Cardiac Arrest
What is a Cardiac Arrest?
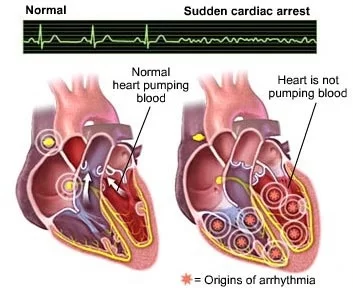
Cardiac arrest is a serious heart condition. The word arrest means to stop or bring to a halt. In cardiac arrest, the heart ceases to beat. It’s also known as sudden cardiac death.
Your heartbeat is controlled by electrical impulses. When these impulses change pattern, the heartbeat becomes irregular. This is also known as an arrhythmia. Some arrhythmias are slow, others are rapid. Cardiac arrest occurs when the rhythm of the heart stops.
Cardiac arrest is an extremely serious health issue. The Institute of Medicine reports that every year, more than half a million people experience cardiac arrest in the United States. The condition can cause death or disability. If someone is experiencing symptoms of cardiac arrest, seek emergency health assistance immediately. It can be fatal. Immediate response and treatment can save a life.
CLASSIFICATION
Clinicians classify cardiac arrest into “shockable” versus “non–shockable”, as determined by the ECG rhythm. This refers to whether a particular class of cardiac dysrhythmia is treatable using defibrillation. The two “shockable” rhythms are ventricular fibrillation and pulseless ventricular tachycardia while the two “non–shockable” rhythms are asystole and pulseless electrical activity.
CAUSES OF CARDIAC ARREST
A number of factors can cause sudden cardiac arrest. Two of the most common are ventricular and atrial fibrillation.
VENTRICULAR FIBRILLATION
Your heart has four chambers. The two lower chambers are the ventricles. In ventricular fibrillation, these chambers quiver out of control. This causes the heart’s rhythm to change dramatically. The ventricles begin to pump inefficiently, which severely decreases the amount of blood pumped through the body. In some cases, the circulation of blood stops completely. This may lead to sudden cardiac death.
The most frequent cause of cardiac arrest is ventricular fibrillation.
ATRIAL FIBRILATION
The heart can also stop beating efficiently after an arrhythmia in the upper chambers. These chambers are known as the atria.
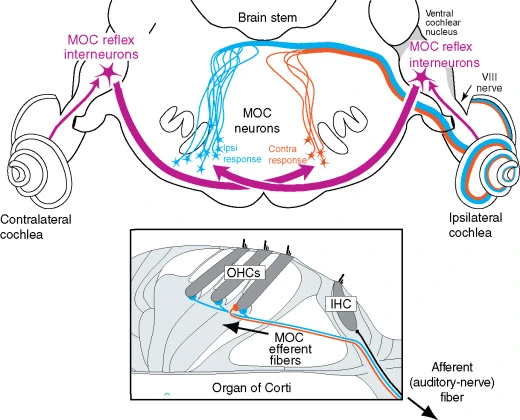
Atrial fibrillation begins when the sinoatrial (SA) node doesn’t send out the correct electrical impulses. Your SA node is located in the right atrium. It regulates how quickly the heart pumps blood. When the electrical impulse goes into atrial fibrillation, the ventricles can’t pump blood out to the body efficiently.
RISK FOR CARDIAC ARREST
Certain heart conditions and health factors can increase your risk of cardiac arrest.
CORONARY ARTERY DISEASE
This type of heart disease begins in the coronary arteries. These arteries supply the heart muscle itself. When they become blocked, your heart does not receive blood. It may stop working properly.
LARGE HEART
Having an abnormally large heart places you at increased risk for cardiac arrest. A large heart may not beat correctly. The muscle may also be more prone to damage.
IRREGULAR HEART BEAT
Valve disease can make heart valves leaky or narrower. This means blood circulating through the heart either overloads the chambers with blood or does not fill them to capacity. The chambers may become weakened or enlarged.
CONGENITAL HEART DISEASE
Some people are born with heart damage. This is known as a congenital heart problem. Sudden cardiac arrest may occur in children who were born with serious heart problems.
ELECTRICAL IMPULSE PROBLEMS
Problems with your heart’s electrical system can increase your risk of sudden cardiac death. These problems are known as primary heart rhythm abnormalities.
Other risk factors for cardiac arrest include:
- Smoking
- Sedentary lifestyle
- High blood pressure
- Obesity
- Family history of heart disease
- History of a previous heart attack
- Age over 45 for men, or over 55 for women
- Male gender
- Substance abuse
- Low potassium or magnesium
SIGNS AND SYMPTOMS
Early symptoms of cardiac arrest are often warning signs. Getting treatment before your heart stops could save your life.
If you are in cardiac arrest, you may:
- Become dizzy
- Be short of breath
- Feel fatigued or weak
- Vomit
- Experience heart palpitations Immediate EMERGENCY care is needed if someone are with experiences these symptoms
- Chest pain
- No pulse
- Not breathing or difficulty breathing
- Loss of consciousness
- Collapse
- Cardiac arrest may not have symptoms before it occurs. If you do have symptoms that persist, seek prompt medical care.
DIAGNOSIS
During a cardiac event that causes your heart to stop beating efficiently, it’s vital to seek medical attention immediately. Medical treatment will focus on getting blood flowing back to your body. Doctor will most likely perform a test called an electrocardiogram to identify the type of abnormal rhythm your heart is experiencing. To treat the condition, doctor will likely use a defibrillator to shock your heart. An electric shock can often return the heart to a normal rhythm.
Other tests can also be used after you have experienced a cardiac event:
Blood tests can be used to look for signs of a heart attack. They can also measure potassium and magnesium levels.
