Ankle Pain While Walking
What is an Ankle Pain While Walking?
Ankle pain while walking can significantly impact an individual’s daily activities, mobility, and overall quality of life. The ankle joint plays a crucial role in supporting body weight and facilitating movement, making any discomfort during walking a cause for concern. Various factors can contribute to ankle pain, ranging from acute injuries and overuse to chronic conditions and underlying medical issues.
To accurately diagnose and effectively treat ankle pain, people must be aware of the possible causes and seek medical attention as soon as possible. This will help them regain their mobility and reduce the likelihood of long-term complications.
Overview
Our ankle is a complicated structure made up of bones, ligaments, tendons, and cartilage. When you stand, walk, or run, it supports your body weight. It is quite common for injuries or conditions to affect the ankle and this can cause pain when walking.
What are the parts of the ankle?

A component of the musculoskeletal system is your ankles. They aid with standing, balancing, and movement by supporting your body weight. A flexible ankle allows you to direct, bend, rotate, and move your foot from side to side.
The lower leg bones (tibia and fibula) meet the foot bone (talus) to form the ankle. Ligaments hold these bones together.
The foot and ankle are capable of movement due to the intricate arrangement of tendons, muscles, and other soft tissues. The ankle is especially vulnerable to injury due to its intricacy.
What is Ankle Pain?
Any kind of pain or discomfort that affects any area of the ankle is referred to as ankle pain. Jumping pain can occur for several reasons. The most common causes are injuries, arthritis, and normal wear and tear. You could have stiffness or soreness anywhere near your ankle, depending on what’s causing it. Also, the ankle may swell and you may not be able to put weight on it.
Ankle pain usually resolves with rest, ice, and over-the-counter pain relievers. Both arthritis and injuries can be treated by medical professionals. The diseases can frequently be managed without surgery. Surgery is required, though, if the injury is severe—such as a broken ankle—or if non-surgical treatment does not alleviate the discomfort in the ankle. A physical therapy (PT) regimen can also aid in your recovery if you’ve had surgery or an ankle injury. PT helps to strengthen the ankle and foot supporting muscles. Both pain relief and injury prevention are possible with therapy.
What is ankle pain when walking?
The ankle joint is one of the most complex and busy areas of the body. It has 26 bones and 33 small joints, all held together by a network of soft tissues that also consist of muscles, tendons, ligaments, nerves, and blood vessels. Most cases of foot or ankle pain are short-lived and are caused by soft tissue damage, namely a sprain or strain.
It supports body weight while standing, walking, and running. It is quite common for injuries or conditions to affect the ankle and this can cause pain when walking. Ankle pain refers to any pain or even discomfort that affects any part of the ankle joint. Ankle pain usually resolves with home treatment, ie. rest, ice, and over-the-counter pain relievers. A physical therapy program can help the patient strengthen muscles and prevent further injuries.
Doctors treat more severe pain with braces and splints or with injections and surgery. In addition, the most common causes of ankle pain are injuries, arthritis, and normal wear and tear. Depending on the cause, the patient may feel pain or stiffness somewhere around the ankle. The patient’s ankle may also be swollen and the patient may not put any weight on it. Often, mild diseases can be treated without surgery.
On the other hand, surgery is required if the injury is severe—such as a broken ankle—or if non-surgical treatment does not alleviate the ankle pain. If a patient has had an ankle injury or even surgery, a physical therapy (PT) treatment plan can help the patient recover. A physical therapist strengthens the muscles that support the legs and ankles. Physical therapy can relieve pain and prevent future injuries.
How common is ankle pain?
Ankle pain and ankle injuries are very common. You are likely to have ankle pain if:
- You’ve reached the age of 65.
- Play sports or practice activities that involve jumping, lateral movements, or rapid changes of direction.
- You are overweight/obese.
Possible reasons
Which factors lead to ankle pain the most frequently?
The causes of ankle disorders are varied and can include running, jumping, and overuse. Other typical reasons for fractures and sprains of the ankle include:
- Beyond the ankle’s usual range of motion by twisting or rotating it
- Tripping or falling
- Landing on the leg with increased force
A multitude of ailments and injuries can result in ankle pain. Ankle discomfort is frequently caused by a number of common injuries, which include:
- Bursitis: Fluid-filled sacs called bursae to cushion the bones during movement. Bursitis occurs when these sacs are irritated and inflamed.
- Fractures: Bones may break as a result of an accident or injury (fracture). Ankle fractures range from mild to severe. Broken ankles can involve the bones of any part of the ankle joint. A broken ankle causes swelling and pain in the ankle.
