Klumpke’sPalsy
What is Klumpke’s Palsy?
Klumpke’s palsy, named after Augusta Dejerine-Klumpke, is neuropathy that involves the lower part of the brachial plexus.
Usually, the 8th cervical and 1st thoracic nerves are commonly injured either before or after they have joined to form the lower trunk. This injury leads to a stretching (neuropraxia,), tearing (called “avulsion” when the tear is at the spine, and “rupture” when it is not), or scarring(neuroma) of the brachial plexus nerves. Most infants with Klumpke paralysis have a more mild form of injury like (neuropraxia) &often recover within 6 months.
In Klumpke’s palsy, the muscles of the forearm, hand &wrist are majorly affected. It occurs during delivery. Also called a birth injury to the neck and shoulder due to a difficult vaginal delivery, tumor of the shoulder or lung, or trauma to the shoulder and arm. The nerves may be torn or stretched leading to pain, numbness, or weakness.
Anatomy of Brachial Plexus:
The brachial plexus is formed from 5 nerves that originate in the spinal cord at the neck.
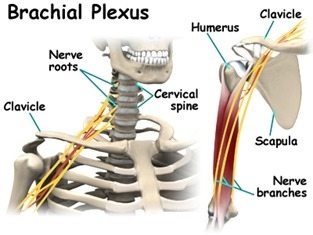
- The plexus connects these 5 nerves with the nerves that provide sensation to the skin and permit movement in the muscles of the arm& hand.
- There is a brachial plexus have both sides of the body. Each of the 5 nerves in the brachial plexus has an important function, such as carrying sensory information from the hand to the brain or powering the muscles.
- Because each nerve has its own function, the location of the nerve injury within the plexus is give information about outcomes and helps in planning the treatment.
- The brachial plexus has 5 anatomic sections, and injuries to the brachial plexus can occur in one or more of these areas.
- Spinal nerves
- Trunks
- Divisions
- Cords
- Branches
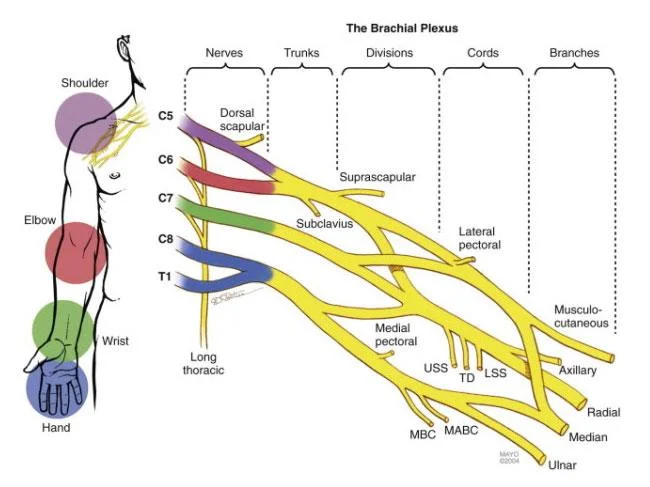
- These are made up of the anterior primary rami of spinal nerves C5,6,7,8 and T1 with contributions from the anterior primary rami of C4 and T2.
- The origin of the plexus may shift one segment either downward or upward resulting in a pre-fixed plexus or post-fixed plexus respectively.
- In a prefixed plexus, the contribution by C4 is large & T2 is often absent.
- In a post-fixed plexus, the contribution by T1 is more, T2 is always present, C4 is absent, and C5 is less in size.
- The roots join to form trunks are:
- Trunks:
- The upper trunk is made up of C5 & C6.
- The middle trunk is made up of C7.
- The lower trunk is made up of C8 & T1.
Divisions (of the trunk)
- Each trunk divides into ventral & dorsal divisions (which ultimately supply the anterior & posterior aspects of the limb).
- These divisions join to form cords. Cords (it forms 3 cords):
- The Posterior Cord is formed by 3 posterior divisions of the trunks (C5-C8, T1).
