which a catheter was threaded into the pulmonary arteries, typically from veins in the groin or the wrist. Dye was injected into the pulmonary arteries and could recognize whether blood clots were present. This is an invasive test and needs a skilled radiologist to insert the catheter.
- CT scan is more commonly used today, and pulmonary angiography is most frequently performed in unusual circumstances.
- Chest X-ray. This imaging test is used to assess the lungs and the heart. Chest X-rays show information about the size, shape, contour, and anatomic area of the heart, lungs, bronchi (large breathing tubes), aorta and pulmonary arteries, and mediastinum (area in the middle of the chest separating the lungs).
Diagnosing Acute Pulmonary Embolism
The cardiovascular specialists conduct a thorough evaluation, which begins with the:
- Physical exam
- Review of personal and family medical history
- Discussion of symptoms
We have extensive experience in evaluating and diagnosing acute pulmonary embolism, which can be difficult to diagnose in individuals with heart disease or lung disease. To confirm a diagnosis, we commonly order one or more tests, such as:
- Blood tests: We measure levels of oxygen, carbon dioxide, and a clot-dissolving substance named D-dimer, as well as check for an inherited clotting disorder.
- Duplex ultrasound: the technician scans the legs to check for blood clots in the veins.
- Spectral CT angiogram: We use a scanner that takes clear images of the lung tissue and the blood vessels to decide where the clots are and how they are affecting lung blood flow.
- Magnetic resonance imaging (MRI): Magnetic resonance imaging uses a magnetic field and radio waves to produce images, avoiding the use of radiation in X-rays and CT scans.
- Chest X-ray: Blood clots cannot be seen with X-rays, but these images can rule out other conditions with the same symptoms. A chest x-ray cannot prove that pulmonary embolism is present or absent because clots do not show up on the x-ray. Nevertheless, a chest x-ray is a useful test in the evaluation of pulmonary embolism because it can find other diseases, such as pneumonia or fluid in the lungs, that may explain a person’s symptoms.
What are the medical conditions and treatments of a Pulmonary embolism?
A Few medical conditions and treatments put people at risk, such as:
- Heart disease. Heart and blood vessel disease, especially heart failure, makes clot formation more likely.
- Cancer. Certain cancers — specifically brain, ovary, pancreas, colon, stomach, lung, and kidney cancers, and cancers that have spread — can raise the risk of blood clots. Chemotherapy further raises the risk. You also have a higher risk of blood clots if you have a personal history or family history of breast cancer and are taking tamoxifen or raloxifene (Evista).
- Surgery. Surgery is one of the leading leads to of problem blood clots. For this cause, medicine to prevent clots may be given before and after major surgery, such as joint replacement.
- Disorders that affect clotting. A few inherited disorders affect the blood, making it more likely to clot. Other medical disorders such as kidney disease also can raise the risk of blood clots.
- Coronavirus disease 2019 (COVID-19). People who have severe symptoms of COVID-19 have a raised risk of pulmonary embolism.
Extended periods of inactivity
Blood clots are more such as to form during longer than usual periods of inactivity, such as:
- Bed rest. Being confined to bed for an extended period after surgery, a heart attack, leg fracture, trauma or any serious illness puts people at risk of blood clots. When the legs lie flat for long periods, the flow of blood through the veins slows down and blood can pool in the legs. This sometimes could result in blood clots.
- Long trips. Sitting in a cramped position during lengthy plane or car trips or travels slows blood flow in the legs, which raises the risk of blood clots.
How is a Pulmonary embolism treated?
If a GP thinks you have got a pulmonary embolism, you will be sent to the hospital for further tests and treatment. At the hospital, you will probably be given an injection of anticoagulant medicine before you get any test results. Anticoagulants stop blood clots from getting bigger and stop new clots from forming. If tests confirm people have a pulmonary embolism, you will continue with anticoagulant injections for at least 5 days. You will also require to take anticoagulant tablets for at least 3 months. You should make a full recovery from a pulmonary embolism if it is spotted and treated early.
Healthcare providers generally treat a pulmonary embolism in a hospital, where they can monitor your condition closely. The length of the pulmonary embolism treatment and hospital stay will vary, depending on the severity of the clot. The main treatment for pulmonary embolism is an anticoagulant (blood thinner). Depending on the severity of your clot and its effect on the other organs such as your heart, people may also undergo thrombolytic therapy, surgery, or interventional procedures to improve blood flow in their pulmonary arteries.
- Prevention is the best treatment for a pulmonary embolus. Minimizing the risk of deep vein thrombosis(DVT) is key in preventing a potentially fatal illness.
- The treatment for pulmonary embolism is anticoagulation.
- Once the diagnosis of pulmonary embolism is made, it is important to know the severity of the illness and whether the patient requires to be hospitalized or whether treatment can happen at home.
- The Pulmonary Embolus Severity Index (PESI) can assist in risk-stratify who is stable and who may potentially be unstable. It takes the following factors into history:
- Age
- Sex
- History of cancer, heart disease, lung disease
- Vital signs
- Mental status
- All patients with abnormal vital signs (heart rate, respiratory rate, blood pressure, and oxygen saturation) are required to be admitted to the hospital.
- Those who have unstable social situations, have difficulty obtaining medication or have difficulty understanding their medication may need observation before being discharged home.