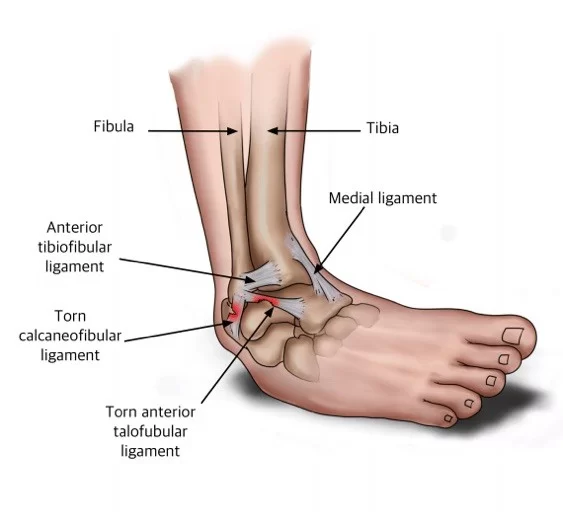
- Sprains: Ankle sprains are a common cause of ankle pain. An ankle sprain occurs when ligaments are stretched or torn. An ankle sprain or sprain occurs when the ankle is forcefully rolled out of its normal position.
- Tendinitis: Irritated, inflamed tendons are a soft tissue injury called tendinitis. Tendons connect muscles to bones. The tendon may occasionally rip (as in the case of an Achilles tendon rupture). It could require surgery to mend a damaged tendon.
- Bruising: When walking, your ankle may hurt if it has been seriously bumped, perhaps by a hit or kick. This kind of trauma usually has a two- to three-week resolution to its agony.
Ankle discomfort can also result from a variety of illnesses, ailments, and situations. They include:
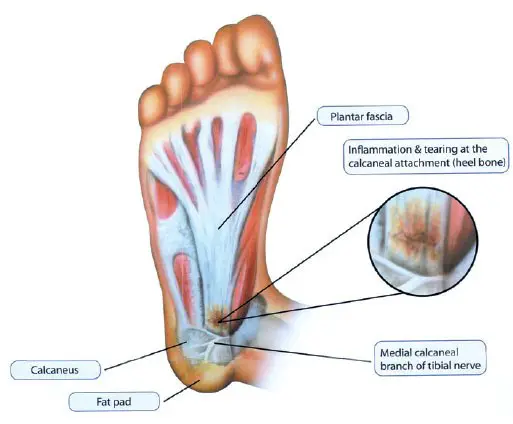
- Plantar Fasciitis: This condition is a band of tissue (fascia) that connects the heel bone to the bottom of the toes. As you walk, it cushions your foot’s arch and reduces impact. Tension, as well as tension in the fascia, can cause small tears in the joint. Repeated stretching and tearing of the face can irritate or inflame it, although in many cases of plantar fasciitis, the cause remains unclear.
- Pseudogout: This is a form of arthritis characterized by sudden painful swelling in one or more joints. This condition can cause pain for days or weeks. The ankle and knee joints are most frequently affected when dealing with this disorder. Also called calcium pyrophosphate deposition disease or CPPD, the more common term “pseudogoth” was coined from the condition’s similarity to gout. Crystal deposits in the joint cause both conditions, although the type of crystal is different in each condition. It is not clear why crystals form in the joints that can cause pseudogout. But the risk increases with age.
- Rheumatoid arthritis: This condition is a chronic inflammatory disease that can affect more than just the joints. In some patients, the condition can affect many different body systems, including the skin, eyes, lungs, heart, and blood vessels. An autoimmune disease, rheumatoid arthritis, occurs when the immune system mistakenly attacks the body’s own tissues. Unlike the wear and tear caused by osteoarthritis, rheumatoid arthritis affects the lining of the joints, causing painful swelling that can eventually lead to bone erosion and joint deformities. The inflammation associated with rheumatoid arthritis mainly affects other parts of the body. Although new types of drugs have greatly improved treatment options, even severe rheumatoid arthritis can still cause physical disability.
- Septic arthritis: Septic arthritis is a painful joint inflammation that can be caused by bacteria traveling through the bloodstream from another part of the body. Septal arthritis can also occur when a penetrating injury, such as an animal bite or trauma, carries bacteria directly into the ankle. Babies and older adults are most likely to have septic arthritis. There is also a risk of septic arthritis in people with artificial joints.
- Arthritis: Ankle pain and stiffness can be caused by ankle arthritis. Arthritis occurs when cartilage (the joint tissue that cushions bones) breaks down. The decay causes the bones to rub together. Injuries and overuse can cause arthritis, and it’s more common in people over 65. The ankle can be subject to a variety of arthritis all kinds. The degeneration of cartilage in the joints is a consequence of the above. Common types are rheumatoid arthritis and osteoarthritis. Osteoarthritis is among the most frequent kinds of arthritis. This can be the cause of ankle pain, especially if the patient is older, overweight, or even has a history of an ankle injury.
- Peripheral neuropathy: Damage to the patient’s peripheral nerves and can cause pain in the ankles when walking. Nerve damage can be caused by tumors, trauma, infections, or even diseases.
- Gout: A type of arthritis, gout is caused by a build-up of uric acid in the body. Normally, uric acid leaves the body with urine. Excess uric acid forms crystals that settle in the joints. A drop in the ankle joint can be very painful. Gout is one type of arthritis. This condition occurs when uric acid does not dissolve in the blood as it should. Rather, it solidifies into crystals, gathers in the joints, and may be painful. Big toe discomfort is the most common place for patients to experience pain, which can later spread to the ankle, heel, and other joints.
