Acromioclavicular Joint
Introduction
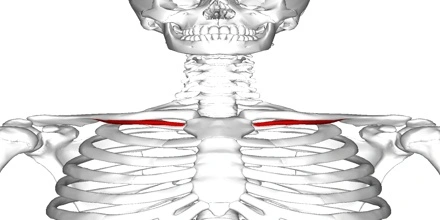
The acromioclavicular joint, often abbreviated as the AC joint, is a critical anatomical structure located at the top of the shoulder where the acromion process of the scapula (shoulder blade) articulates with the lateral end of the clavicle (collarbone). This joint plays a crucial role in the stability and functionality of the shoulder complex, allowing for a wide range of motion while maintaining the structural integrity of the shoulder girdle.
The AC Joint, a gliding or plane-style synovial joint, is created by the intersection of the lateral clavicle and the acromion process of the scapula.
The primary articulation that cuts off the upper extremity from the trunk is the AC Joint, which connects the scapula to the clavicle.
Anatomy of Acromioclavicular Joint
Articulating Surface
The lateral end of the clavicle and a tiny facet on the acromion of the scapula form the AC Joint. Because of their varying configuration, the articular facets are seen to be incongruent. They can be flat, concave-convex in both directions or reversed (convex-concave in both directions). From person to person, the articulating surfaces have different inclinations.
Three different joint types with contacting surfaces inclined at angles ranging from 16 to 36 degrees from vertical are described. The joint was more vulnerable to the wearing effects of shear stresses the closer the surfaces were to vertical. The intra-articular movements of this joint are unpredictable due to the changeable articular structure.
In order to maintain stability and keep the clavicle in touch with the acromion process of the scapula, the ligaments surrounding the joint and the capsule of the AC joint cooperate.
Joint Capsule
Synovium lines a thin capsule that surrounds the AC Joint. The inferior and superior capsular ligaments, which are further strengthened by attachments from the deltoid and trapezius, bolster the weak capsule. The superior and inferior capsular ligaments keep the AC Joint capsule strong enough to protect the joint’s integrity.
Ligament of Acromioclavicular Joint
Three ligaments work together to support the joint: The ligament that connects the clavicle to the scapular acromion is called the acromioclavicular ligament.
Superior crook of the clavicle ligament This ligament is a quadrilateral band that runs between the upper section of the lateral end of the clavicle and the adjacent part of the upper surface of the acromion. It covers the superior part of the articulation.
It is made up of parallel fibers that interlace with the aponeuroses of the Trapezius and Deltoideus. When the articular disc is present, it comes into touch with the fibers below the disc.
Anterior acromioclavicular ligament in the back This ligament, which is a little bit thinner than the one before it and covers the underside of the articulation, is joined to the surfaces of the two bones that are next to each other.
It is related to the supraspinatus tendon below and, in rare instances, the articular disc above.
The coracoacromial ligament connects the acromion to the coracoid process.
The Coracoacromial Ligament is a robust triangular band that connects the acromion to the coracoid process.
It is joined by its apex to the acromion’s summit, which is located directly in front of the clavicle’s articular surface, and by its broad base to the entire length of the coracoid process’ lateral border.
This ligament, along with the acromion and coracoid process, creates a vault to protect the humeral head.
It is connected to the clavicle above, the Deltoideus beneath the surface, and the Supraspinatus tendon below, with a bursa in between.
Its lateral border is continuous with a thick lamina that rests on the Supraspinatus and Infraspinatus tendons as it passes beneath the Deltoideus.
The ligament is sometimes described as having two marginal bands that connect at the acromion and a thinner intervening region. The two bands are linked to the apex and base of the coracoid process, respectively.
The Pectoralis minor passes between these two bands when it occasionally enters the shoulder capsule rather than the coracoid process, which results in a deficiency in the ligament’s intervening segment.
The conoid and the trapezoid ligaments make up the coracoclavicular ligament.
The clavicle and the coracoid process of the scapula are joined by the coracoclavicular ligament.
Despite not technically being a part of the acromioclavicular joint articulation, it is frequently mentioned as such since it functions as the most effective way to keep the clavicle in contact with the acromion. The conoid ligament and the trapezoid ligament are the two fasciculi that make up this structure.
These ligaments are connected to the Subclavius and Deltoideus in front and the Trapezius in the back.