Chest X-ray can look for other signs of disease in the heart.
TREATING THE CARDIAC ARREST
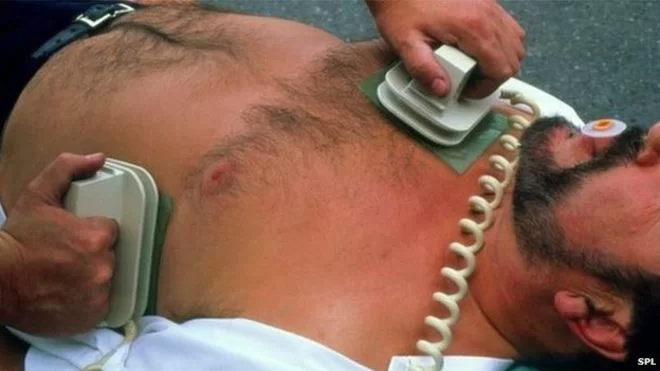
Cardiopulmonary resuscitation (CPR) is one form of emergency treatment for cardiac arrest. Defibrillation is another. These treatments get your heart beating again once it has stopped.
Medication can lower high blood pressure and cholesterol.
Surgery can repair damaged blood vessels or heart valves. It can also bypass or remove blockages in the arteries.
Exercise may improve cardiovascular fitness.
Dietary changes can help you lower cholesterol.
LONG-TERM OUTLOOK OF CARDIAC ARREST
Cardiac arrest can be fatal. However, prompt treatment increases your odds of survival. Treatment is most effective within a few minutes of the arrest.
If you have experienced cardiac arrest, it’s important to understand the cause. Your long-term outlook will depend on the reason you experienced cardiac arrest. Your doctor can talk to you about treatment options to help protect your heart and prevent cardiac arrest from happening again.
PHYSICAL REHABILITATION OF CARDIOVASCULAR DISEASE
INDICATIONS
Cardiac rehabilitation should be offered to all cardiac patients who would benefit. CR is mainly prescribed to patients with ischemic heart disease, with myocardial infarction, after coronary angioplasty, after coronaro-aortic by-pass graft surgery, and to patients with chronic heart failure. CR begins as soon as possible in intensive care units, only if the patient is in stable medical condition. The intensity of rehabilitation depends on patient´s condition and complications in acute phase of disease.
Cardiac rehabilitation typically comprises of four phases. The term phase is used to describe the varying time frames following a cardiac event. The secondary prevention component of CR requires delivery of exercise training, education and counseling, risk factor intervention and follow up.
Appropriate referral pathways should be set up so appropriate patients can be identified and invited to attend. Referrals should be invited by cardiologist/physician, cardiothoracic surgeon, cardiac team, cardic rehab co-ordinator, G.P., CCU nurses or members of the MDT. All referrals should include the following;
Patients name, age, address and contact number
Type of cardiac event and date of event
Cardiac history, complications and meds
Reason for referral
Referring persons name and contact number, date of request
Clinically relevant information – results of exercise stress test, echo, fasting lipid profile and fasting glucose profile
PHASES OF CARDIAC REHABILITATION
PHASE 1: IN HOSPITAL PATIENT PERIOD
2-5 days
Member of Cardiac Rehab team (CRT) should visit the patient to:
Give support and information to them and their families re: heart disease
Assist the patient to identify personal CV risk factors
Discuss lifestyle modifications of personal risk factors and help provide an individual plan to support these lifestyle changes
Gain support from family members to assist the patient in maintaining the necessary progress
Plan a personal discharge activity programme and encourage the patient to adhere to this and commence daily walks
Inform patients regarding phase II and phase III programs if available and encourage their attendance
At this stage emphasis is on counteracting the negative effects of a cardiac event not promoting training adaptations . Activity levels should be progressed using a staged approach which should be based on the patient’s medical condition. Patient should be closely monitored for any signs of cardiac decompensation.
Educational sessions should be commenced providing information re:
- The cardiac event
- Psychological reactions to the event
- Cardiac pain/symptom management
- Correction of cardiac misconceptions
- The use of educational materials such as the heart manual and leaflets from the Irish Heart Foundation should be considered.
PHASE II: POST DISCHARGE PERIOD
GOALS :
Reinforce cardiac risk factor modification
Provide education and support to patient and family
Promote continuing adherence to lifestyle recommendations.
PHASE III: CARDIAC REHABILITATION AND SECONDARY PREVENTION
Structured exercise training with continual educational and psychological support and advice on risk factors
Should take a menu based approach and be individually tailored.
Exercise class will consist of warm up, exercise class, cool down – may also include resistance training with active recovery stations where appropriate.
Patient shouldn’t exercise if they are generally unwell, symptomatic or clinically unstable on arrival;
- Fever/acute systemic illness
- Unresolved/unstable angina
- Resting BP systolic >200mmHg and diastolic > 110mmHg
- Significant drop in BP
- Symptomatic hypotension
- Resting/uncontrolled tachycardia (>100bpm)
- Uncontrolled atrial or ventricular arrhythmias
- New/recurrent symptoms of breathlessness, lethargy, palpitations, dizziness
- Unstable heart failure
- Unstable/uncontrolled diabetes
NEED TO CONSIDER THE FOLLOWING:
Local written policy clearly displayed for the management of emergency situations
Rapid access to emergency team in hospital or via ambulance
Regular checking and maintenance of all equipment
Drinking water and glucose supplements available as required
Access to and from venue, emergency exits, toilets and changing areas, lighting, surface and room space checked to ensure they’re appropriate
Enough space for patient traffic and safe placement of equipment
Adequate temperature and ventilation





3 Comments