Tetralogy of Fallot
INTRODUCTION
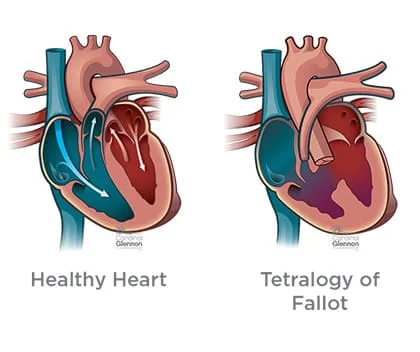
Tetralogy of Fallot (teh-TRAL-uh-jee of fuh-LOW) is a rare condition caused by a combination of four heart defects that are present at birth (congenital).
These defects, which affect the structure of the heart, cause oxygen-poor blood to flow out of the heart and to the rest of the body. Infants and children with tetralogy of Fallot usually have blue-tinged skin because their blood doesn’t carry enough oxygen.
Tetralogy of Fallot is often diagnosed during infancy or soon after. However, tetralogy of Fallot might not be detected until later in life in some adults, depending on the severity of the defects and symptoms.
With early diagnosis followed by appropriate surgical treatment, most children and adults who have tetralogy of Fallot live relatively normal lives, though they’ll need regular medical care throughout life and might have restrictions on exercise.
SYMPTOMS in Tetralogy of Fallot
Tetralogy of Fallot symptoms vary, depending on the extent of obstruction of blood flow out of the right ventricle and into the lungs. Signs and symptoms may include:
A bluish coloration of the skin caused by blood low in oxygen (cyanosis)
Shortness of breath and rapid breathing, especially during feeding or exercise
Loss of consciousness (fainting)
Clubbing of fingers and toes — an abnormal, rounded shape of the nail bed
Poor weight gain
Tiring easily during play or exercise
Irritability
Prolonged crying
A heart murmur
Tet spells
Sometimes, babies who have tetralogy of Fallot will suddenly develop deep blue skin, nails and lips after crying or feeding, or when agitated.
These episodes are called tet spells and are caused by a rapid drop in the amount of oxygen in the blood. Tet spells are most common in young infants, around 2 to 4 months old. Toddlers or older children might instinctively squat when they’re short of breath. Squatting increases blood flow to the lungs.
Seek medical help if you notice that your baby has the following symptoms:
- Difficulty breathing
- Bluish discoloration of the skin
- Passing out or seizures
- Weakness
- Unusual irritability
- If your baby becomes blue (cyanotic), place your baby on his or her side and pull your baby’s knees up to his or her chest. This helps increase blood flow to the lungs. Call 911 or your local emergency number immediately.
CAUSES of Tetralogy of Fallot

Tetralogy of Fallot occurs during fetal growth, when the baby’s heart is developing. While factors such as poor maternal nutrition, viral illness or genetic disorders might increase the risk of this condition, in most cases the cause of tetralogy of Fallot is unknown.
The four abnormalities that make up the tetralogy of Fallot include:
- PULMONARY VALVE STENOSIS– Pulmonary valve stenosis is a narrowing of the pulmonary valve — the valve that separates the lower right chamber of the heart (right ventricle) from the main blood vessel leading to the lungs (pulmonary artery).
Narrowing (constriction) of the pulmonary valve reduces blood flow to the lungs. The narrowing might also affect the muscle beneath the pulmonary valve. In some severe cases, the pulmonary valve doesn’t form properly (pulmonary atresia) and causes reduced blood flow to the lungs.
- VENTRICULAR SEPTAL DEFECT- A ventricular septal defect is a hole (defect) in the wall (septum) that separates the two lower chambers of the heart -the left and right ventricles. The hole allows deoxygenated blood in the right ventricle — blood that has circulated through the body and is returning to the lungs to replenish its oxygen supply — to flow into the left ventricle and mix with oxygenated blood fresh from the lungs.
Blood from the left ventricle also flows back to the right ventricle in an inefficient manner. This ability for blood to flow through the ventricular septal defect reduces the supply of oxygenated blood to the body and eventually can weaken the heart.
- OVERRIDING AORTA– Normally the aorta — the main artery leading out to the body — branches off the left ventricle. In tetralogy of Fallot, the aorta is shifted slightly to the right and lies directly above the ventricular septal defect.
In this position the aorta receives blood from both the right and left ventricles, mixing the oxygen-poor blood from the right ventricle with the oxygen-rich blood from the left ventricle.
- RIGHT VENTRICULAR HYPERTROPHY- When the heart’s pumping action is overworked, it causes the muscular wall of the right ventricle to thicken. Over time this might cause the heart to stiffen, become weak and eventually fail.
Some children or adults who have tetralogy of Fallot may have other heart defects, such as a hole between the heart’s upper chambers (atrial septal defect), a right aortic arch or abnormalities of the coronary arteries.