- Infection: Many types of infection, including cellulitis, can cause ankle swelling and pain. A bone infection called osteomyelitis can be caused by staph. If the patient is ill, irritable, and feverish with ankle pain, the patient may have an infection. The joint is susceptible to becoming exposed to heat, red, and swollen. In order to drain the fluid from the ankle or perform tests, the doctor could use a needle. To eradicate the germs, the patient might be prescribed medicines.
- Peripheral neuropathy: Damage to the peripheral nerves can cause pain in the ankles when walking. Nerve damage can be caused by tumors, trauma, infections, or diseases.
- Chronic ankle instability: Chronic ankle instability occurs when a patient has had multiple sprains or other ankle injuries. As a result of ankle injuries, the ligaments surrounding the ankle joint are weakened, and their job is to keep the ankle joint stable and supported. Over time, this can lead to pain and soreness when the patient walks, as this is when these ligaments need to be tightened to prevent the ankle from rolling. If a patient has unstable ankles, they may find that the pain worsens when walking on uneven ground.
- Sinus tarsus syndrome: Sinus tarsus is simply the term between the two bones below the ankle, towards the outside of the foot. Sinus tarsi syndrome describes a condition where damage to the tunnel or tunnel ligaments, blood vessels, or even the nerves surrounding the tunnel can cause certain symptoms such as pain, burning, tingling, or even weakness in the ankle. Treatment for sinus tarsus syndrome may include helping to keep the foot in an optimal position to allow the damaged structures to heal.
- Flat Feet: Posterior Tibial Tendon Dysfunction: When a patient has flat feet, they are naturally more prone to a painful condition called Posterior Tibial Tendon Dysfunction (PTTD). The posterior tibial tendon is a tendon that runs along the inside of the lower leg, crossing the inside of the ankle. It plays a large and important role in keeping the patient active and mobile. When the tendon is damaged, often from overuse associated with flat and unsupported feet, the pain is usually felt on the inside of the ankle. Treatment for PTTD involves helping the damaged tendon to heal to relieve ankle pain and supporting the flat foot so that the flat foot position does not re-injure the tibial tendon in the near future. Ankle and foot pain and edema may be brought either by an extremely low arch or by no arch at all. Sometimes children’s arches do not develop normally as they grow, leading to disease.
- Cutaneous muscles: Cutaneous muscles are basically a deformity of the big toe. Patients with club toes have an outward pointing toe and a bump on the inside of the foot. As the joint muscle grows and calluses form, it may force the patient to shift weight to avoid pain when the patient walks.
- Lupus: This condition is an autoimmune disease that causes the body to attack healthy tissues. Lupus patients often have joint pain, including ankle pain. This results from concurrent tendinopathy and arthritis which are associated with lupus. Additionally, renal issues brought through lupus can result in fluid accumulation in the joints. There is no cure for lupus, still, the doctor can give medications to the patient to keep it under control. Timely physical activity and a nutritious diet are additionally beneficial.
- Persistent lateral ankle pain: Pain that persists on the outside of the ankle joint might have several causes. It is probably the consequence of the ligament, which remains weak after improper healing following a sprain. This makes the entire joint less stable as well as leads to more injury and pain as well.
- Stress fracture: In this condition, tiny cracks in the bones may occur. It is brought on by repetitive force, which is frequently from overusing the bones and joints, such as when one continually runs large distances or jumps up and down. Additionally, normal use of the bone that has been weakened by an illness like osteoporosis can result in stress fractures. This type of fracture occurs most often in the weight-bearing bones of the foot and ankle. Athletes and soldiers who carry heavy luggage over long distances are most at risk, but anyone can develop a stress fracture. For example, if you start a new exercise program, the patient may develop stress fractures if the patient exercises too much too soon.
- Osteochondral injuries of the talus (OLT): a sudden injury, such as a sprain, can damage the cartilage of the talus (calcaneum) or cause fractures, blisters, or even ulcers in the underlying bone. Several months after treatment of the injury, the patient may notice that the ankle is stuck or locked or even painful, which may be an osteochondral lesion of the talus.
- Reactive arthritis: This type usually follows an infection in the GI tract or urinary tract. Knees and ankles are two of the first areas that are susceptible to it. Antibiotics are what are administered by the physician to treat the infection. Exercise will keep the joints flexible. The arthritis should go away within a few weeks or months.
- Scleroderma: This group of diseases causes thickening of the skin and connective tissues. If it affects the tissues surrounding the joint, the patient may feel pain and stiffness. It can also weaken muscles and cause digestive, heart, and kidney problems.
What causes back ankle or heel pain when walking?

Pain in the back of the ankle, similar to pain in any part of the ankle, can be caused by a fracture, sprain, or twist. However, some specific conditions are more likely to cause pain in the back of the ankle or heel.
Achilles tendon ruptures Achilles tendon tears usually occur when you are active or participate in vigorous sports. It arises whenever there is a break or tear within the Achilles tendon. This is most likely due to an injury, such as falling while walking or running on uneven ground, or accidentally stepping into a hole.
