Enthesitis-Related Arthritis
What is Enthesitis-Related Arthritis?
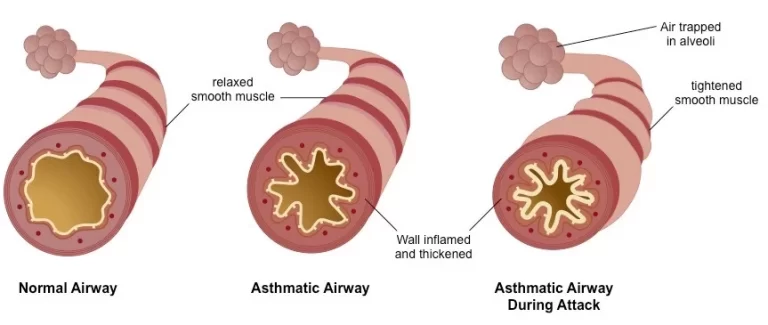
Enthesitis-related arthritis (ERA) is one kind of arthritis. People with ERA not only include joint swelling or inflammation (arthritis) but even have enthesitis. Enthesitis is swelling or inflammation of the entheses, the connective tissue where tendons or ligaments connect to bone.
In ERA, like other kinds of youth arthritis, there is no infection. Rather, the immune system is illogical and strikes the cells and tissues in the body’s connective tissues involving the tendons, joints, and entheses. This leads to swelling, redness, warmth, pain, stiffness, or loss of motion in the connective tissue. For this purpose, ERA is known as an autoimmune disorder.
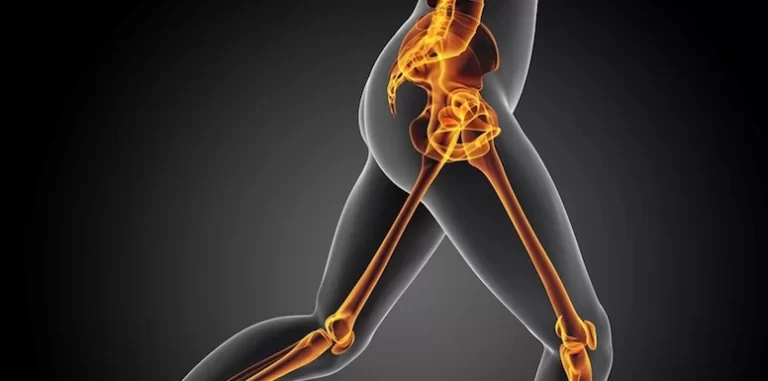
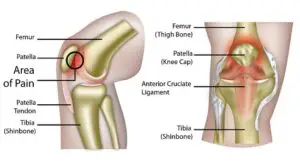
Frequently, ERA begins as arthritis in the big joints of the lower extremities. This involves the hips and knees. It is familiar to have pain and sense tenderness where tendons or ligaments connect to bones. Familiar areas for inflammation are:
- The heel
- Top and base of the kneecap (patella)
- Ball of the foot
- The bottom of the foot at the heel
- Mid-foot area
- Arthritis is not familiar in the elbows and wrists, but it does happen in the shoulders. People with ERA may have inflammation in other regions of their bodies. Eye inflammation (known as anterior uveitis) happens in almost half of people.
Uveitis with ERA induces pain and redness. Redness and ache are not familiar in other kinds of arthritis that involve the eyes.
Synonyms
juvenile rheumatoid arthritis — enthesitis-related
juvenile chronic arthritis — enthesitis-related
enthesitis-related arthritis (ERA)
Epidemiology
Enthesitis-related arthritis (ERA) accounts for about 10 to 19 percent of children organized with juvenile idiopathic arthritis (JIA). The mean age at diagnosis for kids with ERA is about 12 years. An ERA is more familiar in men, who make up about 60 to 80 percent of patients. It is calculated that about 8 to 11 percent of grown-ups with ankylosing spondylitis (AS) had the onset of their condition in childhood
Symptoms of enthesitis-related arthritis
- Inflammatory Spinal Pain. Back pain that occurs before age 45, is slowly in beginning and brings better with activity and more harmful with rest. This runs along with morning immobility. It must happen for at least three-3 months.
- Synovitis. Swelling of the synovium, or the coating of cells striping the joint or junction space. This shows symptoms of arthritis. This frequently affects the lower limbs or shoulders in SpA.
- Positive Family History. Parents, grandparents, sisters and brothers, uncles, aunts, or cousins with any of these: AS, acute uveitis, psoriatic arthritis, reactive arthritis, or inflammatory bowel disorder with arthritis.
- Psoriasis. Psoriasis is a skin condition that causes a scaly, pink-in-color rash in patches on the face or scalp. It can be seen in numerous areas of the body.
- Inflammatory Bowel Disease. Crohn’s condition or ulcerative colitis is interpreted by a doctor or physician.
- Buttock Pain. Past or present pain that alternates between either buttocks.
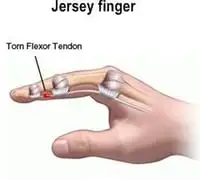
- Enthesopathy. Past or present pain, or supposing tender, where the Achilles tendon or plantar fascia inserts on the bone (back of the heel or bottom heel). Enthesis is the wide term for where a tendon or joint or junction or capsule inserts on bone. Enthesitis guides to swelling at these locations.
- Diarrhea. Sudden onset of loose water-like stool within one month before the onset of arthritis.
- Sacroiliitis. Inflammation in one or both sacroiliac joints or junctions. This inflammation can generate pain, stiffness, tenderness, and restriction of movement in this joint or junction. Inflammation can be noticed on MRI or CT in early phases and on X-rays at later phases.
Others:
Physical exercise may worsen symptoms of enthesitis. Someone may have a problem jogging, running, or climbing stairs because of the pain.
Long enthesitis may lead to permanent modifications that involve body motion and function. One of these likely transformations is ossification, which is the construction of new bone tissue. An instance is a heel spur, which is the extra bone that extends from the heel.
Another likely change is fibrosis, a situation in which delicate body tissues evolve thickened and scarred, involving motion.
Causes of enthesitis-related arthritis
Enthesitis can happen as a consequence of injury, overuse, or underlying condition.
Overuse
Enthesitis can evolve as an outcome of prolonged pressure on the joints or junctions. This can happen as an outcome of the following:
- having overweight or obesity
- playing sports
- performing movements that implicate repetitive motions
- Injury
- Enthesitis can also evolve after injury to the ligaments, tendons, and other connective tissue. Examples of these injuries contain:
Achilles tendonitis:
Hyper use damage of the Achilles tendon, which attaches to the calf muscle and heel bone.
Rotator cuff syndrome:
Damage or degenerative disease involving the rotator cuff, which is a group of muscles and tendons that keep the upper arm bone inside the shoulder socket.
Plantar fasciitis:
Inflammation of the plantar fascia, which is a ligament that attaches the heel bone to the toes.
Bursitis of the hip:
Inflammation of the fluid-filled sacs or bursa that soften the hip joints or junctions.
Disease
Enthesitis can occur because of underlying inflammatory conditions and autoimmune diseases, where the resistant system strikes tissues within the joint or junction. Examples involve:
- Psoriatic arthritis: A type of arthritis that may involve patients with the skin disease psoriasis.
- Gout: A variety of arthritis in which a buildup of uric acid in the body aggravate sudden and extreme joint or junction pain.
- Juvenile idiopathic arthritis: Arthritis that involves juveniles and teenagers.
- Ankylosing spondylitis: An inflammatory disease that causes the vertebrae of the spine to connect jointly.
- Doctors or physicians do not understand specifically how many patients with the above conditions will go on to create enthesitis.
Diagnosis
To diagnose enthesitis, a doctor or physician will ask about a patient’s symptoms and medical record, involving whether someone has a family record of the disease. They will also inspect the impacted locations for signs of swelling and tenderness.
In some patients, a doctor or physician may order medical examinations to rule out other diseases like rheumatoid arthritis. Tests may involve:
- blood tests
- ultrasound scans
- MRI scans
- Depending on the outcomes of the medical examinations, the doctor or physician may guide the patient to a rheumatologist for a more in-depth analysis.
Treatment of enthesitis-related arthritis
Medical Treatment
The treatment for enthesitis relies on several factors, involving:
- the cause of the disease
- the symptoms of individual incidents
- how long has the individual felt symptoms
- One likely treatment choice is nonsteroidal anti-inflammatory medications (NSAIDs). Medications like ibuprofen and piroxicam can assist to relieve inflammation and pain.
Another treatment choice is steroids. Medications that can assist to relieve inflammation and relieve joint or junction aches and stiffness. If enthesitis involves a precise joint or junction, a doctor or physician may suggest a corticosteroid injection into the joint or junction to reduce symptoms.
A rheumatologist may suggest biological medicines to treat enthesitis resulting from autoimmune arthritis. Biological medicines derive from living references, like plants and bacteria. These medications can assist to slow or control inflammation by targeting precise steps in the inflammatory procedure.
Another treatment choice is disease-modifying antirheumatic drugs (DMARDs). These medications assist to delay the progression of autoimmune arthritis by targeting components of the immune system itself.
People may also help from the following:
- resting the involved junctions or joints
- avoiding movements that aggravate symptoms
- practicing physiotherapy to assist to repair normal joint or junction function and mobility
Physiotherapy Treatment
Physical therapy is an essential component of the treatment of this disease. The patient requires to remain active and interested in activities. While pain may restrict the quantity of activity a patient can tolerate it is necessary to promote involvement during times of remission and permit rest and symptom-decreasing therapies during times of flare-ups. Routine activity and general activity schedules assist to keep the range of movement in affective joints or junctions, build and maintain power, keep function, and can even assist with symptom decline.
Factors that should be concentrated on during a physical therapy session are as follows:
- Muscle tone Strengthening
- Range of motion and Stretching exercise
- Education on joint protection
- Home exercise program
- Education on pain-decreasing approaches
- Muscle relaxation methods
- Splints or instruction to orthotics maybe be useful to assist sustain normal bone and joint or junction growth/control deformities during development
Some modalities that can be used to assist to decrease symptoms like pain are:
- Ultrasound therapy
- Paraffin wax bath (hands and feet primarily)
- Moist compress (hot pack)
- Hydrotherapy(warm)
- Cold packs
Stretching Exercises:
Achilles tendon and plantar fascia stretch
Twist a towel near the ball of your foot and drag your toes towards your body, maintaining your knee straight. Maintain it for 30 seconds. Reprise three times per foot.
Plantar fascia stretch
Sit down in a sitting position and relax the arch of your foot on a rounded thing, like a can of beans. Move your foot on the can in all orders for a few minutes. Replicate this activity twice a day.
Sitting plantar fascia stretch
Sit down in a sitting position and cross one foot over your opposite knee joint. Hold the base of your toes and drag them back towards your body, until you suppose a comfortable stretch. Maintain it for 15-20 seconds. Replicate this three times.
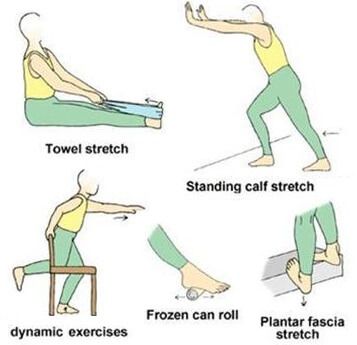
Stand or standing position facing a wall, with your hands facedown against it.
Maintaining your heels flat on the ground and back straight, gradually lean into the wall—as though you are doing a pushup against the wall. You can begin standing very near to the wall; then slowly move a slightly distant out to get a better stretch.
Maintain it for a few seconds; then rest and reprise.
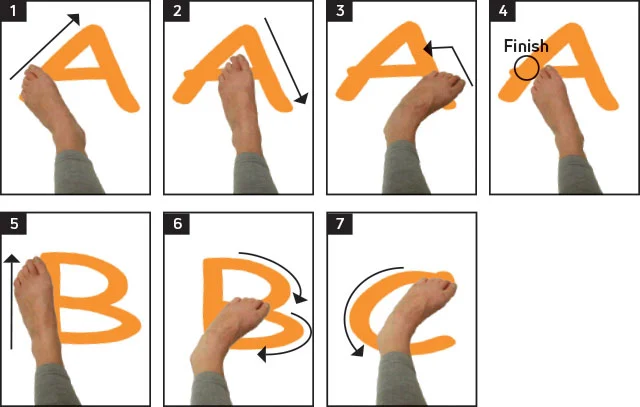
Increase range of motion and strength:
Ankle Alphabet
Sit down in a sitting position so that your feet don’t touch the ground.
Utilize your foot to write per letter of the alphabet in the aura, leading with your big toe. Control the motions small, using only your foot and ankle joints.
Towel Curls
Sit in a sitting position with both feet relaxing flat on the bottom.
Put a small towel on the bottom in front of you.
Grasp the middle of the towel with your toes and wrinkle your toes, twisting the towel toward you. Rest, then replicate.

