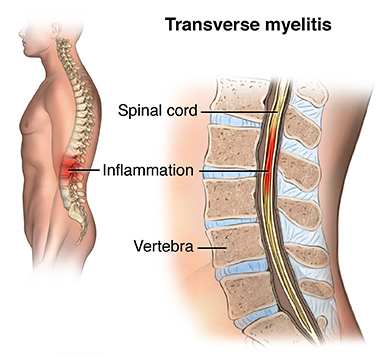
ACUTE TRANSVERSE MYELITIS (ATM)
INTRODUCTION:
Acute transverse myelitis is acute inflammation of gray and white matter in one or more adjacent spinal cord segments, usually thoracic. Causes include multiple sclerosis, neuromyelitis optica, infections, autoimmune or postinfectious inflammation, vasculitis, and certain drugs
The inflammation damages nerve fibers, and causes them to lose their myelin coating leading to decreased electrical conductivity in the central nervous system.
Transverse implies that the inflammation extends across the entire width of the spinal cord.
CAUSES of Acute transverse myelitis :
Transverse myelitis is a heterogeneous condition, that is, there are several identified causes.
Symptoms and Signs in Acute transverse myelitis :
Pain in the neck, back, or head may occur. A bandlike tightness around the chest or abdomen, weakness, tingling, numbness of the feet and legs, and difficulty voiding develop over hours to a few days.
DIAGNOSIS of Acute transverse myelitis :
Magnetic resonance imaging (MRI) uses a magnetic field and radio waves to create 3-D images of soft tissues. An MRI can show inflammation of the spinal cord, and other potential causes of the symptoms, including abnormalities affecting the spinal cord or blood vessels.
→ Lumbar puncture (spinal tap) uses a needle to draw a small amount of cerebrospinal fluid (CSF), the protective fluid that surrounds your spinal cord and brain.
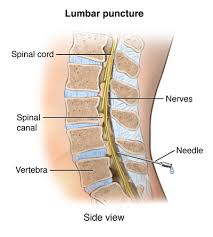
→ In some people with transverse myelitis, CSF may have abnormally high numbers of white blood cells or immune system proteins that indicate inflammation. Spinal fluid can also be tested for viral infections or certain cancers.
→ Blood tests may include a test that checks for antibodies associated with neuromyelitis optica, a condition in which inflammation occurs both in your spinal cord and in the nerve in your eye. People with a positive antibody test are at increased risk of experiencing multiple attacks of transverse myelitis and require treatment to prevent future attacks.
MEDICAL TREATMENT:
→ Intravenous steroids. You’ll probably receive steroids through a vein in your arm over the course of several days. Steroids help reduce the inflammation in your spinal column.
→ Plasma exchange therapy. People who don’t respond to intravenous steroids may need plasma exchange therapy. This involves removing the straw-colored fluid in which blood cells are suspended (plasma) and replacing the plasma with special fluids.
→ Antiviral medication. Some people who have a viral infection of the spinal cord may be treated with medications to treat the virus.
→ Pain medication. Chronic pain is a common complication of transverse myelitis. Medications that may lessen muscle pain include common pain relievers, such as acetaminophen (Tylenol, others), ibuprofen (Advil, Motrin IB, others) and naproxen sodium (Aleve.)
→ Nerve pain may be treated with antidepressant drugs, such as sertraline (Zoloft), and anticonvulsant drugs, such as gabapentin (Neurontin, Gralise) or pregabalin (Lyrica).
Medications to treat other complications. Your doctor may prescribe other medications as needed to treat problems such as muscle spasticity, urinary or bowel dysfunction, depression, or other complications associated with transverse myelitis.
→ Medications to prevent recurrent attacks of transverse myelitis. People who have antibodies associated with neuromyelitis optica need ongoing medications, such as corticosteroids and/or immunosuppressants, to reduce their chances of more transverse myelitis attacks or developing optic neuritis.
PHYSIOTHERAPY TREATMENT:
→ Stretching programme – to prevent contractures
→ Strengthening

→ Transfers
→ Gait training

→ Wheelchair training

→ Reduce the risk of pressure ulcers
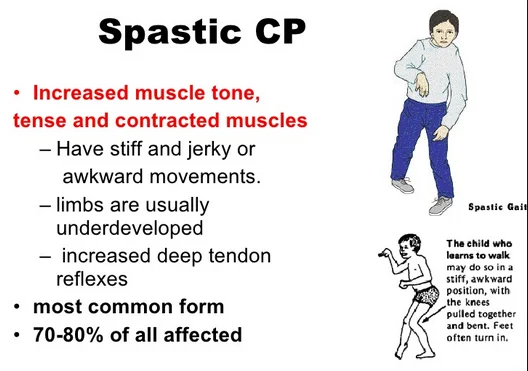
→ Aid control of spasticity
→ Pain reduction/management
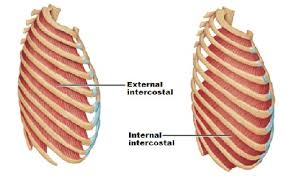
→ Breathing exercises and chest clearance techniques
→ Joint care
→ Pain control





2 Comments