When patients with pulmonary embolism are admitted to a hospital, it is because they are unstable with abnormal vital signs, or there is a concern that they will become unstable. The initial treatment of choice or option is unfractionated heparin, an injectable blood thinner that is continuously given intravenously. If vital signs are not stable, other alternative treatments might be considered based on the clinical situation. Complications could include shock with low blood pressure (hypotension), confusion, coma, or heart failure. A tissue plasminogen activator (tPA) or alteplase is an injectable clot-busting drug.
Anticoagulant medications
In most cases, the treatment consists of anticoagulant medications (blood thinners). Anticoagulants decrease your blood’s ability to clot. This stops future blood clots. As with any medicine, it is important to understand how and when to take the anticoagulant and follow the provider’s guidelines. The diagnosis will determine the type of medication you will take, how long you require to take it, and the type of follow-up monitoring you will require. Be sure to keep all scheduled follow-up appointments with the provider and the laboratory so they can monitor the response to the medication. While taking anticoagulants, the follow-up will include frequent blood tests (prothrombin time test) to see how fast the blood clots. This assists the provider know if you are taking the right dose.
Anticoagulation, (or blood-thinning).that is the treatment of choice for both pulmonary embolism and deep vein thrombosis. Anticoagulation stops further blood clot formation and stops an embolization of a clot to the lung from existing clots. Under normal conditions, the body would activate a system that would break down blood clots within four to six weeks. The recommendations were based on a review of numerous clinical trials and meta-analyses (statistical evaluation) in the medical literature.
- In patients with VTE and no cancer, a drug of choice is a direct oral anticoagulant (DOAC) such as:
- apixaban (Eliquis)
- rivaroxaban (Xarelto)
- edoxaban (Sayvessa)
- dabigatran (Pradaxa)
- In patients with VTE and active cancer, a drug of choice is enoxaparin (Lovenox).
- The National Comprehensive Cancer Network suggests that DOACs might be an acceptable alternative to enoxaparin.
- Apixaban medication and rivaroxaban medication are oral medications that have a relatively rapid (or fast) onset of action and become effective within three to four days.
- Edoxaban and dabigatran take a long to become effective and, hence, there is a two-step process for their use. Either intravenous heparin or subcutaneous enoxaparin requires to be used until the oral medications become effective.
- Coumadin (warfarin) has historically been the medication(or drug )of choice for the treatment of VTE. It takes many days to reach its therapeutic range in the body and, therefore, it too needs the use of heparin or enoxaparin until the medicine is effective.
- Certain clinical conditions also affect the choice of anticoagulation. Pregnancy, those who are breastfeeding, it presence of liver failure or kidney failure, and the presence of antiphospholipid syndrome might require specific anticoagulation medications. A healthcare professional requirements to match the clinical situation with the appropriate medication.
- The dosing of Coumadin is monitored by blood tests. INR (international normalized ratio) is used to guide the amount of Coumadin that is taken every day to keep the blood appropriately thinned. Certain foods and medications could interact with Coumadin and affect the dosing.
- DOACs do not require blood tests to monitor their effectiveness or dosing. There are drug interactions that require to be considered when they are prescribed.
Compression stockings
- Compression stockings (support hose) enhance blood flow in the legs. People with deep vein thrombosis frequently use them. You should use them as the provider prescribes. The stockings are generally knee-high in length and compress the legs to prevent the blood from pooling. Talk with the provider about how to use the compression stockings, for how long, and how to care for them. It is important to wash compression stockings according to directions to prevent damaging them. Compression stockings steadily squeeze the legs, assisting veins and leg muscles to move blood more efficiently. They offer a safe, simple, and inexpensive way to maintain blood from pooling in the legs during and after surgery.
Procedures
- If a pulmonary embolism is life-threatening, or if other treatments are not effective, the provider may recommend using surgery or a catheter to remove the blood clot from the pulmonary artery.
Thrombolytic therapy. Thrombolytic medications (“clot busters”), including tissue plasminogen activator (TPA), dissolve the clot. The person always receives thrombolytics in the intensive care unit (ICU) of a hospital where a provider could monitor them. people may receive this type of medication if they have a special situation, such as low blood pressure or an unstable condition because of a pulmonary embolism.
Fibrinolytic therapy. Also named clot busters, these medicines are given intravenously (IV or into a vein) to break down a clot. These types of medicines are only used in life-threatening situations.
Vena cava filter. The small metal device placed in the vena cava (the large blood vessel that backs blood from the body to the heart) may be used to keep clots from traveling to the lungs. These filters are typically used when people can not get anticoagulation treatment (for medical reasons), develop more clots even with anticoagulation treatment, or when have bleeding problems from anticoagulation medicines.
Pulmonary embolectomy. Rarely used, this type of is surgery done to remove a pulmonary embolism. It is typically done only in severe cases when the pulmonary embolism is very large, you can not get anticoagulation and/or thrombolytic therapy due to other medical problems or people who have not responded well to those treatments, or the condition is unstable.
Percutaneous thrombectomy. A long, thin, hollow tube (catheter) can be threaded via the blood vessel to the site of the embolism guided by X-ray. Once the catheter is in place, it is used to break up the embolism, pull it out, or dissolve it using thrombolytic medicine.
Pregnancy and postnatal period
- There is a raised risk of a pulmonary embolism at any stage of the pregnancy until six weeks postnatally. Any symptoms of deep vein thrombosis or pulmonary embolism in a pregnant or postnatal woman should be taken seriously and investigated immediately.