- The Lateral Cord is the anterior division from the upper & middle trunks (C5-C7).
- The Medial Cord is a continuation of the anterior division of the lower trunk (C8, T1)
Mechanism of injury:
- Mechanism of Injury of klumpke palsy of lower brachial plexus injury: Injury to the brachial plexus can occur in many types of ways.
- These include road traffic accidents, contact sports, motor vehicle accidents, or during birth.
- Majorly it can be divided into:
- Traumatic:e.g. contact sports, motor vehicle accident.
- Nontraumatic: e.g.obstetric palsy& Parsonage-Turner Syndrome.
- The network of nerves is fragile & can be damaged by pressure, stretching, or cutting.
- Stretching can occur when the head & neck are forced away from the shoulder, such as in a motorcycle fall. If severe the nerves can actually avulse or tear out of their roots in the neck.
- Pressure could occur from crushing of the brachial plexus between the collarbone & first rib, or swelling in this area from injured muscles & other structures. Such examples of events are caused by one of two mechanisms that remain constant during the injury.
- The 2 main mechanisms that can occur are traction & heavy impact.
- These 2 methods disturb the nerves of the brachial plexus and cause the injury.
- Traction: Traction, also known as stretch injury, is one of the mechanisms that cause klumpke palsy.
- The nerves of the brachial plexus are damaged due to the forced pull by the broadening of the shoulder and neck.
- Traction occurs from more severe movement and causes tension or pull among the nerves. Upward traction also results in the widening of the angle between the arm & chest as occurs when the arm and shoulder are forced upward, this time the nerves of T1 & C8 have torn away.
- Impact: Heavy impact to the shoulder is the second most common mechanism of causing klumpke plays.
- According to the severity of the impact, lesions can occur at all nerves in the brachial plexus.
- The location of impact also affects the severity of the injury and depending on the location the nerves of the lower brachial plexus may be avulsed or ruptured. Such forms of impact that affect the injury to the lower brachial plexus are shoulder dislocation, clavicle fractures, hyperextension of the arm& forearm, and sometimes delivery at birth. During the baby’s delivery, the baby’s shoulder is against the mother’s pelvic bone. During this process, the lower brachial plexus can receive more damage resulting in klumpke palsy.
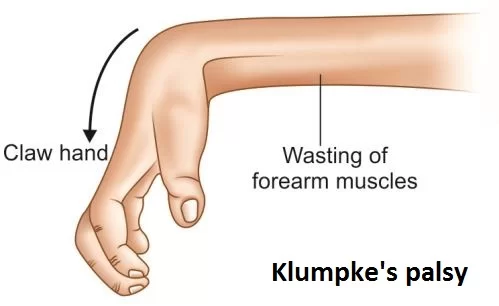
What occurs in Klumpke’s Paralysis?
- Site of injury: Lower part of the brachial plexus.
- The main cause of injury: Undue abduction of the arm, as in clutching a tree branch with the hand during a fall from a height, or sometimes in a birth injury.
- Nerve roots involved: Mainly T1 and C8.
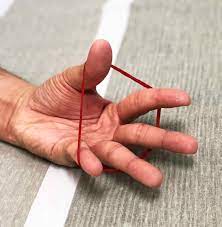
- Muscles paralyzed: Intrinsic muscles of the hand (T1) Ulnar flexors of the fingers and wrist(C8).
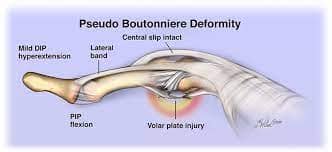
- Deformity: (position of the hand) claw hand due to the unopposed action of the extensors& long flexors of the fingers. In a claw hand, there is flexion at the interphalangeal joints & hyperextension at the metacarpophalangeal joints.
- Disability:
- Claw hand: Cutaneous analgesia & anesthesia in a narrow zone along the ulnar border of the hand & forearm.