Standing heel raise
Using a counter or chair for assistance, lift your heel, with your knee joints straight. Gradually lower your feet back down. Reprise this 10 times.
Ankle out
Create a circle out of a portion of an elastic fitness band, and maintain it in position, either with the leg of a table or chair or with your further foot. Put one foot in the circle. Keeping your heel set on the bottom, rotate your toes outwards against the resistance of the band. Obtain your foot back to the initial position gradually. Do up to replicating this 10 times, and accomplishing the set three times a day.
Basic balance
Using a steady thing like a kitchen counter for assistance, equilibrium on one foot. Build up how long you accomplish this, the goal for one minute. Attempt to accomplish this three times, and reprise the set twice a day.
Bring any chances to practice standing on one leg – making it into your everyday actions will assist you to improve.
When you sense assured with this basic balance activity, you can create it more challenging by standing on a cushion or pillow. Build up the quantity you do gradually.
When you can effortlessly balance on a cushion, and if you’re supposing convinced, go back to standing on the bottom and reprise the basic balance activity with your eyes shut.
Virabhadrasana or Warrior pose
Stand up or achieve a standing position with legs 4 to 5 feet separated.
Hold your right foot at a 90-degree inclination and with your right toe indicating out, hold your left foot at 45 grades.
Obtain your hands at shoulder level, similar to the floor.
Flex your right knee joint and see towards your right.
Maintain your hips quadrangular and the right thigh similarity to the floor. Keep for 10 to 15 seconds and dismiss the posture.