Symptoms include:
- Calf pain
- Pain and edema in the vicinity of the heel
- Inability to bear weight on your toes
Hair loss prevention can include:
- Running on a softer flat surface
- Avoid rapid increases in exercise intensity
- Stretching before training
Heel bursitis: A bursa is a pocket and lubricant that acts as a cushion around a joint. It has a bursa that protects the back of the ankle and the heel. This will help protect your Achilles tendon. It can burst from overuse or strenuous activity.

Symptoms include:
- Pain in the heel area
- Discomfort in the toes when standing
- Swollen or reddened skin on the back of the heel
Treatment includes:
- Avoid painful activities
- Ice or cold pack
- Acetaminophen (Tylenol) or ibuprofen (Advil, Motrin) are examples of over-the-counter pain medications.
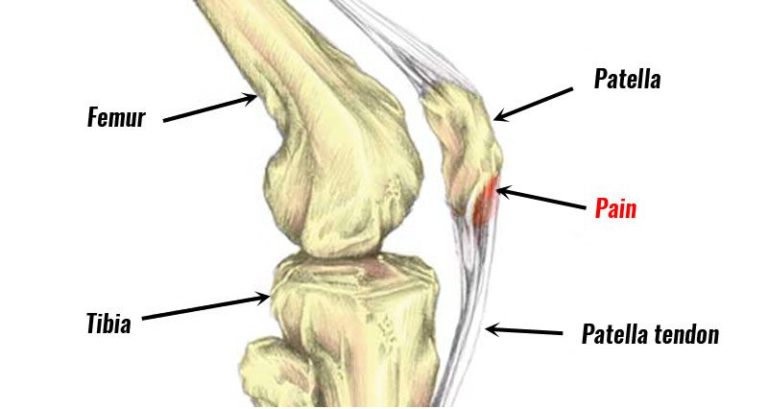
Achilles tendinitis: Along with a tear, Achilles tendinitis is caused by damage to the Achilles tendon. Overuse or strong exertion can stretch the ligament connecting the calf to the heel bone, causing tendinitis.
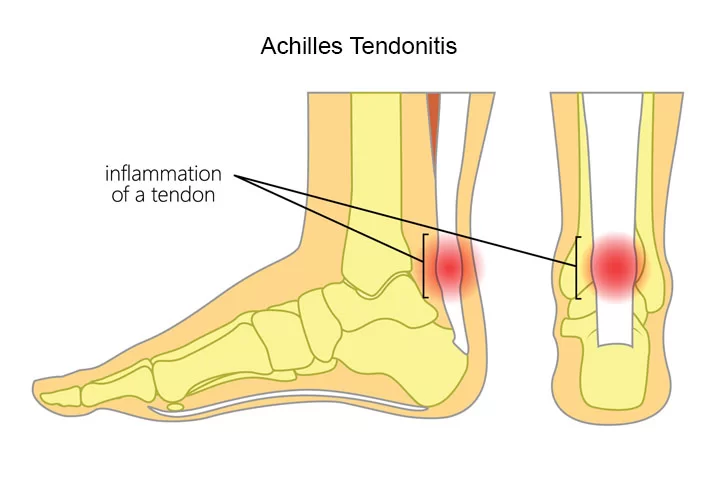
Symptoms include:
- Rigidity
- Tenderness
- Mild to severe pain in the back of the ankle and lower leg
Rest and self-care techniques like elevation and hot or cold compresses are part of the treatment.
What are the symptoms of ankle joint disease?
Symptoms of ankle joint disease vary depending on the type of injury. Common symptoms include:
- Pain
- Swelling
- Rigidity
- Problems with movement of the ankle
- Inability to put pressure on the ankle
- Walking difficulties
- Bruises
Tendonitis and Achilles tendinitis can cause similar symptoms but can include:
- Pain in the back of the heel that gets worse during the day
- Thickening of tendons
- Swelling that worsens with physical activity
- Strong popping sounds at the back of the heel, indicating a tendon tear; if this happens, seek emergency care.
A few unique tests for walking-related ankle discomfort
Anterior drawer test:
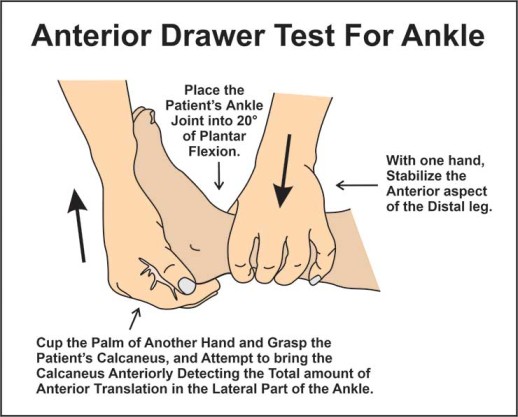
To detect an anterior ankle ligament injury: First, the patient is supine, with the ankle flexed 20° after resting the heel on the therapist’s palm, which is supported by a table. The therapist should then stabilize the heel bone. After that, the therapist stabilizes the tibia and fibula by pulling the bone and observes from the front the amount of anterior translation of the lateral part of the ankle and the change in final sensation.
The amount of anterior translation the final impairment of final sensation and the change from a hard ligament to a weak elastic one are noted. Anterior translation greater than one centimeter relative to the normal contralateral ankle and obvious loss of head sensation is best indicative of a partial or complete tear of the anterior talofibular ligament of the ankle.