- Horner’s syndrome: Miosis, Ptosis, anhydrosis, enophthalmos, and loss of ciliospinal reflex occur. This is because of injury to sympathetic fibers to the neck & head that leave the spinal cord through the T1 nerve.
- Vasomotor changes:
- In the skin sensory loss is occur due to arteriolar dilation. Due to the absence of sweating it is also drier, and there is a loss of sympathetic activity.
- Tropic changes:
- A long-standing case of paralysis leads to scaly & dry skin. Atrophy of the pulp of fingers so the nails crack easily.
Risk factors or causes of Klumpke’s palsy:
- Breech birth: Babies born feet-first are at more risk of Klumpke’s palsy because their arms are raised and more easily get injured from high pressure.
- Gestational diabetes: If blood sugar is not maintained, the babies have more weight making delivery very difficult.
- Use of birthing tools/improper delivery: During a complicated delivery, a baby may be pulled forcibly & quickly from the birth canal, causing injury to the shoulder & neck.
- Small maternal size/Large infant: Delivery becomes more problematic if the infant has larger than normal or if the mother is particularly small.
- Second stage of labor lasting over an hour: A long-lasting “pushing” stage may put an infant at more risk of Klumpke’s palsy.
- Injury: Trauma to the arm or the shoulder leads to Klumpke’s palsy.
- Cancer: A history or risk factor for cancer have more risk of Klumpke’s palsy.
Signs and symptoms of Klumpke’s palsy:

- Atrophy of hand and arm muscles
- Intrinsic Muscle weakness.
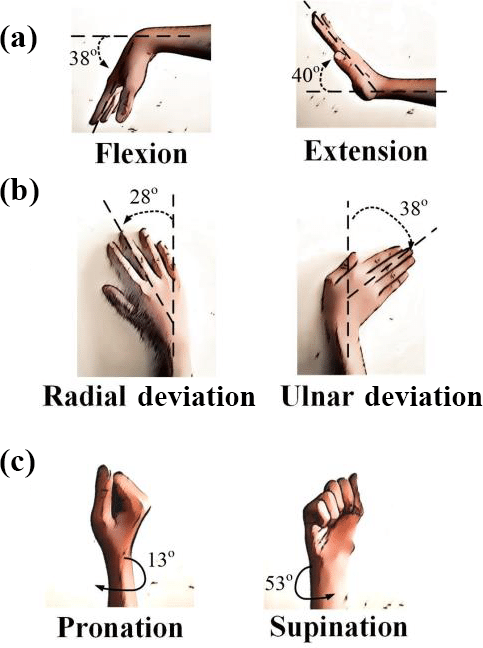
- Limited range of motion in the arm.
- Constant crying due to pain.
- Paralysis of the arm or hand.
- Limp lower arm, minimal arm, & hand movement
- Poor reflexes
- Claw hand, tightened hand, and fingers
- Sensory loss
- Paralysis
- Stiff joints like wrist and finger joints
- Pain
- Loss of movement of the arm & hand.
- Some babies have drooping of the eyelid on the opposite side of the face as well. This symptom may also be referred to as Horner’s syndrome.
- Decrease of sensation along the medial aspect of the distal upper extremity along with the C8 and T1 dermatomes.
- Myotome findings that decreasing muscular strength to muscular atrophy and positional deformity.
- Reflexes in the affected roots are absent.
- Associated injuries clavicular & humerus fractures, torticollis, cephalohematoma, and facial nerve palsy.
- Main sign:
- ”Claw hand” is a classic presentation seen where the forearm is supinated and the wrist & fingers are flexed.
- An infant with a nerve injury to the lower plexus (C8-T1) holds the arm supinated, with the wrist extended and elbow flexion.
- To diagnose Klumpke’s palsy, a medical professional may perform a physical examination &various tests for a child with arm weakness.