- Treatment in pregnancy is with heparin injections instead of warfarin tablets. This is because warfarin can potentially lead to harm (birth defects) to the unborn child. For a massive pulmonary embolism where a person is unwell, any of the additional treatments listed above may be used.
- Treatment in pregnancy is continued until 3 months after the embolism or until 6 weeks postnatally, whichever is longer.
- Postnatally, warfarin can be begun in place of heparin, once bleeding from birth has settled.
- Heparin and warfarin could be taken by breastfeeding mothers. If taking warfarin and breastfeeding, it is advisable to assure that the baby has had its routine vitamin K injection. This is because vitamin K assists counteract the effects of warfarin. (In the UK, all babies(or infants) are routinely given a vitamin K injection at birth time, unless parents object. Vitamin K assists prevent clotting problems in newborn babies anyhow, regardless of whether the mother is taking treatment.)
Duration of treatment
- People commonly take anticoagulation medications for a minimum of three to six months. At that time, a decision will be made based on their risk of developing recurrent clots as to whether they should continue with long-term therapy.
- Risk stratification may include whether a blood clot was provoked or not provoked. An example of a provoked blood clot would be a person who broke their leg, was placed in a cast, and was sedentary. Those who have VTE frequently undergo hypercoagulable evaluations looking for genetic or familial leads to blood clots.
- If a health care professional, in consultation with the patient (shared decision-making), decides that lifelong therapy is needed, that decision should be reviewed every year to determine if the risk of clotting still exists and whether a risk of clotting is greater than a risk of bleeding.
Physiotherapy Implications
- Mobility is vital to patient recovery following pulmonary embolism. Following anticoagulation and thrombolytic therapies, bed rest is generally prescribed followed by inpatient therapy. The main aim of physiotherapy is to restore the clear lung field and oxygen uptake to an optimal level. This might be achieved through chest physiotherapy and then progressed to include endurance exercises such as walking or bicycle ergometry.
Pulmonary Rehabilitation
- Pulmonary rehabilitation assists patients regain strength and endurance following treatment for a pulmonary embolism. people exercise under the guidance of respiratory therapists and attend education sessions to learn about breathing techniques, medications, oxygen therapy, etc.
Reduce your pulmonary embolism risk
- A pulmonary embolism often occurs when part of the blood clot dislodges itself from your leg and travels up to your lungs, leading to a blockage.
- There are measures you can take to lower the risk of getting a pulmonary embolism.
- If you are being treated in a hospital for another condition, your medical team should take steps to prevent deep vein thrombosis.
- A deep vein thrombosis can occasionally develop on journeys lasting more than 6 hours.
- To reduce your risk of getting a travel-related deep vein thrombosis :
Do
- sit comfortably in the seat and lie back as much as possible
- wear loose-fitting clothing
- make sure people have plenty of legroom
- drink water regularly
- take regular breaks from sitting
- bend and straighten the legs, feet, and toes every 30 minutes while seated
- Press the balls of the feet down hard against the floor every so often
- wear flight socks
Don’t
- do not sit for long periods without moving: Try not to stay seated for more than 2 hours at a time — get up and walk around regularly. If you had a deep vein thrombosis in one of your legs, don’t cross your legs when you sit down. That position can affect your circulation. Be mindful of this when you are on long flights or driving for a long time.
- do not drink alcohol
- don’t drink too much coffee and other caffeine-based drinks
- do not take sleeping pills
Side effects of the treatment
- Bleeding is a possible side effect of the medications for pulmonary embolism treatment. The provider would give you the dose of anticoagulants or thrombolytics that fits the situation. Keeping people in the hospital allows them to monitor their condition.
What is the home treatment of Pulmonary embolism?
Home treatments are not recommended for initial treatment for pulmonary embolism. But it is important for preventing more clots from developing and leading to a deep vein thrombosis, which can lead to recurring pulmonary embolism. Measures that reduce the risk of developing a deep vein thrombosis include the following:
- Take anticoagulant medicines exactly as prescribed.
- Exercise. Keep blood moving in the legs by pointing the toes up toward the head so that the calves are stretched, then relaxing. Repeat. This exercise is especially important when you are sitting for long periods, for example, on long driving trips or airplane flights.
- Get up out of bed as soon as possible after an illness or/and surgery. It is very important to get moving as soon as people are able. If you can not get out of bed, do the leg exercises described above every hour to keep the blood moving through the legs.
- Quit smoking.
- Wear compression stockings to assist prevent leg deep vein thrombosis if you are at raised risk for this condition.
For more information on how to prevent or control clots from developing, see the topic Deep Vein Thrombosis.
Considerations for exercising after pulmonary embolism
If persons are currently recovering from a pulmonary embolism and wonder if the person can begin exercising, here are a few important considerations and suggestions:
- Get medical clearance: Before starting exercise, it is important to get clearance from a healthcare professional. the body requires time for healing, which may be hindered if you push yourself too hard.
- Listen to your body: If you are struggling with exercise, lower the intensity. This will ensure you are exercising at a pace that you can safely tolerate.
- Start slowly: It may be tempting to back to vigorous activity, but your body may need more time to recover before it can tolerate high volumes of physical activity.
- All activity counts: If you are only able to walk for a few minutes before feeling fatigued, don’t worry. Any movement is advantageous for your body, and it can add up.
- Be patient: the body just went through a stressful event and traumatic. Be patient and permit it to heal.