Vrikshasana /Tree Pose
Put your right foot elevated up on your left thigh. The sole should be balanced and put firmly. Hold your left leg straightforwardly and see your balance.
While inhaling, lift your arms over your head and get your palms jointly. Confirm that your spine is straight and bring periodic deep breaths.
Gradually exhale, get your hands down and terminate your right leg. Back in the standing position replicate the exact with a different leg.

Trikonasana/ Triangle Pose:
Stand or achieve a standing position with your feet broadly separated. Extend your right foot out (90 degrees) while maintaining the leg nearer to the torso.
Hold your feet pushed against the floor and balance your weight same on both feet. Inhale and as you exhale flex your right arm and push it to touch the floor while your left arm moves up.
Hold your waist straightforwardly. Confirm that your body is flexed sidewards and not ahead or back. Stretch as greatly as you can while bringing long, deep breaths.
Replicate on the different side.

Setubandhasana or Bridge Pose
Lie down on your back or achieve a supine position.
Push into your feet to raise the hips barely and glide a yoga block underneath them for help.
To arrive out, push into the feet to raise the hips too, and glide the block out.

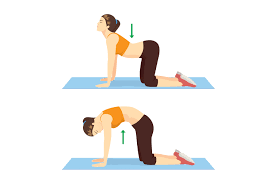
Urdhva Mukhi Marjari Asana
Bring down on your knees, position of palms is under shoulders and knees under hips
Inhale, bend your spine, and lookup

Adho Mukhi Marjari Asana
Exhale, bend your spine to create an angle of the back and permit your neck to plunge down
Concentrate your eye on your chest
Forward fold
Gradually move down the spine to turn ahead, with weight in the center of the feet, not the toes or heels. Be confident not to close the knees or move in/out with the feet. The upper body should only turn without stress, involving a relaxed head. You can carry hold of opposing elbows or twist fingers behind your back.

Cobra
Lay face down with the tops of the feet relaxing on the bottom. Palms are flat on the bottom alongside the trunk, elbows in near the body. For those incapable to put their palms on the bottom, you can use fists or elbows. Head, neck, and chest are raised off the bottom, gaze forward, maintaining the feet and legs down. Upper back muscles should be committed and arms should not be operated to perform the motion. You can test this by trying to raise your hands from the bottom and hold the pose. For more difficulties, twist fingers behind the back to pull shoulder blades jointly (or carry the opposite wrist).

