Acromioclavicular Joint Pain
Acromioclavicular joint pain, often abbreviated as AC joint pain, is a common musculoskeletal condition characterized by discomfort or pain in the region of the AC joint. This type of pain can range from mild to severe and may be accompanied by other symptoms such as swelling, tenderness, and limited range of motion in the shoulder.
Introduction
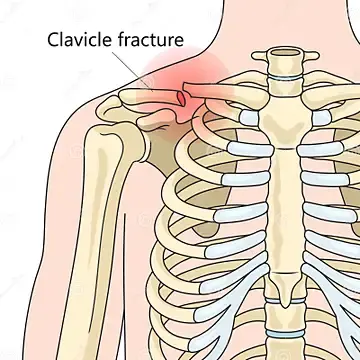
A broad group of conditions is referred to as disorders. It could be caused by degenerative disorders like osteoarthritis or trauma, like the acromioclavicular joint dislocating. An acromioclavicular dislocation is a traumatic dislocation of the joint in which the clavicle is moved away from the shoulder.
At the apex of the shoulder, where the acromioclavicular joint is placed. Pain in the acromioclavicular joint can also be referred to as ACJ pain or sprain. It occurs when the joint between the clavicle (the collar bone) and the acromion (a portion of the shoulder blade) gets inflamed. This hurts and is typically painful to the touch.
A person’s daily routine can be affected by acromioclavicular joint pain. It may restrict their capacity for overhead activities like tennis and gym routines like bench pressing or shoulder press. People of all ages may experience shoulder pain due to this common cause.
Anatomy
The acromioclavicular joint, which joins the clavicle and the acromion, is a synovial joint with an intervening fibrocartilaginous meniscal disc. It can be identified by various degrees of inclination in the sagittal and coronal planes as well as by a disc. It has an interaction between the articular cartilage and the intra-articular synovium.
A complete disc, which is extremely uncommon, and a disc that looks like a meniscoid are two that have been seen. The superior/inferior capsular ligaments and the coracoclavicular ligaments (trapezoid and conoid) are important structural features for maintaining the stability of the acromioclavicular joint, which is protected in the capsule.
The joint’s static stabilizers include the acromioclavicular (AC) and coracoclavicular (CC) ligaments. The coracoclavicular (CC) ligaments maintain vertical stability while the anterior-posterior (AC) ligaments control horizontal stability. The trapezoid portion of this ligament connects anteriorly and laterally, whereas the conoid portion attaches posteriorly and medially on the clavicle. Additionally, the trapezius and deltoid muscles help to dynamically stabilize the AC joint.
Cause of AC Joint Pain
Shoulder injuries and arthritis are some of the most common causes of pain in the AC joints.
Over 40% of all shoulder injuries involve the AC joint, according to a reliable source. These injuries are frequently suffered by people in sports-related accidents. The following sports have a high rate of AC joint injuries: skiing, cycling, ice hockey, football, and lacrosse.
These wounds could develop as a result of a car accident or another traumatic incident. Injuries to the AC joint are frequently caused by a direct fall onto the shoulder. However, they can also happen when someone falls and lands on their arm or outstretched hand.
Males have AC joint shoulder injuries more frequently than females do. These injuries are more common among men in their late 20s and early 30s.
Depending on the severity of the damage, injuries to the AC joint may result in a sprain or rupture of the surrounding ligaments.
After a fall, people who experience shoulder pain should consult a medical expert.
Arthritis
Aching AC joints might also result from shoulder arthritis. The AC joint and cartilage, a protective substance that covers the outside of bones, are frequently impacted by osteoarthritis.
The distance between bones that are attached to hands as the cartilage ages. It may hurt if the bones rub against one another.
An inflammatory disorder called rheumatoid arthritis produces inflammation in the joints. AC joint pain can also be caused by this type of arthritis.
Pain in the acromioclavicular joint can happen without a known reason. even if the shoulder does not have specifically been injured or traumatized. It may appear as a result of ‘wear and tear’ alterations in the joint or as a result of the joint being put under periodic pressure.
Additionally, we see a lot of patients who have acromioclavicular joint pain from falling onto their outer shoulder. This frequently occurs if you suffer an accident when skiing or falling off a bike. These injuries, which separate the clavicle and acromion bones, are referred to as AC joint sprains/subluxations or dislocations. A swelling or lump on the top of the shoulder can be the result of surgery.