Muscles around the Acromioclavicular Joint
Many of the muscles that function on the upper extremities and head attach to the clavicle, including the following:
- Clavicular Head, Pectoralis Major
- Sternocleidomastoid
- Trapezius, Deltoid
The acromioclavicular joint’s muscles
The scapula and clavicle’s movements inside the scapulothoracic and glenohumeral joints determine the movements of the acromioclavicular joint, which is entirely passive.
The descending and transverse sections of the trapezius muscle, which pull the acromion, the spine of the scapula, and the lateral third of the clavicle superomedially, are principally responsible for elevating and lateral rotating the scapula on the AC joint. Elevation of the scapula will ensue if the levator scapulae muscle contracts simultaneously, neutralizing the rotation.
The medial end of the clavicle is depressed on the sternoclavicular joint after these movements.
Due to the relaxation of lifts and the pull of gravity, the scapula’s medial rotation and depression occur passively. The levator scapulae, rhomboid, and pectoralis minor are active medial rotators, and the pectoralis minor and inferior fibers of the serratus anterior strongly depress it if necessary. The sternal end of the clavicle is elevated on the sternoclavicular joint after these movements.
Serratus anterior and pectoralis minor muscles are principally responsible for protracting the scapula on the AC joint, whereas the contraction of the horizontal and ascending sections of the trapezius muscle, as well as the rhomboid minor and major muscles, causes retraction. The sternal end of the clavicle moves anteriorly and posteriorly on the sternoclavicular joint, respectively, during protraction and retraction.
Blood Supply
The: provides the acromioclavicular joint with arterial blood flow.
At the thyrocervical trunk, the suprascapular artery emerges from the subclavian artery.
The thoracoacromial artery develops from the axillary artery.
The major arteries are accompanied by the venous drainage.
Innervation
The lateral pectoral and suprascapular nerves supply the acromioclavicular joint with its innervation. The suprascapular nerves come from the superior trunk of the brachial plexus, while the lateral pectoral nerve arises from the lateral cord of the plexus.
Function
The main purpose of the AC Joint is to give the scapula on the thorax more rotational freedom.
To follow the changing shape of the thorax while arm movement takes place, allow for adjustments of the scapula (tipping and internal/external rotation) outside of the initial plane of the scapula.
Forces from the upper extremities can pass through the joint and be transferred to the clavicle.
The main purpose of the AC Joint is to give the scapula on the thorax more rotational freedom.
To follow the changing shape of the thorax while arm movement takes place, allow for adjustments of the scapula (tipping and internal/external rotation) outside of the initial plane of the scapula.
Forces from the upper extremities can pass through the joint and be transferred to the clavicle.
Generally speaking, Sternoclavicular and Acromioclavicular movements are combined to move the Scapulothoracic Joint. When compared to the clavicle, the AC Joint’s motion is described as a scapular movement, which includes
Upward/Downward rotating medially and anteriorly around an axis perpendicular to the scapular plane. The scapula rotates roughly 30 degrees upward and downward in reference to the acromion during abduction and flexion, and about 30 degrees downward and upward in relation to the acromion during adduction and extension.
Rotation of the internal and external surfaces about a roughly vertical axis. In order to conform to the shape of the postero-lateral thorax during protraction, the scapula rotates internally at the AC level; during retraction, it rotates externally.
Tipping or tilting about an axis that is anteriorly and laterally oriented. The scapula adjusts itself on the dome-shaped thorax by anteriorly tilting during elevation and posteriorly tilting during depression in relation to the AC.
Movements
The scapulothoracic articulation, the sternoclavicular joint, and the soft tissue attachment of the scapula and posterior chest wall make up the acromioclavicular joint. The purpose of this articulation is to help with scapular movements that will place the glenohumeral joint in its proper location.
The movements within the acromioclavicular and sternoclavicular joints are tightly related to one another since they share the clavicle as a bone. The ability to provide a larger range of motions (RoM) inside the pectoral girdle, specifically from the point at which the sternoclavicular joint has reached its own maximal RoM, is the most determinant function of the AC joint.
The AC joint has three degrees of freedom and is a multiaxial joint.
