Spastic Diplegia
Introduction
Spastic diplegia, also known as spastic bilateral cerebral palsy, is a neurological condition that primarily affects motor function and muscle control in individuals. This condition is characterized by increased muscle tone, stiffness, and difficulty with coordinated movements, particularly in the legs. Spastic diplegia is caused by damage or abnormalities in the developing brain, typically occurring before or during birth.
Learning that a child has been diagnosed with cerebral palsy can be an overwhelming experience for most parents. When faced with such a diagnosis, it’s natural to worry about your child’s future, their potential for independence, and the quality of life they can lead. While cerebral palsy remains incurable, it’s essential to understand that many children can significantly benefit from early intervention programs aimed at improving muscle control, mobility, and overall independence. The prognosis for your child will largely depend on the severity of their condition and the specific form of cerebral palsy they have.
The most prevalent type of cerebral palsy in the United States is spastic cerebral palsy, accounting for approximately 80% of all cases. Spastic cerebral palsy manifests in three distinct forms, each named based on the affected areas of the body: spastic diplegia, spastic hemiplegia, and spastic quadriplegia. Let’s delve into what spastic diplegia entails, focusing on insights provided by the Philadelphia cerebral palsy law firm, Raynes & Lawn.
Understanding Spastic Cerebral Palsy:
Spastic cerebral palsy is the most commonly diagnosed type within the cerebral palsy spectrum. Individuals with this condition exhibit increased muscle tone in one or more regions of their bodies. The origins of spastic cerebral palsy stem from damage to various brain areas during fetal development, shortly before birth, during labor and delivery, or in the immediate postnatal period.
The distinct forms of spastic cerebral palsy, such as spastic diplegia, hemiplegia, and quadriplegia, are defined by the specific areas of the body affected. People with spastic CP may encounter a range of challenges, including:
- Extremely rigid muscles
- Difficulty moving affected areas
- Spasticity
- Difficulty transitioning between positions
- Coordination problems
- Balance issues
- Difficulty with speech or swallowing
Spasticity results from damage to specific brain regions responsible for motor function control, including the corticobulbar and corticospinal tracts. Such damage leads to disrupted neural signaling to the affected areas of the body, contributing to the symptoms observed in individuals with spastic cerebral palsy.
What is Spastic Diplegia?
Spastic diplegia, also known as spastic diparesis, represents a particular manifestation of spastic cerebral palsy that primarily impacts the lower limbs, with minimal or no involvement of the arms. Individuals diagnosed with spastic diplegia often exhibit a distinctive gait pattern characterized by leg scissoring. Leg scissoring occurs when the knees turn inward or cross while walking, a consequence of heightened muscular spasticity and rigidity in the leg and hip muscles.
While some symptoms of spastic diplegia can overlap with other forms of cerebral palsy, several distinctive characteristics are associated with this specific subtype:
- Excessively rigid leg muscles: People with spastic diplegia commonly experience increased stiffness in their leg muscles.
- Jerky and exaggerated leg reflexes: Reflex responses in the legs can appear abrupt and exaggerated.
- Toe walking: Many individuals with spastic diplegia tend to walk on their toes due to the spasticity in their leg muscles.
- Leg scissoring: The distinctive leg scissoring gait, where the knees come together or cross during walking, is a hallmark feature of spastic diplegia.
What are the Causes of Spastic Diplegia?
Cerebral palsy arises from damage to the developing brain before, during, or shortly after birth. Common factors leading to early brain damage include premature birth, infections, and oxygen deprivation to the brain.
The specific areas of the brain affected and the extent of damage determine the nature and severity of the condition. For instance, damage to the cerebellum results in ataxic cerebral palsy, while damage to the motor cortex leads to spastic cerebral palsy.
Spastic diplegia represents a subtype of spastic cerebral palsy primarily impacting motor control in the lower limbs. Typically, this form of spastic CP is linked to milder brain damage, which explains why motor impairments are predominantly localized to the legs rather than affecting the entire body.