Astragalus tilt test:
To determine possible damage to the anterior talofibular ligament and ligament. Initially, the patient sits on the unsupported leg and ankle. The foot position is 10-20 degrees of plantar flexion. The distal lower extremity is stabilized with one hand proximal to the ankle and the hindfoot is rotated with the other hand. The lateral side of the talus is palpated to determine if there is bowing. The slack is compared in the other direction.
Compression test:
The compression test initially compresses the proximal fibula against the tibia to assess the integrity of the bones, interosseous membranes, and syndesmotic ligaments. In the event of a fracture or diastasis, pain is considered advantageous. In the event of a fracture or diastasis, pain is considered advantageous.
First, the patient is in a sitting position, the knee is bent 90 degrees and the ankle is relaxed. After that, the examiner should sit at the level of the tested ankle with a strong hand stabilizing the leg from behind, and the other hand grasps the ankle in a normal position and then makes the leg outside. If there is pain in the area of the interosseous membrane or even medically. The pain can radiate up the leg, depending on the severity and extent of the injury, the test is positive.
Ankle prick sign:
Initially, the examiner is in a sitting position facing the patient. The examiner holds the calcaneus with the hand on the lateral side of the foot, the fingers around the colon, and the thumb over the anterolateral aspect of the ankle joint. The medial hand also grasps the front of the foot. The foot is held in plantar flexion.
By applying pressure with the probing thumb, the foot is brought from plantar flexion to full dorsiflexion. If the pain of the movement, together with pressure and pain in the thumb, is greater in dorsiflexion than in plantarflexion, the test is positive. If the pain does not improve with the combined movement, the test is negative.

Cotton test:
This test is done to detect syndesmotic instability of the joint. This is a manual stress test that detects lateral movement of the talus when the ankle is dead. The doctor stabilizes the proximal ankle by moving the talus laterally. A positive test is characterized by an increase in the range of motion compared to the healthy side and indicates a sprain of the distal tibiofibular syndesmosis or even subtalar joint.
Coleman Blocking Test:
With this test, the therapist can assess the flexibility of the rear foot and the pronation of the forefoot. At first, the initial deformity is in the leg, followed by changes in the hind leg. The examination is performed by placing the patient’s foot on a 2.5-4 cm thick wooden block with the heel and lateral edge of the foot resting on the block and bearing the weight of the whole body, with the first, second, and third metatarsals allowed to hang freely for plantar flexion and pronation.
The test result is based on the assumption that the flexion of the first metatarsal is fixed. This test excludes the influence that the forefoot (1st metatarsal during plantar flexion) may have on the stance phase of the hindfoot. If the heel is correct when the patient stands on the block, the hindfoot is considered flexible, if the subtalar joint is flexible and the Coleman block test is correct, surgical procedures can be directed at correcting the pronation of the forefoot, which is usually. due to plantar flexion. . of the first metatarsal. if the hind leg is stiff, then surgical correction of both front and hind legs is required.
Eversion stress test:
The eversion stress test evaluates the integrity of the brachial ligament and helps determine the degree of instability after a medial ankle sprain. First, the patient is in a supine position, on his side, or sitting comfortably, the knee must be at a 90-degree angle, and the gastrocnemius muscle must be relaxed. The physiotherapist holds the heel with one hand and the lower leg with the opposite hand.
Keeping the ankle in a normal position, the doctor applies an abduction force to the calcaneus bone to tilt the talus. Increased talar tilt or even pain in the deltoid ligament on bilateral comparison indicates a positive test. A soft or even vague final sensation indicates a complete tear. In the normal position, a tilt of 2 degrees or more during testing, when compared bilaterally, indicates a high probability of knee ligaments.
Navicular Drop Test (NDT):
First, instruct the patient to assume an upright position with the lower limbs fully weight-bearing, and ensure that the foot is in the normal position of the subtalar joint. Mark the most visible area of the navicular tubercle and measure its distance from the supporting surface (floor or even a step). Ask the patient to relax and then use a ruler to measure the sagittal movement of the navicular.
Alternatively, the test can be performed in the opposite position, for example measuring from a relaxed position to a normal standing position. Many examiners also choose to perform this test by marking the initial and final position of the navicular on an index card on the inside of the foot and then measuring the change with a ruler.
Posterior box test:
This ankle test is used to test for posterior talofibular ligament injury and ankle ligament instability. First, ask the patient to lie supine with the knee slightly flexed to neutralize the pulling force of the gastrocnemius muscle of the lower extremity. When the ankle joint is held 10-15 degrees below plantar flexion, the Therapist grasps the heel with one hand and stabilizes the front part of the tibia with the other hand.
After that, ask the patient to relax the muscles, in which case the examiner moves the leg backward from the ankle joint, holding the tibia with the other hand. Positive test – if there is no terminal sensation and the proximal tibia falls back (excessive translation). The amount of posterior movement determines the degree of a PCL tear.
How does my provider determine the cause of my ankle pain?