Clinical Symptoms
Pain from an AC joint injury frequently radiates to the deltoid and neck. The clavicle may elevate and the AC joint may swell. The upper extremity is frequently kept in adduction and with the acromion compressed.
Recommended a three-grade categorization system, then Rockwood and Green expanded on this to create the Rockwood grades, a six-grade system. This classification of AC joint injuries assists in choosing the best course of action and prevents complications caused by a failure to identify a pattern of injury.
Rockwood degrees of harm.(CC: coracoclavicular; AC: acromioclavicular)
Description of the grade Observation/testing
Class I. AC ligament sprain. Intact ligaments in the AC and CC
No clavicle instability was found during stress tests.
Class II The CC ligaments are intact, however, the AC ligaments are torn. frequently referred to as a subluxation.
Direct stress tests reveal that the Clavicle is unstable.
Grade III Absence of any major delta-trapezial fascia disruption, complete disruption of both the AC and CC This is frequently called a dislocation.
The clavicle appears high (with the acromion depressed) and is unstable in both the vertical and horizontal planes due to a deformity.
Grade IV The trapezius muscle receives posterior displacement of the distal clavicle.
There is a posterior deformity.
Class V is an increased type of grade III. Complete rupture of the deltoid-trapezial fascia as well as the AC and CC ligaments.
Pseudo lateral clavicle elevation, scapular displacement downward.
Class VI Distal clavicle inferior displacement, subacromial or subcoracoid
severe trauma, generally accompanied by multiple severe injuries.
Diagnose
Acromioclavicular joint discomfort is a “clinical diagnosis,” which means that during your initial evaluation, a physiotherapist can make the diagnosis. In most cases, a diagnosis is easy to make. The diagnosis is based on three major symptoms:
The patient shows you where the discomfort is, pointing to the top of the shoulder as opposed to the external part of the upper arm. The joint is tender to the touch when you or your physiotherapist touches it.
Bringing your arm across your chest or neck causes you pain.
An X-ray is frequently taken to determine the “grade” of the AC joint injury if you fall on your shoulder. Surgery is not necessary for the great majority of these injuries since they can be treated conservatively with rehabilitation.
To confirm the diagnosis or rule out alternative causes of your discomfort, diagnostic ultrasonography scans and MRIs can be helpful. If necessary, the physiotherapist can recommend you to them.
Different Diagnoses
- 90% of dislocations in the Glenohumeral joint are anterior, where they can result in together diseases such as a Hill Sachs lesion or injury to the brachial plexus.
- pain in the AC joint caused by disc disease or osteoarthritis
- Distal clavicle osteoporosis
- Joint instability in the AC
- tear or impingement of the rotator cuff
- Capsular adhesion
- The thoracic outlet syndrome
- superior labral tears
- complex pain syndrome
- a dislocated shoulder
- The anterior humerus is subluxed.
Diagnostic Procedures
Radiography is frequently used to identify acromioclavicular dislocation. Patients with type I injuries may experience issues because nothing abnormal is visible on a radiograph. Therefore, the mechanism of damage and discomfort over the AC joint is used to make the diagnosis.
AC Joint Extension Test Resistance
Treatment of Acromioclavicular Joint Pain
Conservative – Types I and II
Initial care should follow the POLICE procedure, which includes:
- Protection,
- Optimal loading,
- Ice
- Compression,
- Elevation
and referral within the first 48 hours. A sling should be used to immobilize the shoulder along with keeping the shoulder in an elevated position when at rest. It may also be beneficial to apply tape to support the joint.
Medical Treatment
The type of treatment for an AC joint injury depends on how severe it is.
For type I and type II AC separations, nonoperative treatment is advised; however, for type III AC separations, this is still up for debate because there is a substantial risk of early-onset degeneration within the joint. However, if a type III injury does not respond to conservative therapy or the patient is younger or more active, surgical intervention may be selected as this in some circumstances may result in superior functional outcomes. Surgery is strongly advised for type IV and type V repair.
Physiotherapy treatment in Acromioclavicular Joint Pain
- Soft tissue is released to the surrounding muscles.
- Mobilization techniques to improve the movement at the joint.
- using tape to release the joint from pressure.
- Address any muscle imbalances with strength training and/or stretches.
- Postural advice
It’s important that we identify the main cause of the problem, i.e., why are you causing too much strain on the joint, if you haven’t directly injured your shoulder, say from a fall, and the discomfort just started suddenly. This could be caused by certain muscles being weak or tight. a restriction in the nearby joints, such as the thoracic spine (the region of the spine between your shoulder blades), or abnormal shoulder blade mechanics.