Birth Asphyxia:
Brain damage during birth, especially in complicated deliveries, can be attributed to various factors. Swift and decisive action is crucial to prevent oxygen deprivation during labor and birth, a condition known as birth asphyxia. Several circumstances during childbirth can contribute to this:
- Overuse of Pitocin: This hormone, used to induce labor, can lead to complications.
- Umbilical cord compression or prolapse: Obstructions in the umbilical cord can restrict oxygen flow.
- Shoulder dystocia: A situation where the baby’s shoulders become stuck during delivery.
- Blocked airway: Any impediments to the infant’s airway can hinder oxygen intake.
- Prolonged Cesarean process: Delays during a C-section can affect oxygen supply.
Hypoxic Ischemic Encephalopathy (HIE):
HIE is a brain disorder resulting from inadequate blood flow and oxygen levels in the body. Factors contributing to HIE during or shortly after labor and delivery include:
- Umbilical cord issues: Abnormalities in the umbilical cord can impact blood and oxygen supply.
- Rupture of the uterus: A uterine rupture can lead to oxygen deprivation.
- Excessive placental bleeding: Hemorrhaging in the placenta can affect oxygen transport.
- Abnormal fetal position: An atypical fetal position can impede delivery and oxygenation.
- Prolonged late stages of labor: Lengthy labor can contribute to oxygen-related issues.
- Low blood pressure in the mother or baby: Insufficient blood pressure can reduce oxygen delivery.
- Severe prematurity: Babies born very prematurely are at higher risk for HIE.
- Lung or heart issues, infections, or brain and skull trauma: These factors can also contribute to HIE.
Healthcare providers should remain vigilant for signs of fetal distress, low heart rate, or respiratory difficulties during labor and delivery, as these may indicate the presence of HIE.
It is essential to acknowledge that lower body motor impairments, as seen in spastic diplegia, can still have profound consequences. Fortunately, with appropriate management through rehabilitative therapies and other interventions, individuals with spastic diplegia can enhance their quality of life. In the following section, we will explore the potential effects associated with spastic diplegia.
Risk factors related to the Spastic Diplegia
While pinpointing the exact cause of spastic diplegia in an individual can often be challenging, several common risk factors are associated with the development of this condition in children:
- Premature Birth: Babies born before 37 weeks of gestation face an elevated risk of developing spastic diplegia.
- Low Birth Weight: Babies with low birth weight, even those born at full term, are at a heightened risk for spastic diplegia.
- Multiple Births: The presence of multiple fetuses during pregnancy increases the likelihood of one or more babies developing spastic diplegia or other forms of cerebral palsy. This heightened risk is primarily due to the increased likelihood of premature birth, low birth weight deliveries, or a combination of both factors in multiple pregnancies.
- Infection: Various studies have established a connection between spastic diplegia and other forms of cerebral palsy and infections during pregnancy. These infections can encompass viral illnesses like meningitis, cytomegalovirus (CMV), chickenpox, or rubella, as well as bacterial infections involving the placenta or fetal membrane. Additionally, sexually transmitted infections, such as herpes, have also been linked to an increased risk of cerebral palsy, including spastic diplegia.
- Blood Type Incompatibility and Jaundice: In cases where there’s an Rh-negative blood type incompatibility between the pregnant individual and their fetus (who has Rh-positive blood), it can lead to jaundice in the baby and potential oxygen deprivation to the brain. This circumstance can elevate the risk of cerebral palsy, including spastic diplegia.
Which are the Signs & Symptoms of Spastic Diplegia?
Most individuals diagnosed with spastic diplegia typically exhibit normal cognitive abilities and have the potential to walk independently. However, it’s important to note that the severity of motor impairments can vary, and some individuals may rely on assistive mobility devices like crutches, wheelchairs, or walkers for support.
Early identification of signs of cerebral palsy is crucial to ensure prompt access to necessary treatments, minimizing the impact of motor impairments and preventing the development of poor movement habits.