- Take your medication: If a healthcare professional prescribes medication, such as a blood thinner, it is important to take it. Exercise is not a stand-alone treatment for deep vein thrombosis or pulmonary embolisms.
- Wear compression socks: Compression socks assist to promote blood flow in the lower extremities. In a few cases, a healthcare professional may recommend wearing compression socks during or outside of physical activity.
What are the complications of a Pulmonary embolism?
A pulmonary embolism can be life-threatening. About one-third of individuals with not diagnosed and not treated pulmonary embolisms do not survive. When the condition is diagnosed and treated promptly, although, that number drops dramatically. Pulmonary embolisms also can lead to pulmonary hypertension, a condition in which the blood pressure in the lungs and on the right side of the heart is too high. When you have blockages in the arteries inside the lungs, the heart must work harder to push blood through those vessels. This raises blood pressure and eventually weakens the heart. In rare cases, small clots called emboli remain in the lungs and scarring develops in the pulmonary arteries over time. These restrict blood flow and result in chronic pulmonary hypertension.
A pulmonary embolism (PE) can lead to a lack of blood flow that leads to lung tissue damage. It can lead to low blood oxygen levels that can damage other organs in the body, too. A pulmonary embolism, specifically a large pulmonary embolism or many clots, can fast lead to serious life-threatening problems and, even death. Treatment of pulmonary embolism frequently involves anti-coagulation medicines or blood thinners. These medicines can put people at a risk for excessive bleeding if they thin the blood too much. Excessive bleeding is bleeding that won’t stop after people apply pressure for 10 minutes. another symptom of bleeding to watch for includes. the signs of bleeding in the digestive system:
- Bright red vomit or vomit that looks such as coffee grounds
- Bright red blood in the stool or black, tarry stools
- Abdominal pain
- Signs of bleeding in the brain:
- Severe headache
- Sudden vision changes
- Sudden loss of movement or feeling in the legs or arms
- Memory loss or confusion
If you have any of these, you require to get treatment right away.
How can I prevent a Pulmonary embolism?
Ways to prevent a pulmonary embolism include:
- Exercise regularly. If you can not walk around, move your arms, legs, and feet for a few minutes every hour. If you know you will require to sit or stand for long periods, wear compression stockings to encourage blood flow.
- Drink plenty of fluids, but limit the caffeine and alcohol.
- Do not use tobacco products.
- Avoid crossing your legs.
- Do not wear tight-fitting clothing.
- Lose weight if you have overweight.
- Elevate the feet for 30 minutes twice a day.
- Talk to the provider about reducing the risk factors, specifically if you or any of the family members have had a blood clot.
Deep vein thrombosis is the primary lead to pulmonary embolisms. As such, preventing deep vein thrombosis is the main way to prevent pulmonary embolism. If you are at risk of either condition, the doctor may recommend the following:
- Elevate the legs as often as possible and raise the bottom of the bed during sleep.
- Maintain a moderate weight.
- Move and get physical activity, including walking very soon after the surgery.
- Stop smoking.
- Take the anticoagulant for surgery, heart attack, stroke, or cancer complications.
- Use pneumatic compression during periods of immobility.
- Wear compression stockings.
For prolonged sitting or travel, it can be useful to drink plenty of fluids, wear support stockings, take frequent standing or walking breaks, and practice calf exercises and ankle exercises in the seat. For individuals who are at higher risk for deep vein thrombosis — such as following orthopedic surgery —the doctors may also recommend taking aspirin when traveling by airplane. The provider may also recommend an interventional procedure in which a healthcare provider places a filter inside the body’s largest vein. A vena cava filter traps clots before they enter the lungs. Preventing clots in the deep veins in the legs will assist prevent pulmonary embolisms. For this cause, most hospitals are aggressive about taking measures to stop blood clots, including:
- Blood thinners (anticoagulants). These medicines are often given to individuals at risk of clots before and after surgery. Also, they are often given to individuals admitted to the hospital with certain medical conditions, such as heart attack, stroke, or complications of cancer.
- Compression stockings. Compression stockings steadily squeeze the legs, assisting veins and leg muscles to move blood more efficiently. They offer a safe, simple, and inexpensive way to maintain blood from pooling in the legs during and after surgery.
- Leg elevation. Elevating the legs when possible and during the night can be very effective. Increase the base of a bed by 4 to 6 inches (10 to 15 cm) with blocks or books.
- Physical activity. Moving as soon as possible after surgery can assist prevent pulmonary embolism and hasten recovery overall. This is one of the main reasons the nurse may push you to get up, even on the day of surgery, and walk despite the pain at the site of the surgical incision.
- Pneumatic compression. This type of treatment utilizes thigh-high or calf-high cuffs that automatically inflate with air and deflate every few minutes. This massages and squeezes the veins in the legs and improves blood flow.
Stretching during trips
- If peoples are on a long flight, try to walk around every few hours. If you can not stand up, flex the ankles by pulling the toes toward you.
- Here are another stretch people can try to do while seated:
- Pull the leg up toward the chest with one hand.
- Maintain the bottom of that leg with the other hand.
- Maintain this pose for 15 seconds, and then try it with the other leg.
- Do this up to ten times every hour.
- If you are driving a long distance, stop per hour and stretch your legs.
- Also, be sure to drink extra fluids to assist you to stay hydrated.
Lifestyle changes
- Other steps you can take include:
- Maintain a healthy weight.