Diagnostic tests for Klumpke’s palsy include:
- Electromyograms (EMGs)
- Nerve conduction studies
- Ultrasounds
- X-rays
Differential diagnosis of Klumpke’s palsy:
- Distal ulnar nerve entrapment
- Thoracic outlet syndrome
- Apical lung tumor
- Neurofibroma
- Disc herniation
- Shoulder impingement
- Clavicular or vertebral fracture
- Others
Complications of Klumpke’s palsy:
- Klumpke’s paralysis complications most often occur during difficult childbirths.
- permanent disability
- claw hand deformity
- Chronic pain that results from nerve damage
- Loss of sensations leads to accidental burns
- Atrophy of muscles
- stiff joints
Treatment of Klumpke’s palsy:
Medical treatment of Klumpke palsy:
Treatment of Klumpke’s injury in babies and children is heavily dependent on the severity of the injury.
- Medications:
- Klumpke’s palsy often causes pain & burning sensation. Physicians mostly prescribe medications to relieve this mild symptom.
- Klumpke’s palsy pain, including topical ointments & prescription medications.
- Immobilization:
- The affected arm may be immobilized across the body for seven to ten days. For minimal cases, gentle massage of the arm and range-of-motion exercises may be suggested. For ruptured nerves (avulsion and rupture injuries), symptoms may improve with surgery.
- Surgical procedures:
- Surgery on the nerves (e.g., nerve grafts & neuroma excision).
- Tendon transfers: To assist the muscles that are affected by nerve damage work better.
- Muscle transfer: in which a less important muscle or tendon is removed from other parts of the body & attached to the injured arm if the muscles there damaged.
- Nerve graft: Some nerve tears can be repaired by splicing a “donor” nerve graft from another nerve.
- Nerve transfer: In such cases, a surgeon can transfer a nerve from various muscles to restore function in the nerve.
Physiotherapy Treatment:
- During the first 6 months treatment is focusing on the prevention of fixed deformities.
- Exercise therapy should be administered daily to maintain range of motion & improve muscle strength.
- Parents must be taught to take an active role in maintaining ROM & keeping the functioning muscles fit.
- Exercises should be having bimanual or bilateral motor planning activities. Initial treatment in the first 1-2 weeks after birth will consist of careful handling is required & extremes of motion are avoided for the first, one to two weeks to allow for the initial inflammatory response to the injury to calm.
Aims of physiotherapy treatment:
Physical therapy also keeps muscles and joints working smoothly & decreases stiffness in joints such as the shoulder, wrist & elbow.
- To improve flexibility
- To improve strength and dexterity
- Development of muscle strength, flexibility, stamina, and co-ordination
- Maintaining range of motion via passive movements, stretching, splinting and positioning, and protection of denervated dermatomes.
- Functional training and adoption of adaptive devices if required.
- Pain control via acupuncture and TENS
- .Sensory stimulation give to increased awareness of the arm.
- Electrical Stimulation is also helpful for weak muscles.
- Exercises to improve range of movement in the joints to prevent stiffness & pain.
- Managing chronic edema via education, compression garments & massage therapy.
- Physiotherapy interventions like constraint-induced movement therapy, Kinesio tape, electrotherapy, & use of splints or orthotics have beneficial for the affected upper limb.

Techniques:
- Passive and active stretching: A physical therapist will assist you & your child in performing gentle stretches to improve joint flexibility (range of motion), & prevent or delay contractures (tightening) in the arm.
- Improving strength: the physical therapist will teach you &your child exercises and play activities to maintain or increase arm strength. The therapist will identify games & fun tasks that promote strength without asking the baby to work too hard. As your child improves & grows, your physical therapist will identify new games &activities that will continue to strengthen the arm & hand.