Common signs and symptoms associated with spastic diplegia include:
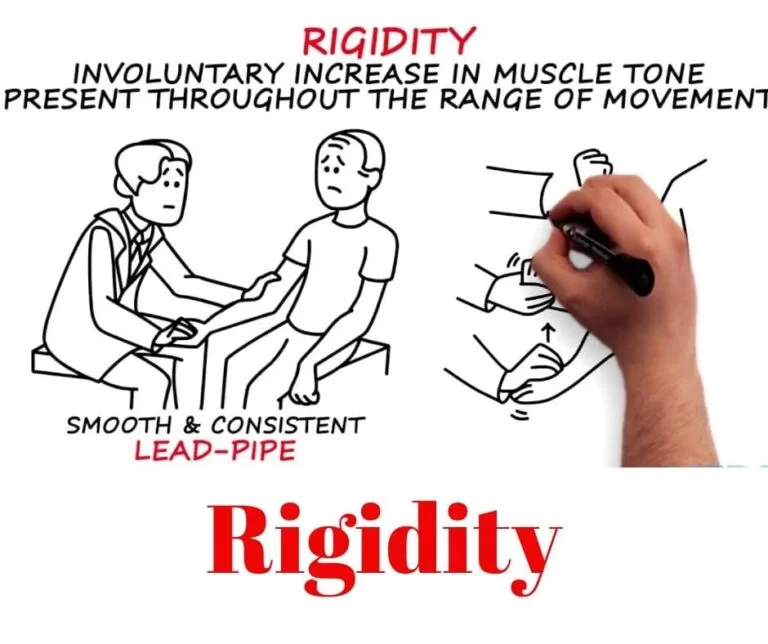
Spasticity:
Spasticity is a common feature experienced by individuals with spastic diplegia. It arises from damage to the motor cortex, disrupting the communication between the brain and the muscles. Consequently, the muscles connected to the affected area remain persistently contracted without voluntary control.
Spasticity serves as the underlying cause behind several secondary complications associated with cerebral palsy, including the development of abnormal walking patterns, chronic pain, and disturbances in normal growth.
It’s important to note that while the initial brain damage causing cerebral palsy does not worsen over time, spasticity itself can intensify if left unmanaged. This increased spasticity can severely impede mobility and, in some cases, lead to a loss of the ability to walk.
Abnormal Gait:
An abnormal gait, or walking pattern, is a common characteristic among individuals with spastic diplegia. This abnormal gait arises due to the inability of leg muscles to fully relax because of spasticity. As a result, continuous muscle contractions lead to rigid movements, making it challenging for individuals to maintain balance while walking.
Typical abnormal gait patterns seen in individuals with spastic diplegia include:
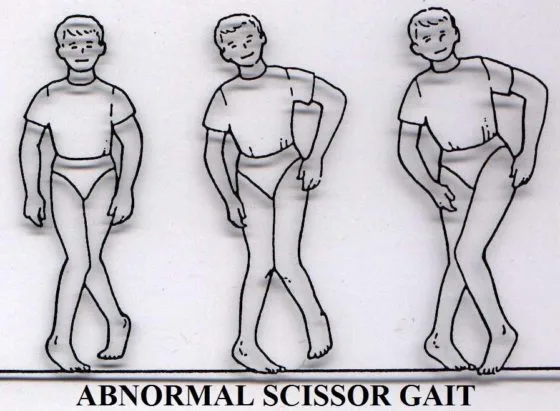
- Scissor Gait: This pattern involves walking with the knees turned inward, resembling a scissor-like motion.
- Tiptoeing: Walking predominantly on the toes, with limited heel-to-toe contact, is another common gait variation.
- Crouch Gait: In this gait pattern, individuals walk with continuously bent knees, hips, and ankles, resulting in a crouched posture.
Muscle Weakness:
Muscle Weakness is also a significant concern in individuals with spastic diplegia. Severe spasticity in the leg muscles can discourage physical activity, leading to muscle and bone weakening. Our bodies typically build strength through regular movements that apply pressure to joints, bones, and muscles. The absence of such activities can increase the risk of injury and exacerbate muscle weakness.