The physiotherapist will also evaluate your technique if you have pain while completing specific activities in the gym.
If the pain does not resolve, then an ultrasound-guided steroid injection is an effective treatment for Acromioclavicular joint pain. Following an injection, we constantly suggest that you complete a course of physiotherapy. This helps to gain additional progress in pain, range of movement, and shoulder stability.
Surgical Treatment of Acromioclavicular Joint Pain
Surgical procedures come in a variety of forms, but the four most popular ones are as follows:
AC joint fixation using hook-plates
Coracoacromial ligament transfer
Coracoclavicular interval fixation
A coracoclavicular ligament reconstruction.
A splint can be on site until the pain reduces. Return to regular movements is normally close to 2-4 weeks for a type I injury, 4-6 weeks for a type II, and 6-12 weeks for a type III. For patients whose symptoms do not improve within this boundary, intra-articular steroid injections may be indicated
The evidence supporting rehabilitative procedures is, however, lacking.
Acute Phase
Range of motion (ROM): passive, active-assisted, active
Glenohumeral Joint (GHJ): Internal rotation, external rotation, flex to tolerance: towel slides, pendular exercise
Scapula: protraction, retraction, elevation, depression
L-bar workout with active assistance for internal and external rotation: GHJ abduction: 30° to 45°, forward flexion: 30° to 40°
Posterior part of the GHJ: sleeper stretch
Isometric exercises: should be multi-angle, submaximal, and sub-painful
Closed Kinetic Chain: (no weight) hand supported in various planes and levels of elevation, control scapula position, and progress to 90°
elbow-supported internal rotation/external rotation
wall slides, scapula clock
push-ups on wall
Recovery Phase
Preventing the injury’s aggravation: Bench presses, press-ups while prone, shoulder presses, or slides are a few examples of exercises. Strength cannot be gained until proximal stability is maintained.
Motion: The GHJ should regain its complete range of motion, including horizontal adduction. It should also perform IR/ER at 90° abduction and strain the capsular ligaments.
Closed kinetic chain: Increase the loads used in previous closed kinetic chain exercises. Actively raise your arms and rotate them.
Wall slides with lower limb work and an axial load active ROM (transition from a closed kinetic chain to an open kinetic chain.
Open kinetic chain: Scapular retracting with trunk and hip extension For instance, scapular protraction exercises that involve trunk and hip flexion punches with trunk rotations, such as uppercuts, are both unilateral and bilateral.
Exercises for the Deltotrapezius complex, include shrugs, abductions at various angles, and cable work
Medicine ball tosses and catch and tubing plyometric activities are plyometric workouts (dynamic stretch shortening). Exercises specific to a sport a side-to-side throw for the overhead athlete with two hands overhead.
Return to sport
Return to sports guidelines:
Grade I: 2-4 weeks
Grade II: 4-8 weeks
Grade III: 6-8 weeks
Types V and VI postoperative personnel
Physical therapy may be used as a post-operative procedure for Type V and VI, which are thought to need surgical repair.
Surgical procedures do not significantly improve outcomes, as indicated by the results of non-operative and surgical care of type III AC separations. With proper treatment for type III injuries, recovery to full shoulder kinematics may be achieved more quickly and with fewer complications.
For type III separations, conservative management needs to be the first course of treatment.
For injuries of classes IV and V, there is no literature providing evidence-based recommendations for a specific therapy. Manual reductions have been reported to help convert type IV to type II, however, surgery is still the preferred treatment.
Post-surgical management
Goals of post-surgery
- Reduce pains and swelling in regions
- Keep the AC joint repair safe.
- protects the healing of wounds
- Start your shoulder motion early
To reduce pain and swelling, apply cold packs to the shoulder after surgery.
Remove the sling many times per day to passively swing the arm while leaning forward and moving the arm in a pendulum motion.
As needed, apply cold therapy to the shoulder for 20 minutes at a time to ease discomfort and swelling.
Remove the sling regularly throughout the day and move the elbow, wrist, and hand. Every one to two hours, lean over and swing your arms around for three to five minutes to wash under an operated arm, bend at the waist, and allow the arm to passively move away from the body. Washing under the arm while in this position is comfortable. The pendulum exercise is performed in this position.