Your foot and ankle will be examined by your physician. Providers will check for swelling, pain, and bruising. Testing depends on the location of the pain and whether you have had a recent injury. Your provider may order an imaging test, such as an X-ray, CT (computed tomography), or MRI (magnetic resonance imaging). These tests create images of the bones and soft tissues so your provider can check for damage. If your provider suspects you have an infection, you may need a biopsy. Your provider will take a tissue sample and send it to a lab for bacteria.
During the physical examination:
The doctor examines the patient’s ankle, foot, and lower limb. The doctor will touch the skin area around the injury to check the exact pain points and move the patient’s leg to check the range of motion and find out which positions cause discomfort or pain in the ankle. If the injury is severe, your doctor may recommend one or more of the following imaging tests to determine the fracture or even assess the extent of ligament damage:
X-ray:
During an x-ray, a small amount of radiation passes through the patient’s body to create images of the bones of the entire ankle joint and surrounding areas. This test is best for detecting fractures.
Magnetic Resonance Imaging (MRI):
MRI mainly uses radio waves and a strong magnetic field to produce detailed cross-sectional or 3-D images of the soft tissue inside the ankle joint, including the ligaments.
Computed tomography (CT scan):
Computed tomography allows the doctor to obtain more information about the bones in the ankle joint. A CT scan takes X-rays from multiple angles and mixes them to create cross-sectional or 3D images.
Ultrasound (USA):
Sound waves are used in ultrasound to create images of the ankle. These images can help the doctor determine the condition of the ligament/tendon when the leg is in different positions.
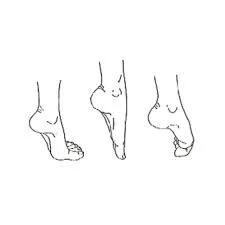
A walk
A gait cycle is the time interval between two consecutive occurrences of a single repetitive movement event. The human gait cycle is divided into two distinct periods, representing the period when the foot is in contact with the floor, called the stance phase, and the period when the lower limb is not in contact with the floor called the swing phase. In the standing phase, the foot touches the floor, the body mass is supported, and then the body is pushed forward in the later stages of the stance.
There are five events in the stance phase: 1) heel strike (HS), 2) foot flat (FF), 3) mid-distance (MS), 4) heel rise (HO), and 5) toe off (AL).
- Heel strike: The initial moment of the human gait cycle is the first contact of one foot with the floor, often referred to as heel strike or foot strike.
- Flat foot: The point at which the rest of the foot contacts the floor and is usually where the entire weight of the lower leg is supported.
- Middle height: This pitch is determined when the center of gravity is directly above the center of the ankle joint. It is also used when the center of the hip joint is above the ankle joint.
- Heel Release: Heel release occurs when the heel begins to lift off the floor in preparation to propel the body forward.
- Toe-off: Toe-off occurs as the last contact during the stance phase.
The various events of the gait cycle occur in a remarkably similar sequence and are independent of time. Therefore, the stride cycle is usually described as a percentage rather than as elapsed time. The initial heel strike is 0% and the next heel strike on the same foot is 100% (0-100%). During a normal gait cycle, the hip, knee, and ankle joints experience a range of motion. Illustrates these ranges of motion at different speeds.
Hip movements can be classified into two main movements: first, hip extension, which occurs in the stance phase and whose main function is to stabilize the body, and second, hip flexion, which occurs in the swing phase. In the stance phase, the knee is the main factor in the stability of the lower limb, and in the swing phase, the knee flexibility is the main factor in the freedom of movement of the limb. In the middle phase, the entire body weight is transferred to the bent knee. The range of motion of the ankle joint is not great, but it is crucial for progression and shock absorption during stance.
Walking cycles and stages
The human gait cycle begins when one foot touches the floor and ends when the same foot touches the floor again. The gait cycle can be divided into periods and phases to define normal and abnormal gait. In most cases, the gait cycle is divided into two periods, stance and stride. The period of time the foot is in touch with the floor is known as the stance phase. The swing phase follows the stance phase and is the time during which the same leg is in the air. The separation of the two phases can be seen at the top.
If the position of the other or opposite leg is considered, the stance period can be further divided into three sub-periods. The first double leg rest is the part during which both feet are in contact with the floor. One leg support is the subperiod during which one or the opposite leg is in the air. The final double leg is the section during which both legs are back in contact with the floor.
The stance cycle represents the first 60% of the step cycle and the swing the last 40%. The initial bipedal stance represents the first 10% of the gait cycle, the single-leg stance represents 40%, and the final bipedal stance completes the stance phase for the second 10% of the gait cycle. The duration of consecutive periods of standing, swinging, and bipedal periods is similar for repeated trials of the same walking path and the same goal.
However, speed can affect percentages for stance sub-periods, where increasing speed decreases two-leg support periods and increases single-leg support. Eventually, as the person resumes moving faster and starts running, the periods of double leg support disappear. On the other hand, reducing your walking speed has exactly the opposite effect.