RISK FACTOR
While the exact cause of tetralogy of Fallot is unknown, various factors might increase the risk of a baby being born with this condition. These risk factors include:
- A viral illness during pregnancy, such as rubella (German measles)
- Alcoholism during pregnancy
- Poor nutrition during pregnancy
- A mother older than age 40
- A parent who has tetralogy of Fallot
- The presence of Down syndrome or DiGeorge syndrome
COMPLICATIONS
All babies who have tetralogy of Fallot need corrective surgery. Without treatment, your baby might not grow and develop properly.
Your baby may also be at an increased risk of serious complications, such as infective endocarditis — an infection of the inner lining of the heart or heart valve caused by a bacterial infection.
Untreated cases of tetralogy of Fallot usually develop severe complications over time, which might result in death or disability by early adulthood.
PHYSIOTHERAPY TREATMENT
PRE-OPERATIVE – Most infants with TOF will receive thoracic surgery to correct the associated abnormalities. The most important physical therapy intervention pre-operative for the patient and family is education. Many institutes are using a method of education that describes a pre-operative program that helps to decrease post-operative complications. Many institutions use a doll to explain to children about the tubes and how to care for them.
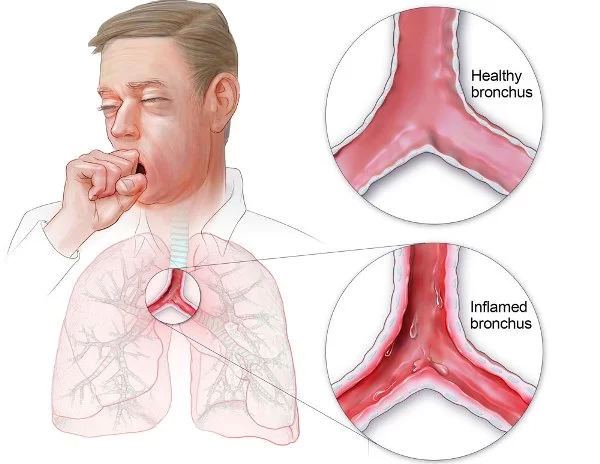
POST-OPERATIVE– Pulmonary function is a main area of concentration after thoracic surgery. The interventions vary with age but the general goal is the same, to mobilize secretions, increase aeration and increase general mobility. Atelectasis is a concern after thoracic surgery and is caused by the slowed mucous transport, altered breathing patterns, prolonged positioning in supine and diaphragmatic dysfunction in early post-operative period. The yawn maneuver and prolonged inspiration to increase inflation are ways to prevent atelectasis. The incentive spirometry is an effective tool for preventing atelectasis in the pediatric population. Other ways that can be more fun for children are activities such as blowing bubbles or blowing on a windmill. There are expiratory maneuvers but the children typically take a large breath before blowing, thus they become inspiratory maneuvers also.
Segmental expansion techniques are effective to increase segmental aeration. These techniques are performed by placing your hand over whichever segment of the lung is not effectively inflating and allowing your hand to move with the respiratory cycle. Gentle pressure may be applied to the chest at the end of the expiratory phase, just before the inhalation phase. This elicits a stretch reflex that facilitates air flow to that particular segment.
Percussion and vibration may be performed in conjunction with segmental expansion. Percussion is the rhythmic clapping with cupped hands over the involved lung segment performed throughout the respiratory cycle, with the goal of mechanically dislodging pulmonary secretions. Vibration is performed by creating a fine oscillating movement of the hands on the chest wall just before expiration begins and throughout the expiration phase. If the child does not tolerate percussion and vibration, placing the patient in side lying and gently rocking back and forth may stimulate expansion, secretion motion and relaxation. This technique is affective if the child is upset and may decrease respiratory rate.
Positioning may be useful for patients, but certain positions may be contraindicated post thoracic surgery. Check with the MD or nurse before using positioning to make sure that it is safe for the child.
POSTURAL DRAINAGE :
If the child is intubated suctioning may be used to remove secretions from the airways, however children with cyanotic defects (such as TOF) tend to desaturate during suctioning and it is very important to hyperventilate these patients before and after suctioning and to monitor oxygen levels.
Coughing is an effective way to mobilize secretions if the patient is able and willing to cough. A teddy bear or pillow can be used by the child to self-splint the incision. Have the child squeeze the stuffed animal against their chest to decrease pain.
Range of motion (ROM) exercises should be initiated as soon as possible after surgery. ROM exercises are extremely important with thoracic surgery because this type of incision tends to produce more guarding. Child position should be changed regularly to avoid a pooling of secretions in the dependent part of the lungs and regular position changes reduce the risk of fevers after surgery. Ambulation should be implemented as soon as possible to decrease both pulmonary and circulatory complications. As soon as atrial lines and groin lines are removed, patients should begin to ambulate, even if only 5-10 ft.
DIFFERENTIAL DIAGNOSIS
Any other cyanotic heart defects, such as, pulmonary stenosis, transposed arterial trunks, common arterial trunk and tricuspid atresia. Patients with heart murmurs will also be tests for persistent pulmonary hypertension.


Respected Sir/Mam,
Please share something about Vestibular Rehabilitation.