Delay developmental milestones:
The interplay of spasticity and muscle weakness can indeed lead to delays in achieving developmental milestones such as crawling, standing, and walking for children with spastic diplegia. However, it’s essential to emphasize that these delays don’t signify that children with this condition will never attain these skills; rather, it may take them a bit longer to do so.
Remarkably, a significant proportion, approximately 50-60%, of children diagnosed with cerebral palsy, including those with spastic diplegia, eventually achieve the milestone of independent walking.
For those individuals with more severe motor impairments who may require assistance for mobility, there are effective strategies to maximize their independence. They are taught how to use mobility aids such as walkers and wheelchairs. These assistive devices play a crucial role in enhancing their mobility and overall quality of life, enabling them to navigate their environment with greater ease and independence.
Limited growth and development:
The presence of spasticity during early childhood can have a profound impact on a child’s growth and overall development. In the case of individuals with spastic diplegia, imbalanced muscle tension, and continuous muscle contractions can exert disproportionate pressure on various muscles, joints, and bones in the legs. As a result, deformities or distortions may emerge over time. For instance, one leg may experience greater strain, leading to a potential discrepancy in leg length.
Having explored the potential signs and symptoms of spastic diplegia, it’s imperative to shift our focus toward treatment and underscore the critical importance of early intervention.
How to Diagnose Spastic Diplegia?
Diagnosing spastic diplegia typically follows the confirmation of cerebral palsy through neuroimaging techniques like MRI (Magnetic Resonance Imaging) or cranial ultrasound. Spastic diplegia, a specific subtype of cerebral palsy, is identified through the observation of spasticity primarily affecting the lower limbs. In addition to clinical observation, healthcare professionals may recommend further assessments and tests to provide a comprehensive evaluation, including:
- EEG (Electroencephalogram): An EEG may be conducted to rule out any seizure disorders, as some individuals with cerebral palsy can also experience seizures.
- Metabolic and Genetic Screening: Blood, urine, or skin tests may be employed to screen for metabolic or genetic issues that could contribute to or be associated with cerebral palsy.
- Comprehensive Assessments: A range of assessments may be performed to evaluate various aspects of an individual’s health and development, including vision, hearing, speech, cognitive function, overall development, and movement abilities.
These additional tests and evaluations help healthcare providers gain a more comprehensive understanding of the individual’s condition and any potential coexisting factors or associated conditions. This, in turn, enables the development of a tailored treatment and intervention plan to address the unique needs of the person diagnosed with spastic diplegia.
What are the Treatment for Spastic Diplegia?
While cerebral palsy is indeed a lifelong condition, individuals can significantly enhance their quality of life through appropriate treatment and interventions. Spastic diplegia, with its varying degrees of severity and impacts on leg muscles, necessitates a personalized approach to treatment.
The primary focus of treating spastic diplegia revolves around harnessing the brain’s remarkable capacity for adaptation and rewiring of neural circuitry, known as neuroplasticity. This intrinsic mechanism enables functions affected by brain damage to be rerouted to healthier, unaffected regions of the brain.
One of the most effective ways to promote neuroplasticity is through task-specific repetition. The brain operates on a ‘use it or lose it’ principle, with the strength of neural pathways growing as skills are practiced. Starting interventions at a young age is particularly advantageous, as the developing brain exhibits higher neuroplasticity. Nevertheless, it’s essential to recognize that the brain retains its adaptability throughout life, offering opportunities for improvement at any age.
Management and intervention strategies for spastic diplegia typically encompass the following approaches:
Physical Therapy:
Physical therapy plays a pivotal role in mitigating the impact of spasticity in the legs for individuals with spastic diplegia. During physical therapy sessions, individuals receive targeted interventions aimed at addressing various aspects of their condition. These may include:

- Stretching Spastic Muscles: Therapists work on stretching muscles affected by spasticity to improve flexibility and reduce muscle tension.
- Strengthening Underused Muscles: Exercises are designed to target muscles that may be underutilized due to spasticity, enhancing overall muscle strength and control.