Inman, Ralston, and Todd, 1981, can also divide the gait cycle into functional phases. Levine et al., 2012; Perry and Burnfield, 2010; Roos and Danger, 2005). The following steps follow from this approach:
- Initial contact (0-2% of gait cycle): This phase is the beginning of a load response or acceptance of weight. This is also the beginning of the stance phase and the first part of the bipedal stance phase. In the initial contact phase, the person also has collision phenomena that appear in the very early phase of ground reaction forces.
- Load response (2-12% of the gait cycle): This phase is the initial bipedal support phase. In this phase, the person continues and completes the weight-receiving task. In terms of front-back force, a person has the smallest (or largest) brake tip.
- Mid-distance (12-31% of gait cycle): Mid-distance is the first part of the stance cycle of one leg. The main theme is stability because the base of support is greatly reduced and the center of gravity (COG) moves to the highest point when the legs extend and transfer kinetic energy into potential energy. The end of this period is characterized by the appearance of a “valley” or even a local minimum of the vertical bottom reaction force.
- Final stance (31-50% of gait cycle): The final stance is the second part of the stance cycle of one leg. Stability is still a concern and the heel strikes the other foot. The center of gravity (COG) “falls” from its highest point and potential energy is transferred to kinetic energy.
- Eelswing (50-60% of the stride cycle): This is the two-legged final support period plus our second loading period. According to vertical ground reaction force (VGRF), a person has a second load peak or even a second local maximum, or a second “hump”. During this phase, the person also has a maximum thrust in terms of front-back force, because the person is preparing to push our feet off the floor.
- Initial Swing (60-73% of the stride cycle): This phase is the first part of the swing cycle and our main task is to clear the ground by flexing the entire leg. Full flexion reduces the moment of inertia of the leg and increases the angular velocity of the swinging leg.
- Midstroke (74%-87% of the stride cycle): This phase is the second part of the swing cycle, and our biggest concern is that the opposite or opposing leg has little support in one stance. stability is a concern. We also prepare for the next leg contact at the end of our swing.
- Final Swing (85-100% of the stride cycle): This phase is the third and final phase of the swing cycle and our biggest concern is future foot contact.
Treatment and care
What can I do to relieve ankle pain?
If you have severe ankle pain while walking, you should see a doctor. You likely hurt your Achilles tendon or ankle. If your pain is mild and you remember twisting your ankle or tripping, you may have a sprain. If you use ice, elevate the area, and obtain sufficient rest, they normally cure in one to two weeks. Talk to your doctor if your pain persists or if you are concerned. If lifestyle changes and OTC treatments just don’t reduce pain, it may be time to look at other options.
An orthotic shoe or foot or ankle support is an excellent non-surgical way to realign joints and reduce pain and discomfort. Available in different sizes and degrees of stiffness, the inserts support different parts of the foot and distribute the weight of the body, which relieves pain. The ankle support works the same way. There are several sizes and amounts of support accessible for these braces.
Some can be worn with regular shoes, while others are a little more roomy and look like casts that cover both the ankle and the foot. Although some varieties may be available at the pharmacy or pharmacy, it is best to consult a doctor to ensure the correct fit. Injections of steroids are commonly utilized to lessen inflammation and pain.
A medication known as a corticosteroid is thrust into the area of concern during the injections to relieve pain, stiffness, and edema. The majority of injections require only a few minutes, and the effects usually show results within hours or three months. The best part is that it is a non-invasive, non-surgical procedure that allows you to rest at home the same day. Most ankle pain improves with rest, ice, and OTC pain relievers.
Follow your provider’s instructions for home care for ankle pain. The RICE approach (rest, ice, compression, and elevation) is often said as a result of your healthcare physician. If the pain is severe or the ankle still hurts after a few days of home treatment, Over-the-counter pain reliever: Nonsteroidal anti-inflammatory drugs (NSAIDs) can relieve pain and reduce swelling. Consult a healthcare provider starting any new medicine. Contact your service provider.

The most common home remedies for ankle pain are:
- Rest: If you have had an injury, such as a sprain, you should rest on your feet for a while. Consult your healthcare practitioner about the ideal amount of rest. Walking sticks or walking boots help you move without straining your ankle.
- Ice: Apply ice or a cold pack to the area for 15-20 minutes every few hours to reduce swelling.
- Compression: Ask your provider how to wrap an elastic bandage around your ankle to reduce inflammation. If you can, attempt not to encase it too tightly.
- Elevation: Resting the ankle above the heart reduces swelling. You can also try sleeping with your legs elevated at night.
- Supportive footwear: Make sure your shoes provide adequate foot and ankle support. Overly loose shoes, sandals, and flip-flops should be disregarded. When you play sports, it is essential to wear appropriate shoes. Activities such as basketball and volleyball can cause ankle injuries, especially without proper footwear.
Treatment depends on your condition and symptoms. Treatment may include non-surgical and surgical options. Non-surgical options include:
- The use of drugs that reduce swelling and inflammation, such as aspirin or ibuprofen
- Rest and raise the ankle
- Use ice packs to reduce swelling
- Use compression bandages or casts to immobilize the ankle
- Have a cortisone (steroid) injection to reduce pain and swelling
Severe fractures or tendon tears may require surgical treatment. Several different surgical techniques serve to treat ankle disorders:
- Reconstruction to restore the bones, joints, tendons, and ligaments of the ankle
- Removal of damaged tissue (incontinence)
- Lengthening the calf muscles to reduce pressure on the Achilles tendon
- Fusion of bones in the ankle joint to keep it stable (arthritis)
- Ankle joint replacement (joint surgery)
How do healthcare providers treat ankle pain?