- Use of modalities: A physical therapist might use a variety of intervention techniques (modalities) to improve muscle function & movement. Electrical stimulation is applied to carefully simulate the nerve signal to the muscle. Flexible tape can be applied over specific muscle areas to assist in proper muscle movement or provide relaxation. Constraint-induced movement therapy (CIMT) may be applied to the nonaffected arm to smoothly limit its use & encourage the use of the affected arm. A physical therapy session in the pool may help with stretching & strengthening. Repetitive training of the affected arm is promoted, using age-appropriate tasks, such as finger painting, building a tower, or picking up & eating small bites of food.
- Improving developmental skills: A physical therapist will help a child learn to motor skills, like putting the child’s weight on the injured limb, sitting up with arm support, & crawling. physical therapists will provide a personalized plan of care that is appropriate based on your child’s specific needs.
- Fostering physical fitness: A physical therapist will help you determine the exercises, diet, & community involvement that will provide good health throughout childhood. the physical therapist will continue to work with you & your child to determine any adaptations that may be needed, so that child can participate fully in family life & society.

Teach the parents how to handle the patient.
- Teach the parents & caretakers to grip the child with gentle care.
- playing with a child so improves sensory as well as motor function.
- The clothes are comfortable for the child.
- When the child is crying handle with peacefully & calmly.
- Avoid picking a child up by the arm or from under the armpit. This can compress or stretch the brachial plexus & cause further injury.
- Placing a child on a side-lying or on the back, with the affected limb up, to avoid compression of the injured limb.
- Put the affected arm into the sleeves before the unaffected arm. This will help to neglect extreme movement at the shoulder &will help make dressing quicker & easier.
Home exercises for Klumpke’S palsy:
- Encourage the parents to carry out specific exercises with their child two to three a day in the comfort of their own home – although the exercises can be carried out anywhere appropriate &comfortable.
- The Home Exercise Programme focuses on the following:
- Improve movement at the joints.
- Ensuring that the joints of the affected limb, especially the shoulder, elbow & wrist keep their full range of movement and avoid excessive shortening of the muscles is also called a contracture.
- This will include assisted, passive & active exercises.
- Improve the strength of muscles in the affected limb.
- Improving the child’s awareness of the arm through tactile touch &contact.
- Teach parents, carer takers & the child how to handle the affected limb & how to position it for both comfort, prevention of complications, and practicality.
Prevention of Klumpke’s palsy:
- The risk of Klumpke’s palsy can be decreased by:
- Advanced planning: If the baby is larger than normal or in the incorrect position in the weeks leading up to the due date, advanced planning by the obstetrician to prevent Klumpke’s palsy should include insuring qualified doctors are present in the delivery room, proper use of birthing instruments&extractors&induction of labor or Cesarean delivery if several risk factors are identified.
- Maternal healthcare: Good maternal healthcare during pregnancy, including avoidance or control of diabetes, can use to prevent Klumpke’s palsy.
FAQ
What is the difference between Erb’s palsy and Klumpke’s palsy?
Erb’s palsy results from injury to the upper section of the brachial plexus. Klumpke palsy is brought on by injury to the brachial plexus’s lower portion.
Where the musculocutaneous nerves are damaged is what distinguishes Klumpke from Erb’s palsy.
What is the waiter’s tip in Klumpke’s palsy?
The affected arm is adducted at the shoulder and internally rotated, the elbow is extended, the forearm is pronated, and the fingers and wrists are flexed in a typical newborn with Erb’s palsy. This distinctive stance is known colloquially as the “waiter’s tip” position.
What nerve is damaged in waiter’s tip?
Erb’s palsy is caused by nerve root damage to C5 and C6, with C7 also being impacted in 50% of cases. The ‘waiter’s tip hand’ is a characteristic symptom of Erb’s palsy. Internal rotation of the forearm, as well as wrist and finger flexion, hangs limply from the shoulder.
How does Klumpke’s palsy cause Horner syndrome?
Horner syndrome is another name for this ailment. Klumpke paralysis is caused by damage to the brachial plexus nerves during birth as a result of a difficult delivery. This injury can result in brachial plexus nerve strain damage (neuropraxia), scarring, or tears.


3 Comments