- Gait Training: Specialized gait training programs focus on improving an individual’s ability to walk effectively. This may involve exercises conducted in a pool or using a weight-bearing treadmill. Such activities relieve joint pressure, enabling individuals to concentrate on refining their walking form. They also enhance stability, reduce the risk of falls, and minimize the likelihood of injuries resulting from falls, instilling confidence in individuals as they practice more advanced skills.
- Incorporating Fun and Engaging Activities: Many physical therapists integrate enjoyable games and activities like obstacle courses and balance challenges into their sessions, particularly when working with pediatric patients. These interactive approaches motivate children with spastic diplegia to actively participate in therapy and facilitate the transfer of learned skills to home settings.
Physical therapy stands out as an effective treatment for spastic diplegia due to its emphasis on repetition. The consistent practice of exercises stimulates neuroplasticity, fortifying the connections between the brain and muscles. The ‘practice makes perfect’ principle applies, as increased repetitions activate neuroplasticity, fostering improvements in motor function over time.
Occupational therapy:

Occupational therapy takes a holistic approach, focusing on enhancing independence in activities of daily living for individuals with spastic diplegia. Given that the primary motor impairments in spastic diplegia predominantly affect the lower limbs, individuals can often achieve a high level of independence by learning to utilize their upper body strength and coordination.
Occupational therapy empowers individuals with spastic diplegia to develop the skills necessary for tasks such as transfers, dressing, and toileting. These therapists work closely with patients to optimize their arm and upper body function, allowing them to carry out these daily activities autonomously.
In cases where motor impairments are more severe, occupational or physical therapists may introduce the use of mobility aids such as walkers, crutches, or wheelchairs. Additionally, occupational therapists may provide guidance on the use of adaptive equipment, such as sock aids or leg lifters, which further enhance functional independence.
The overarching goal of occupational therapy is to equip individuals with spastic diplegia with the tools and techniques they need to lead fulfilling, independent lives despite the challenges posed by their condition.
Muscle Relaxants:
Botox and muscle relaxants play a crucial role in managing spasticity by intercepting the signals responsible for causing tightness in spastic muscles. These interventions offer valuable benefits, including the postponement of contracture progression and temporary relief from spasticity.
Given that spastic diplegia primarily impacts the leg muscles, the use of oral medications affecting the entire body is generally less preferable. Instead, targeted injections directly into the affected muscles prove to be more effective in managing spasticity.
It’s important to note that the effects of Botox and muscle relaxants are not permanent. Therefore, individuals should capitalize on the period of reduced spasticity that these treatments provide. This window of opportunity should be maximized through intensive physical therapy efforts, as it can lead to more sustained relief and improved mobility over the long term.
Orthotic:
Orthotic devices, including braces, splints, and casts, serve as wearable solutions designed to maintain proper body alignment.
Spasticity exerts forces that disrupt the body’s alignment, placing undue stress on the joints. Over time, this pressure can impede a child’s growth and lead to severe complications, including hip dislocations. Orthotic devices serve a dual purpose in addressing these challenges:

- Stretching Spastic Muscles: Orthotics gently stretch spastic muscles, helping to alleviate tightness and prevent further constriction.
- Structural Support: These devices offer structural support, effectively reducing the risk of increased muscle tightness.
- Positioning and Stability: Orthotics aid in maintaining correct positioning and stability, ultimately enhancing independence in walking and facilitating transfers.
By employing orthotic interventions, individuals with spastic diplegia can experience improved comfort, enhanced mobility, and a reduced risk of complications associated with misalignment and muscle spasticity.
Surgery:
Surgical interventions for spastic diplegia primarily revolve around two main approaches: muscle lengthening and realignment procedures or selective dorsal rhizotomy (SDR).
Muscle lengthening and realignment surgeries involve the manual adjustment of muscles to achieve improved length and alignment. These procedures aim to alleviate spasticity and enhance overall motor function.
On the other hand, selective dorsal rhizotomy (SDR) entails precise incisions made at specific nerve roots, leading to the permanent severing of innervation to reduce the excitability of spastic muscles.