Protraction – retraction
Elevation – depression (15° total angular range)
(Total range of motion 30°) Lateral rotation – medial rotation
A vertical axis that passes through the lateral end of the clavicle, between the AC joint and coracoclavicular ligament, is where the acromion expands and contracts. The conoid portion of the acromioclavicular ligament and the posterior joint capsule operate as protraction restraints. Retraction is restricted by the acromioclavicular ligament’s trapezoid portion and the anterior part of the capsule.
On the other hand, the acromion elevates and depresses along a sagittal axis. In contrast to depression, which is finally constrained by contact between the coracoid process of the scapula and the inferior surface of the clavicle, elevation is maintained by tension in both sections of the coracoclavicular ligament.
The AC joint and conoid ligament are located along a transverse axis that the acromion rotates about. It’s crucial for coordinating shoulder motions with pectoral girdle movements since it makes it possible to fully elevate the flexed arm. Both portions of the coracoclavicular ligament restrict movement.
When the arm is 90° abducted, the AC joint assumes a closed packed state; yet, when the arm is at the side of the body, it assumes a loose pack configuration. The acromioclavicular joint’s capsular pattern describes pain at extreme ranges of motion, particularly in relation to complete elevation and horizontal adduction of the arm. The joint permits protraction-retraction and elevation-depression of the lateral end of the clavicle as well as auxiliary movements in two axes (biaxial).
Closed Packed Position
The AC Joint is in its closed-packed state when the Glenohumeral Joint is abducted to 90 degrees.
open packed Position
The AC Joint’s open-packed position is unknown.
Pathology/Injury
Tolerance to Acromioclavicular Stress
The AC Joint is particularly susceptible to injury and deterioration. This is because the surfaces are irregular and tiny, which leads to high forces per unit of surface. From the second decade on, degenerative change is typical, and by the sixth decade, the joint space itself is frequently narrowed.
Variation
An X-ray analysis of 100 shoulders associated with US servicemen revealed significant diversity in the joint’s size and form. The size and shape of the articular surfaces were noticeably different. On some, a meniscus connected to the superior acromioclavicular ligament serves as their separation. This meniscus can take the appearance of a disc that separates the joint into two halves or a blade of fibrocartilage that extends almost halfway into the joint. In other joints, there is no articular cavity and just a fibrous tissue pad linked to the clavicle’s outer end serves as the joint.
Clinical significance
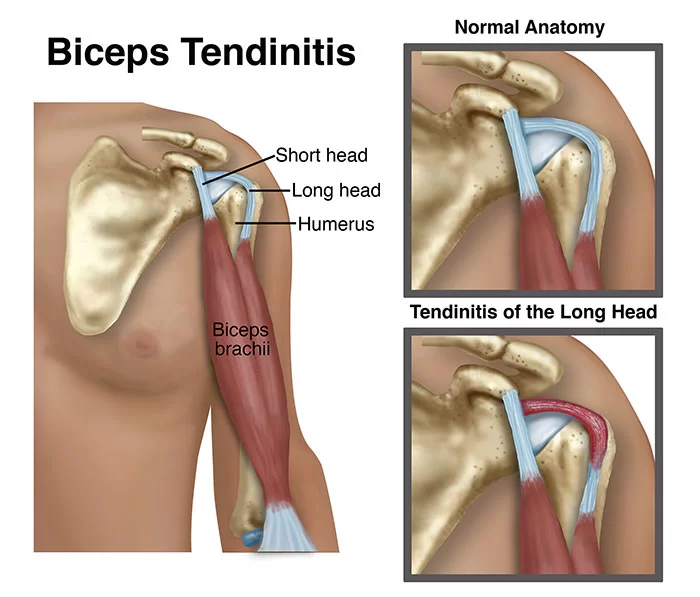
Injury
a separated shoulder
Dislocation, also referred to as AC separation or shoulder separation, is a common injury to the AC joint. This is not the same as a “shoulder dislocation,” which is the glenohumeral joint dislocating.
Acromioclavicular joint dislocation is a concern for people who participate in swimming, horseback riding, mountain biking, biking, snow skiing, and skateboarding. It is particularly common in collision sports like ice hockey, football, Judo, rugby, and Aussie rules. A fall onto the shoulder’s apex, often known as a FOOSH (Fall On Outstretched Hand) injury, is the most frequent mechanism of harm. Dislocations of the acromioclavicular joint are rated from I to VI. The degree of acromion separation from the clavicle when weight is applied to the arm determines the grade.