Side angle pose
With feet, about 4 ft. separated, rotate the right foot out 90 grades and curve the left foot in 45 grades. Flex the right knee, maintaining the knee straight over the toes. Obtain your right elbow to the flex right knee and the left arm lengthens alongside the left ear. The plan is one straight diagonal stripe from the back left foot to that extended left arm. The arm should not be pointed directly up toward the roof. The look is beyond the outstretched fingers. Attempt not to pull or drop in the lower shoulder, but raise out of the confirming elbow. The hip joints and shoulder joints should be in the same plane, as though laying against a wall. (You could even try it against a wall to check.) Terminate any tension in the hand and fingers of the elongated arm. Repeat on the further side.

Extended leg balance
Stand up straight and gradually move your weight into one leg (using a chair or wall for help if required). When you sense satisfied, raise one leg and maintain the outside of the knee. The further hand can be put on the hip, or extended overhead. From this position, the leg can be carried out to one side, confirming that the hip does not raise. It is also essential to support the other hip aligned with the knee and ankle, without bending to the outside of the confirming foot. If feeling steady, you can bring the other arm out to the side and/or rotate the head to look the different way.

Seated spinal twist
Begin sitting with your legs outstretched. You can sit up on a pillow or tucked blanket if you sense any rounding in the lower back. Drag one knee in, raise the foot and strike it over to the exterior of the elongated leg. If probable, plant a foot on the bottom as if creating a footprint on the bottom. The foot is dragged in as close to the opposite hip as likely. Cover the opposing arm around the flexed knee, clasping it into the body. This can occur by covering the elbow around the knee, or only the hand. It is most necessary to sit up tall, extending the spine.

When to confer with a doctor or physician
An individual should contact a doctor or physician if they experience any of the following symptoms in their joints or junctions:
pain or discomfort
warmth
swelling
stiffness
People must seek medical alert as shortly as enthesitis symptoms set. Long and untreated enthesitis can cause painful and lasting joint or junction damage that can impact motion.
Individuals who have preexisting inflammatory diseases, like psoriatic arthritis or ankylosing spondylitis, may fear that enthesitis symptoms signal a worsening of their condition. But enthesitis can happen with both mild and extreme forms of these conditions. Having enthesitis symptoms only points that the underlying condition is active, and not necessarily that it is declining.
At-home treatment
In addition to medical therapies, an individual may see ease for their symptoms with some home treatments. Some potentially useful therapies contain:
- carrying a medium weight
- utilizing compression socks, braces, or other instruments that assist to decrease swelling
- lowering salt consumption
- cold or hot therapies
- elevating the affected joint
- avoiding smoking
FAQ
What kind of doctor treats enthesitis?
If enthesitis involves a precise joint or junction, a doctor or physician may suggest a corticosteroid injection into the joint or junction to reduce symptoms. A rheumatologist may suggest biological medicines to treat enthesitis resulting from autoimmune arthritis.
Is exercise good for enthesitis?
Regular activity has many advantages: it maintains or controls your heart, bones, lungs, and muscles strong. It also assists to enhance your mood and energy level and even assists you sleep nicely. Activity is only as essential if you have enthesitis-related arthritis (ERA).
Is enthesitis permanent?
Children with this kind of JIA have enthesitis, which is inflammation where tendons and ligaments attach to bones. Treatments can assist with symptoms, so kids can live a full and busy life. The symptoms can go out for a time (named remission). In some children, the disease goes out permanently.
Is enthesitis-related arthritis rare?
A periodic inflammatory rheumatic condition in a minor younger than 16 years is represented by arthritis and/or enthesitis and/or acute anterior uveitis. The most typically involved joints or junctions at diagnosis are the ankles, knees, and hips.
How common is enthesitis-related arthritis?
Enthesitis is swelling or inflammation of the entheses, the connective tissue where tendons or ligaments connect to bone. Between 10% and 15% of all kids with JIA have ERA. It is generally noticed in late youth or juvenility (eight to 15 years of period). It involves boys more frequently than girls.