Living with Spastic Diplegia
Spastic diplegia, a subtype of cerebral palsy primarily impacting the legs, has the potential to significantly influence an individual’s growth and walking abilities if not effectively managed.
The encouraging aspect is that the impact of motor impairments stemming from cerebral palsy can be effectively mitigated by fostering neuroplasticity.
The key to making progress and attaining the highest possible level of independence lies in a dedicated commitment to rehabilitation. The journey toward recovery necessitates an intensive effort characterized by thousands of repetitions. Thus, maintaining unwavering motivation, adhering to exercise routines, and placing trust in the rehabilitation process is pivotal. It’s essential to recognize that the more one practices, the more they stimulate the brain, enhancing its adaptability and facilitating positive neurological changes.
Conclusion
Spastic diplegia cerebral palsy constitutes a variant of cerebral palsy, a neurological condition typically manifesting in infancy or early childhood, characterized by enduring challenges in muscle control and coordination. This condition presents with notable symptoms, including heightened muscle tone resulting in spasticity (manifesting as stiffness or tightness in the muscles) primarily affecting the legs. In contrast, the muscles of the arms are typically less affected or unaffected altogether. Additional observable symptoms encompass delayed achievement of motor milestones (such as rolling over, sitting, and standing), toe-walking, and a distinctive ‘scissored’ gait pattern when walking.
Individuals born prematurely or with low birth weight face an elevated risk of developing cerebral palsy. Nonetheless, the precise causative factors often remain elusive. Nevertheless, spastic diplegia cerebral palsy has been associated with various factors, including genetic abnormalities, congenital brain malformations, maternal infections or fevers, and potential injury occurring before, during, or shortly after birth.
FAQ
What is the cause of spastic diplegia?
There are many times no recognized specific causes. Spastic diplegia cerebral palsy, however, has been associated with genetic abnormalities, congenital brain deformities, maternal illnesses or fevers, and/or injuries before, during, or soon after delivery.
What are spastic Diplegia cerebral palsy symptoms?
The most typical signs of spastic CP are stiff, tight muscles (hypertonia) on one or both sides of the body.
Excessive movement.
Restricting movement.
Unusual gait.
Knees crossed.
Joints don’t stretch all the way.
Balancing on one foot.
Contractures.
What is the difference between diplegia and paraplegia?
Diplegia/diparesis often means the lower body is most afflicted; the legs are typically impacted more than the arms. Hemiplegia/hemiparesis is a condition that affects the arm and leg on one side of the body. The lower body, including both legs, is impaired in paraplegia/paraparesis.
Is spastic diplegia curable?
There is presently no treatment available for spastic diplegia or any other kind of cerebral palsy. Children with spastic diplegia have a good prognosis with early intervention and appropriate therapy. The illness won’t become worse on its own, but related problems could get worse over time.
How do you treat diplegia?
Muscle relaxants and Botox both inhibit the impulses that constrict spastic muscles. This reduces transient spasticity and slows the development of contractures. Oral drugs that affect the entire body are often not optimal for spastic diplegia since the muscles in the legs are largely affected.
What are the 4 types of cerebral palsy?
The condition known as cerebral palsy (CP) comes in a variety of forms. Spastic, ataxic, athetoid (dyskinetic), hypotonic, and mixed cerebral palsy are the five basic forms. Based on afflicted body areas and movement restrictions, there are several forms of cerebral palsy.
References
- What Is Spastic Diplegia? | Levin & Perconti. (2023, March 26). Levin & Perconti. https://www.levinperconti.com/birth-injury/cerebral-palsy/spastic-diplegia/
- Horne, B. (2023, May 26). Understanding spastic diplegia cerebral palsy. https://www.medicalnewstoday.com/articles/spastic-diplegia-cerebral-palsy#risk-factors
- Otr/l, E. D. (2021, October 14). Understanding Spastic Diplegia: Causes, Symptoms, and Treatment. Flint Rehab. https://www.flintrehab.com/spastic-diplegia/#symptoms