- If you plan to take hormones, like birth control or replacement therapy, talk to the doctor about the risk of blood clots.
- If you have other health issues, like diabetes or heart failure, take the meds, watch what you eat, and talk to the doctor about any changes.
- Also, talk to the doctor if you have a history of kidney disease or certain autoimmune diseases, or a family history of blood clots
- If you smoke, quit.
- In life-threatening cases of pulmonary embolism, the doctor may decide to give you drugs called thrombolytics to break up the clot. It might even need to be carried out or broken up with surgery, though this is rare.
Prevention while traveling
The risk of blood clots developing while traveling is low but raises as long-haul travel increases. If people have risk factors for blood clots and people are concerned about travel, talk with the healthcare provider.
The provider might suggest the following to assist prevent blood clots during travel:
- Drink plenty of fluids. Water is the best liquid for controlling dehydration, which can contribute to the development of blood clots. and avoid drinking alcohol, which contributes to fluid loss.
- Take a break from sitting. Move around an airplane cabin once an hour or so. If you are driving, stop every so frequently and walk around the car a couple of times. Do a few deep knee bends.
- Move-in the seat. Bend and make circular movements with the ankles and raise the toes up and down every 15 to 30 minutes.
- Wear support stockings. The provider may recommend these to assist promote circulation and fluid movement in the legs. A compression stocking is available in a range of stylish colors and textures. There are even devices, called stocking butlers, to assist you to put on the stockings.
Can pulmonary embolism cause death? Survival rate
- Patient survival depends upon:
- the underlying health of a patient,
- the clot burden of a pulmonary embolus,
- the effect has on the heart and its ability to pump blood to the organs of a body,
- vital sign stability,
- the lead to the pulmonary embolus, and
- An ability for the diagnosis to be made and early initiation of treatment.
- Without treatment, a pulmonary embolism is a very serious condition that could lead to permanent illness or death. With treatment, the prognosis depends on the size of the blood clot and blockages, as well as the overall health and how well the heart can pump blood.
- The exact amount of time that it takes to recover from a pulmonary embolism can vary from person to person. Many people can completely recover and return to their normal level of activity after many weeks or months. Some of the symptoms may ease as people receive treatment and the body heals.
How do I take care of myself?
- You will require to take a blood thinner for three to six months or longer. Do not stop taking this unless the provider instructs you to. If you are taking a blood thinner, do not do things that have a high risk of an injury that could make you bleed.
- Be sure you discuss and understand the follow-up care with the healthcare provider. Follow their recommendations to decrease the risk of another pulmonary embolism.
- Keep all appointments with the provider and the laboratory so they can monitor the response to prescribed treatments.
When should people go to the ER?
Get immediate treatment if people have pulmonary embolism symptoms. Pulmonary embolism common symptoms may include:
- Sudden shortness of breath. This symptom generally appears suddenly. Trouble catching the breath occurs even when resting and gets worse with physical activity. whether you have been active or at rest.
- Chest pain. people may feel like people are having a heart attack. The pain is usually sharp and felt when people breathe in deeply. The pain can stop people from being able to take a deep breath. people also may feel it when people cough, bend or lean over. Not explained sharp pain in the chest, arm, shoulder, neck, or jaw. The pain may also be the same as the symptoms of a heart attack.
- Fainting. people may pass out if the heart rate or blood pressure drops suddenly. This is called syncope.
- Cough with or without bloody mucus.
- Pale, clammy, or bluish skin.
- Rapid heartbeat (pulse).
- Excessive sweating.
- In a few cases, feeling anxious, lightheaded, faint, or pass out.
- Wheezing.
Other symptoms that can happen with pulmonary embolism include:
- A cough that may include blood-streaked mucus or bloody
- Rapid or irregular heartbeat
- Lightheadedness or dizziness
- Excessive sweating
- Fever
- Leg pain or swelling, or both, generally in the back of the lower leg
- Clammy or discolored skin, named cyanosis
Key points about pulmonary embolisms
- A pulmonary embolism (PE) is a blood clot that develops in the blood vessel elsewhere in the body (often the leg), travels to an artery in the lung, and suddenly forms a blockage of the artery.
- Abnormal or not normal blood clots could form due to problems like “sluggish” blood flow through the veins, an abnormality in clot-forming factors, and/or an injury to the blood vessel wall.
- A wide variety of conditions and risk factors have been linked to pulmonary embolism.
- Sudden shortness of breath is the most common symptom of pulmonary embolism.
- Pulmonary embolism is often difficult to diagnose because the signs and symptoms of pulmonary embolism are a lot like those of many other conditions and diseases. Imaging tests and blood tests are used to look for a pulmonary embolism.
- An important aspect of treating pulmonary embolism is preventing additional clots. Medicines, filters to keep clots from getting to the lungs, and surgery are used to treat pulmonary embolisms.
- A pulmonary embolism, particularly a large pulmonary embolism or many clots, can quickly cause serious life-threatening consequences and death.
Takeaway
- A pulmonary embolism happens when a blood clot reaches the lungs. These blood clots often come from deep vein thrombosis, which can result from damage to bone and muscle or long periods of inactivity. Many times the exact cause of a deep vein thrombosis or pulmonary embolism is unknown despite a thorough evaluation.
- pulmonary embolism can be very dangerous, so it’s important to contact a medical professional if you’re experiencing symptoms such as chest pain, spitting up blood, and fainting.