A significantly stretched or partially torn AC ligament and a minor amount of joint dislocation characterize Grade I. It typically has a 4 mm spacing. Grade II describes an AC joint partial dislocation, total AC joint tear, and partial coracoclavicular ligament disruption. Over 5 mm is the AC gap.
Grades I and II never require surgery and heal on their own, though it may be necessary for them to get physical therapy. Complete destruction of the AC and CC ligaments is grade III. The superior aspect of the acromion will be above the inferior aspect of the clavicle on plain film. This can also be evaluated with an MRI scan, which will also show tearing of the joint capsule and disruption of the coracoclavicular ligaments (to varying degrees depending on the severity of the AC joint disruption). On examination, the joint will be extremely sensitive and swollen. Most Grade III separations do not require surgery, and after 16 to 20 weeks, shoulder function should return to normal. However, the dislocation of the clavicle will leave the shoulder with a visible lump and some physical deformities.
Grades IV through VI are complications on a “standard” dislocation that involve collarbone displacement and nearly usually necessitate surgery. Because minor (grade I) dislocations can appear as normal joints in static pictures, dynamic US is essential for their detection. a damaged ligament heals, it can also be utilized to boost diagnostic confidence when looking for low-grade injuries.
Osteoarthritis
The acromioclavicular joint is prone to osteoarthritis. It can be pushed on by a previous injury (secondary osteoarthritis) or develop over time as a degenerative condition that frequently coexists with subacromial impingement.
FAQs
Why are the Acromio-Clavicular Joint Injuries Relatively Common?
Due to the extremely sloping structure of the acromioclavicular joint’s surface, injuries to this joint account for around 40% of all shoulder injuries in contact sports. Due to the medially and inferiorly directed force toward the shoulder when the tip of the shoulder impacts over any hard surface, the joint will dislocate. The superior and inferior capsular ligaments of the joint will resist loads over the joint in the main. If the loads are too great for these ligaments to handle, the coracoclavicular ligament will provide secondary resistance to horizontal shear. If it is unable to withstand this great load, its disruption will result, and the AC joint will either dislocate or subluxate, depending on the severity of the loads.
How do people who have AC joints sleep?
Put a pillow beneath the affected arm, including the shoulder, to avoid this. As a result, the shoulder is raised, preventing pain from the effects of gravity on the joint. For side sleepers, you must rest on the side that isn’t impacted to prevent shoulder injury.
How can I increase the mobility of my AC joints?
Neck rotation, shoulder rolls, neck stretches, shoulder blade squeezes, and other activities for AC joint rehabilitation are possible. Standing shoulder extension, and shoulder flexion when lying down and stretching the goalposts.
Does AC have an impact on joints?
The connection between air conditioning and arthritis is a chilly one—arthritis frequently worsens when the AC is turned up. You’re lucky if that isn’t the case for you! Complicating the situation, air conditioning can slightly lower the humidity in a room, which might help ease joint pain.
What is the typical AC joint distance?
joint gap of 0.5 mm can be regarded as normal in persons over the age of 60. The acromioclavicular joint space typically measures 1-6 mm (for females) and 1-7 mm (for men), decreasing with age. Acromioclavicular injury may be the cause of an abnormally large AC distance of >7 mm in men and >6 mm in women. effusion
Reference
- Abdelaal, I. M. (2011). Management of acromioclavicular joint injuries. LAP Lambert Academic Publishing.
- Bueno, J., & Flors, L. (2018). The role of imaging in the diagnosis of bronchiectasis: The key is in the distribution. Radiología. https://doi.org/10.1016/j.rxeng.2017.06.005
- Conway, A. M. (1950). Movements at the sternoclavicular and acromioclavicular joints.
- De Oliveira, C. (2017). Structural Analysis of Repairing Process of Acromioclavicular Joint Injury that Requires a Drilled Hole.
- Zanca, P. (1971). SHOULDER PAIN: INVOLVEMENT OF THE ACROMIOCLAVICULAR JOINT. American Journal of Roentgenology, 112(3), 493–506. https://doi.org/10.2214/ajr.112.3.493
- Rockwood, J., Rockwood, C. A., & Videos, S. M. (1997). The surgical treatment of acute and complete dislocation of the acromioclavicular joint using a coracoclavicular lag screw.



One Comment