Depending on the surgeon and the treatment, different protocols for active movement and sling use will apply. Some would advise patients to stay away from using their arms actively and to wear a sling for up to 6 weeks. Others might permit the use of a sling as required and immediate active mobility, such as up to 90 degrees in the first two weeks and then gradually increasing from there.
The post-operative rehabilitation process then adheres to the same standards as for Type I and II injuries. Exercises for range of motion are done initially, then gradually increasing strengthening is done.Too reduce the risk of chronic pain and AC joint instability, rehabilitation must be continued until the patient is fully mobile and strong.
Injury type and severity both affect how an AC joint injury is treated. A mild or moderate injury may require oral pain relievers, corticosteroid injections, physical therapy, and physiotherapy.
In some circumstances, doctors could advise surgery to relieve pain in the AC joint. One of the most common operations for osteoarthritis of the AC joint is distal clavicle excision (DCE).
A surgeon removes the collarbone’s distal end during DCE. This technique could reduce shoulder pain in the AC joint and increase the range of motion.
Weight loss or performing light exercise may help people with shoulder arthritis. The following are additional options for managing shoulder arthritis:
Topical creams or ointments for pain
Nonsteroidal anti-inflammatory medications (NSAIDs) with paracetamol
injections of corticosteroids or hyaluronic acid
Anyone having severe discomfort in their AC joints needs to take medical advice. They can assess a person’s symptoms and suggest the most effective course of action.
Resting from the movements and activities that trigger the discomfort should be the first step in treatment. Painkillers and anti-inflammatory drugs may also be helpful. We recommend you consult a physiotherapist for an evaluation if the pain does not go away after a few weeks.
For the purpose of helping the pain decrease, we may advise you to wear a support device for a few days if the injury is recent (within the previous week) and still very severe. Our recommendation is to not use a sling for more than a week. Depending on how severe the strain is, follow this advice. While the injury heals, it’s important that your shoulder does not get stiff.
After an in-depth assessment, your physiotherapist will perform many kinds of physical treatments and exercises to help you feel better and to help you restore the complete use of your arm and strength.
Do’s and Don’t’s for acromioclavicular joint pain
DO:
As much as the pain will allow, keep your shoulder moving.
Consult a physiotherapist if you’ve experienced the pain for more than two weeks and it does not decrease despite rest.
Consider an ultrasound-guided injection if PT is not working to relieve the pain or if it is making it more serious.
DON’T:
Do not fully stop using your shoulder; doing so may prevent recovery.
whether you have pain when doing things above shoulder level, cease doing them for two weeks and see whether the pain goes away.
Massage or rubbing won’t be of any help!
Anyone who has continuous or severe shoulder pain needs to see a doctor. A healthcare provider should be consulted by those who are at risk for arthritis. The following individuals have a higher risk of developing arthritis:
older individuals
Those with a family history of arthritis
people who smoke
individuals who have experienced joint injuries in the past
those with more weight or obesity
A damaged AC joint or arthritis may be the cause of persistent shoulder pain. People who have persistent shoulder discomfort or who are worried about their shoulder pain should consult a medical expert.
Measures outcome
DASH: examines for arm, shoulder, and hand disabilities.
Simple questionnaires for the shoulder test: In order to evaluate the functional impairment of the shoulder, 12 questions were asked. 2 discuss how function and pain are related, 7 discuss function and strength, and 3 discuss a range of motion.
The patients’ subjective level of pain and impairment is an important end measure for the shoulder pain and disability index (SPADI). A total score between 0 (no pain or functional difficulty) and 100 (highest level of pain and functional difficulty) is generated by adding the two subscales of pain and disability. When it comes to shoulder discomfort that is musculoskeletal, neurogenic, or of unknown origin, the SPADI is reliable, valid, and responsive. Evaluate patients with musculoskeletal shoulder disorders for functional limits and discomfort. On a scale of 1 to 4, 10 questions about function are used to generate the functional score.
Look for tenderness when palpating the AC joint.
The O’Brien test tightens the posterior capsule and posteriorly transposes the humeral head during the examination, placing pressure on the labrum and causing pain and weakness.
Provocative testing for acromioclavicular joint damage is the Paxinos sign. The Paxinos test is a useful clinical diagnostic tool, and bone scanning is the most trusted imaging modality for the detection of AC joint disease, There is a high degree of confidence in the diagnosis of AC joint pathology when both of these tests are positive.