- A doctor will generally prescribe medications that thin the blood and, in certain cases, use medications that break up blood clots. Minimally invasive interventional procedures and surgery may be required in a few instances.
Summary
- A pulmonary embolism can be a life-threatening condition that most often results from deep vein thrombosis. It is possible to have a pulmonary embolism and not have symptoms involving the lungs. A few people only have deep vein thrombosis symptoms.
- If people have a deep vein thrombosis, doctors will use diagnostic testing to find out if people also have a pulmonary embolism. If so, the severity of the pulmonary embolism will guide treatment. A severity will also give the doctors information about the prognosis.
Outlook(Prognosis)
- With effective and timely treatment, most individuals who experience a pulmonary embolism can make a full recovery.
- The condition carries a high risk of fatality. although, early treatment can dramatically reduce this risk.
- The period of highest risk is in the hours after the embolism first happens. The outlook is also worse if the embolism was led to by an underlying condition, such as a type of cancer.
- Although, most individuals with pulmonary embolisms can make a full recovery.
How well the individual recovers from a pulmonary embolus could be hard to predict. It usually depends on:
- What caused a problem in the first place (for example, cancer, major surgery, or an injury)
- The size of a blood clot in the lungs
- If the blood clot dissolves over time
- A few people can develop long-term heart and lung problems.
- Death is possible in individuals with a severe pulmonary embolism.
What is people’s plan if people have a pulmonary embolism?
If people have had a pulmonary embolism, the following options may help decrease the risk of a blood clot forming in the future:
- Compression stockings – knee-high socks that apply a firm pressure about the legs when worn and help the blood circulate (move) in the legs
- Exercise – the regular movement of the arms and legs helps keep the blood flowing and prevent it from ‘pooling’ in the lower legs
- Hydration – drinking plenty of fluids prevents you from becoming dehydrated (which can thicken the blood and raise the risk for blood clots)
- Maintain a healthy weight – if people are overweight or obese, talk to the doctor about a referral to a registered nutritionist or dietitian
- Medication – such as blood thinners (known as anticoagulants) will help prevent the blood from forming clots
- Smoking – if people smoke, talk with the doctor about quitting
- Stretches – regular stretches and leg movement when on long trips (such as flights) can help keep the blood circulating.
DISCLAIMER:
- This article is intended or purposeful for your general informational purposes only and does not address particular circumstances. it is not a substitute for professional advice(or guidance) or help( or assistance) and should not be relied on to make decisions of any kind. A few or any actions you take upon the information presented in this article are strictly at your own risk and responsibility.
FAQs
What is the main cause of pulmonary embolism?
Generally, a pulmonary embolism is caused by a blood clot traveling up from one of the deep veins in your body, usually in the leg. This kind of blood clot is named deep vein thrombosis (DVT). In a few cases, the blood clot happens because of a change in the physical condition, such as pregnancy or recent surgery.
Can you survive a pulmonary embolism?
While a pulmonary embolism can be life-threatening, most patients survive and require to learn how to live with the risk of recurrence. the healthcare provider might prescribe anticoagulants, or blood thinners, which may be needed for as little as three months but can be needed for the remainder of a patient’s life.
What are the four common signs and symptoms of pulmonary embolism?
What are the symptoms of a pulmonary embolism?
Sudden shortness of breath (most common)
Chest pain (usually worse with breathing)
A feeling of anxiety.
A feeling of dizziness, lightheadedness, or fainting.
Irregular heartbeat.
Palpitations (heart racing)
Coughing and/or coughing up blood.
Sweating.
What are the 3 types of pulmonary embolisms?
Based on the location of the clot in the pulmonary artery following terms are used A) saddle pulmonary embolism(large clot into a main pulmonary artery), B) lobar pulmonary embolism(into the big branch of the pulmonary artery), or C) distal pulmonary embolism(into small branches of the pulmonary artery).
How many early warning signs of pulmonary embolisms?
Fainting.
A cough that might include bloody or blood-streaked mucus.
Rapid or irregular heartbeat.
Lightheadedness or dizziness.
Excessive sweating.
Fever.
Leg pain or swelling, or both, commonly in the back of the lower leg.
Clammy or discolored skin is called cyanosis.
How do you detect pulmonary embolism?
Pulmonary angiogram. This test provides a clear image of blood flow in the arteries of the lungs. that is the most accurate way to diagnose a pulmonary embolism.
Is pulmonary embolism very painful?
The main symptoms of a pulmonary embolism include chest pain that might be any of the following: Under the breastbone or on one side. Sharp or stabbing. Burning, aching, or the dull, heavy sensation.
What is the best treatment for pulmonary embolism?
The main treatment for pulmonary embolism is named an anticoagulant. This is a drug that causes chemical changes in the blood to stop it from clotting easily. This drug will stop the clot from getting larger while the body slowly absorbs it. It also decreases the risk of further clots developing.
How long can a people live with a pulmonary embolism?
Recent findings: A death rate after pulmonary embolism is less than 5% during 3-6 months of anticoagulant treatment, provided that the patient is hemodynamically stable and free of major underlying disease. The rate of recurrent thromboembolism is less than 5% on the anticoagulant therapy, reaching 30% after 10 years.
How can people prevent pulmonary embolism?
What can people do to avoid getting a pulmonary embolism?
stopping smoking – if people smoke, quitting is the best thing you can do for your health.
getting regular exercise.
not sitting still for a long time – such as when watching TV or using a computer.
avoid becoming dehydrated.
What organs does pulmonary embolism affect?
A pulmonary embolism (PE) can lead to a lack of blood flow that leads to lung tissue damage. It can lead to low blood oxygen levels that can damage other organs in the body, too.
Who is most at risk for pulmonary embolism?
Pulmonary embolism (PE) happens equally in women and men. The risk increases with age. For every ten years after age 60, the risk of having Pulmonary embolism doubles. Certain inherited conditions, such as factor V Leiden, raise the risk of blood clotting and Pulmonary embolism.
What increases the risk of pulmonary embolism?
8 things that increase the risk for a Pulmonary embolism
Medical conditions: including high blood pressure, COPD(Chronic obstructive pulmonary disease), stroke, cancer, and inflammatory bowel disease. Vein disorders: including varicose veins and swelling in the leg. Smoking: restricts blood flow and contributes to the “hardening of the arteries”.
Can ECG detect pulmonary embolism?
While an ECG cannot assist diagnose a pulmonary embolism, it can reveal problems in the heart that could suggest a pulmonary embolism, specifically if a patient has other symptoms. In certain, it could show problems with the right ventricle of the heart.
What age does pulmonary embolism start?
Pulmonary embolism happens most frequently in the age group 70 to 79 years. The most common factors that lead to pulmonary embolism are the state after surgery and a history of deep vein thrombosis.
Does pulmonary embolism come on suddenly?
A pulmonary embolism is a sudden blockage or stoppage of an artery in the lungs. It generally happens when a blood clot breaks loose and travels through the bloodstream to the lungs.
When should you suspect pulmonary embolism?
However the signs and the symptoms of pulmonary embolism are nonspecific, there are some “classical” clinical signs, which increase suspicion of pulmonary embolism. The circulatory collapse caused by a massive pulmonary embolism presents as shock or syncope. It is sometimes accompanied by severe dyspnoea and chest pain and there might be signs of acute right heart failure.
Can a blood test detect a pulmonary embolism?
D-dimer. The doctor will order a D-dimer blood test to assist diagnose or rule out the presence of a pulmonary embolism. A D-dimer test measures the levels of the substance those are produced in the bloodstream when a blood clot breaks down.
Are there stages of pulmonary embolism?
A new rule classifies patients who have pulmonary embolism into five disease stages that reveal a raised risk of death or another adverse outcome.
What food causes pulmonary embolism?
No specific food is known to directly decrease or cause blood clots, DVT( deep vein thrombosis), or pulmonary embolism. Factors that may increase the risk include physical inactivity, surgery or injuries, and smoking. It is best to focus on maintaining a well-rounded, healthy lifestyle, which may help prevent pulmonary embolisms.
Do blood thinners dissolve pulmonary embolism?
Blood thinners are also used to assist prevent clots after a stroke or pulmonary embolism (when a blood clot travels to an artery in the lungs). Blood thinners do not dissolve the clot, but they can stop it from getting bigger and keep new ones from forming. That gives the body time to break up the clot.
Can stress cause pulmonary embolism?
Effect of Stress on Blood Vessels
But anxiety can also raise blood pressure, putting additional stress on the blood vessel walls, making them stiffer, and reducing the amount of blood that flows through the body. Combined these forces can lead to serious blood clots that can lead to blockages in the heart and the lungs.
Will oxygen saturation be low with pulmonary embolism?
If people have a pulmonary embolism, their blood oxygen level will be lower than normal. A pulse oximeter device is usually clipped onto the finger and measures the blood oxygen saturation level using red and infrared light through the tissue in the finger. A blood oxygen saturation level of less than 90 percent is abnormal.
What is the position best for people with a pulmonary embolism?
Immediately place a person in the left lateral decubitus (Durant maneuver) and the Trendelenburg position. This assists to prevent air from traveling through the right side of a heart into the pulmonary arteries, leading to right ventricular outflow obstruction (airlock).
What is the most common source of embolism?
A common source for an embolus is from areas of hardening (atherosclerosis leading to plaque) in the aorta and other large blood vessels. This clot could break loose and flow down to the legs and the feet.
Can a chest x-ray show a pulmonary embolism?
A chest x-ray cannot prove that pulmonary embolism is present or absent because clots do not show up on the x-ray. Nevertheless, a chest x-ray is a useful test in the evaluation of pulmonary embolism because it can find other diseases, such as pneumonia or fluid in the lungs, that may explain a person’s symptoms.
What is the recovery rate for pulmonary embolism?
Most patients with pulmonary embolisms make a full recovery within weeks to months after starting treatment and do not have any long-term effects. Roughly 33 percent of individuals who have a blood clot are at an increased risk of having another within ten years, according to the Centers for Disease Control and Prevention (CDC).
Is walking good for pulmonary embolism?
It is generally recommended to start with a few minutes of walking each day and gradually raise the time as you become stronger. As long as it is done safely, exercising after a pulmonary embolism may assist to prevent another one from occurring and help build back strength.
What is the heart rate when people have a pulmonary embolism?
Electrocardiogram: Electrocardiogram of the patient with pulmonary embolism showing sinus tachycardia of approximately 150 beats every minute and right bundle branch block. In most cases, anticoagulant therapy or treatment is the mainstay of the treatment. Acutely, supportive treatments, such as oxygen or/and analgesia, are often needed.