Test of Stenvers 4: Clavicular Roll
Clavicular Roll Resisted AC Joint Extension Test,
It is possible to differentiate between type I and type II injuries using the history of the injury’s mechanism and palpation of the AC joint. In a type I injury, swelling and pain are typically present when the arm is abducted, whereas in a type II injury, discomfort is typically felt during all arm movements. A type II injury is indicated by a slight AC joint deformity
A type III injury is identified by an evident step deformity of the AC joint, and the patient typically maintains the injured arm as close to his body as possible.
Summary
The upper shoulder blade and clavicle are joined by the AC joint. An individual’s shoulder’s range of motion and arm movements are supported by an ideal AC joint.
AC joint pain that will not go away could be caused by shoulder injuries or different types of arthritis. These may include osteoarthritis, rheumatoid arthritis, or sports-related injuries.
Anyone experiencing continuous or increasing shoulder pain should speak with a medical practitioner for a more complete assessment.
FAQs
Put a pillow under any affected arm, shoulder included, to prevent this. By raising the shoulder, gravity is prevented from pulling on the joint and causing pain. For side sleepers, you must do your best to sleep on the side that is not impacted by your shoulder pain.
Acromioclavicular joint pain can interfere with a person’s normal daily activities. It may restrict their capacity for overhead activities like tennis and gym routines like the bench or shoulder press. It is a common cause of shoulder pain and can affect people of all ages.
Interpretation. The acromioclavicular joint space normally measures 1-6 mm (females) and 1-7 mm (males) 4, decreasing with age – a joint space of <0.5 mm can be considered normal in patients >60 years old 2. When the AC distance is abnormal and can result from acromioclavicular injury, it is >7 mm in men and >6 mm in women
Treatment may include:
Rest. This allows your shoulder to heal. …
Sling. This protects the shoulder and maintains the joint’s beneficial healing environment.
ice packs. These aid in pain relief and edema reduction.
Prescription or over-the-counter pain medicines. These help relieve pain and swelling
To prevent this, place a pillow under the entire affected arm, including the shoulder. As a result, the shoulder is lifted, reducing pain caused by the joint’s exposure to the effects of gravity. To avoid shoulder injury for side sleepers, you must rest on the unaffected side.
References
Cailliet, R. (1981). Shoulder pain.
Chaudhury, S., Bavan, L., Rupani, N., Mouyis, K., Kulkarni, R., Rangan, A., & Rees, J. (2017). Managing acromioclavicular joint pain: a scoping review. Shoulder & Elbow, 10(1), 4–14. https://doi.org/10.1177/1758573217700839
Heck, C. V., & Chandler, F. A. (1955). DIAGNOSIS AND TREATMENT OF PAIN IN THE ACRO-MIO-CLAVICULAR JOINT†. Journal of the American Geriatrics Society. https://doi.org/10.1111/j.1532-5415.1955.tb01012.x
Lee, B., & Park, D. (2020). Botulinum Toxin Injection of a Patient with Intractable Acromio-Clavicular Joint Pain due to Distal Clavicular Osteolysis. Pain Medicine, 21(12), 3730–3732. https://doi.org/10.1093/pm/pnaa066
Michener, L. A., McClure, P., & Karduna, A. R. (2003). Anatomical and biomechanical mechanisms of subacromial impingement syndrome. Clinical Biomechanics, 18(5), 369–379. https://doi.org/10.1016/s0268-0033(03)00047-0
Ritchie, D. M., Boyle, J. A., Mcinnes, J. M., Jasani, M. K., Dalakos, T. G., Grieveson, P., & Buchanan, W. W. (1968). CLINICAL STUDIES WITH AN ARTICULAR INDEX FOR THE ASSESSMENT OF JOINT TENDERNESS IN PATIENTS WITH RHEUMATOID ARTHRITIS. QJM: An International Journal of Medicine. https://doi.org/10.1093/oxfordjournals.qjmed.a067150
Trikha, S. P., Acton, D., Wilson, A. J., & Curtis, M. J. (2004). A new method of arthroscopic reconstruction of the dislocated acromioclavicular joint. Annals of the Royal College of Surgeons of England, 86(3), 161–164. https://doi.org/10.1308/003588404323043265
Waldman, S. D. (2021). The Shoulder and Elbow, E-Book: Pain Medicine: A Case-Based Learning Series. Elsevier Health Sciences.






2 Comments