Why is hemoglobin low in pulmonary embolism?
found that patients with pulmonary embolisms had significantly lower mean hemoglobin levels than gender and age-matched controls. They proposed that this was due to reduced secretion of anti-thrombotic mediators, initiated by low blood viscosity in anemic states, resulting in raised clotting.
Can you live a normal life with a pulmonary embolism?
While a pulmonary embolism can be life-threatening, most patients survive and require to learn how to live with the risk of recurrence. The healthcare provider may prescribe anticoagulants, or blood thinners, which may be required for as little as three months but can be needed for the remainder of a patient’s life.
What kills in pulmonary embolism?
Up to one-third of patients with a pulmonary embolism (PE) would die of cardiac arrest before the dangerous clot is identified in a hospital or/and emergency department. A big cause for the high mortality rate is that the symptoms of pulmonary embolism are generally non-specific until it progresses to an emergency.
Where does a pulmonary embolism begin?
A pulmonary embolus is most frequently caused by a blood clot that develops in a vein outside the lungs. The most common blood clot is one in a deep vein of the thigh or the pelvis (hip area). This type of clot is named deep vein thrombosis (DVT). A blood clot breaks off and travels to the lungs where it lodges.
What bacteria causes pulmonary embolism?
Septic pulmonary embolism (SPE) is an uncommon but serious complication resulting from an infection of the blood. Gram-positive cocci, including methicillin-susceptible Staphylococcus aureus and methicillin-resistant Staphylococcus aureus, are the most common causative organisms of Septic pulmonary embolism.
How long can you live with a lung embolism?
Recent findings: The death rate after pulmonary embolism is less than 5% during 3 to 6 months of anticoagulant treatment, provided that the patient is hemodynamically stable and free of major underlying disease. The rate of recurrent thromboembolism is less than 5% on anticoagulant therapy, reaching 30% after ten years.
When should you suspect pulmonary embolism?
However the signs and symptoms of pulmonary embolism are nonspecific, there are some “classical” clinical signs, which raise suspicion of pulmonary embolism. The circulatory collapse caused by a massive pulmonary embolism presents as shock or syncope. It is a few times accompanied by severe dyspnoea and chest pain and there may be signs of acute right heart failure.
What can people do to avoid getting a pulmonary embolism?
stopping smoking – if people smoke, quitting is the best thing people can do for their health.
getting regular exercise.
not sitting still for a long time – such as when watching TV or using a computer.
avoid becoming dehydrated.
Can a chest x-ray show a pulmonary embolism?
A chest x-ray cannot prove that pulmonary embolism is present or absent because clots do not show up on the x-ray. Nevertheless, a chest x-ray is a useful test in the evaluation of pulmonary embolism because it can find other diseases, such as pneumonia or fluid in the lungs, that may explain a person’s symptoms.
Can a stethoscope detect pulmonary embolism?
In pulmonary embolism, the chest examination is usually normal, but if there is some associated inflammation on the surface of the lung (the pleura), a rub may be heard (pleura inflammation may lead to friction, which can be heard with a stethoscope).
Does pulmonary embolism cause low BP?
The Symptoms of pulmonary embolism include difficulty breathing, chest pain on inspiration, and palpitations. Clinical signs include low blood oxygen saturation and cyanosis, rapid or fast breathing, and a rapid heart rate. Severe cases of pulmonary embolism could lead to collapse, abnormally low blood pressure, and sudden death.
Can a person live a normal life after a pulmonary embolism?
The exact amount of time that it takes to recover from a pulmonary embolism can vary from person to person. Many people can completely recover and return to their normal level of activity after many weeks or months. Some of the symptoms may ease as people receive treatment and the body heals.
What can people expect if people have a pulmonary embolism?
Without treatment, a pulmonary embolism is a very serious condition that could lead to permanent illness or death. With treatment, the prognosis depends on the size of the blood clot and blockages, as well as the overall health and how well the heart can pump blood.
Will a pulmonary embolism go away?
It can take months or years for the pulmonary embolism to go away completely. Repeated pulmonary embolism or a very large pulmonary embolism can lead to pulmonary hypertension in a few people.
When should people see my healthcare provider?
See the healthcare provider for follow-up appointments. While taking a blood thinner, contact the provider if people have black poop, a bad headache, or a bruise that is getting bigger. This could mean that people are bleeding.


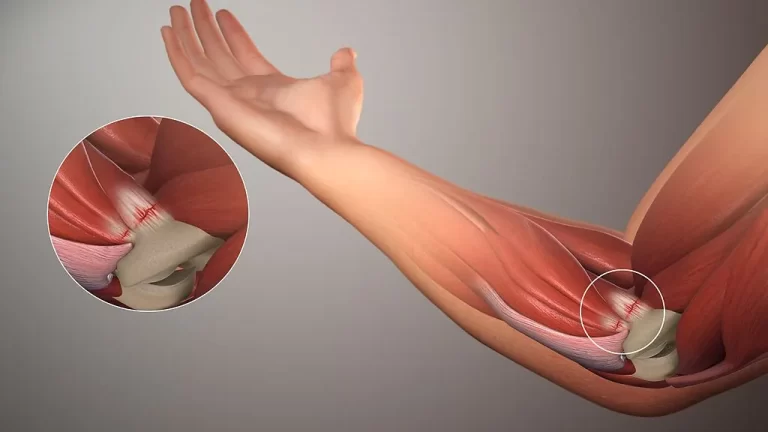



5 Comments