Most ankle injuries heal with home care. More serious injuries may require surgery. The cause of the ankle discomfort will impact how it is dealt with. Common treatments for ankle pain include:
- Braces and Splints: An ankle brace can relieve pain and stabilize the ankle. Certain braces are better for certain activities. Ask your provider to recommend one that best fits your lifestyle.
- Joint aspiration: the healthcare provider is going to employ a needle to drain extra fluid from the joint during this treatment. Joint exercises relieve pain and swelling.
- Medications: Several medications can reduce inflammation and relieve ankle pain. Arthritis and gout medications can significantly reduce pain and swelling.
- Orthopedic insoles: Orthopedic insoles adapt to your shoes. You can buy them in a store, or your provider can customize them for your feet. Orthotics support and stabilize the foot ensuring correct orientation.
- Physical Therapy (PT): A personalized PT program helps improve flexibility and strengthen the muscles that support your ankle. Your physical therapist will create a PT plan that includes exercises and stretches just for you. Remember to do the prescribed exercises and stretches regularly.
- Steroid injections: Your provider will inject an anti-inflammatory medication directly into your joint with a needle. Cortisone injections reduce inflammation and pain.
- Surgery: A wide variety of ankle surgical procedures can be used to repair torn ligaments or tendons. Some options relieve arthritis pain or correct flat feet. Ankle replacement surgery can relieve pain and restore function.
How does physical therapy help?
If you have an acute injury, x-rays are usually needed for diagnosis. Sprains or strains are usually initially prescribed R.I.C.E treatment, also known as “rest, ice, compression, and elevation”. Fractures are usually different but require different treatments. If the pain and swelling are severe, you may also be given an anti-inflammatory medication. If a chiropractic adjustment is necessary, it is delayed until the original trauma has subsided.
Physical therapy, however, can normally begin immediately regardless of the severity of your injuries. Before coming up with a treatment plan for you, your physical therapist will consider your condition, symptoms, medical history, and physical goals. Your physical therapist may next recommend non-weight-bearing activities like these once this has been determined.
- “Toe drawing.” Your physical therapist may have you “draw” letters of the alphabet with your toes.
- Inversion/eversion. This exercise requires you to point your feet either to the left or right.
- Resistance training. This is usually done with a TheraBand around the leg.
- Isometric exercises. These are gentle exercises used to build muscle strength in the ankle. Stop ankle pain with us!
Your physical therapist may also perform special physical therapy procedures, such as manual therapy, ice and heat treatments, ultrasound, or massage, at their discretion. They all aim to relieve pain, promote healing, and improve range of motion. If you are concerned about your ankle pain, call us today. Our highly trained physical therapists can help you safely and effectively rehabilitate your ankle.
Physiotherapy treatment
Electronic categories
- This treatment helps the patient reduce ankle pain, relieve nerve pain, accelerate the healing of muscle injuries, increase blood circulation in the body, heal wounds, and relax muscle spasms.
- Ultrasound (US): The US mainly reduces pain in soft areas.
- This method, known as transcutaneous electrical nerve stimulation (TENS), is utilized to reduce swelling, redness, and pain.
- Wax therapy: The primary benefit of this technique is pain relief for the patient.
Exercises
Daily one or two sessions of exercises may help the patient to relieve pain and strengthen the muscles.
Stretching exercise:-
In the starting phase do some stretching exercises. It may improve performance in physical activities, decrease the risk of injuries, help the joints move through their full range of motion, increase muscle blood flow, enable the muscles to function at their peak efficiency and enhance daily activity performance.
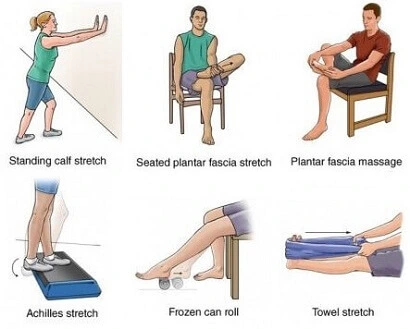
Achilles tendon and plantar fascia stretch: First, tell the patient to wrap a towel around the foot and pull it back toward the body so the knees are straight. Hold for 30 seconds with one repetition, do three repetitions in one session. Do three exercises per set
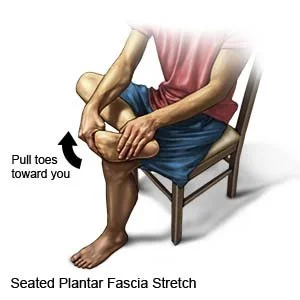
Sitting plantar stretching exercise: First, the patient is instructed to cross the leg over the contralateral knee, from the bottom of the toes to the floor, and gently pull back until the patient feels a stretch in the lower leg. Hold for 30 seconds per rep. Do three sessions per set, and repeat three times in a single session. Do two sets a day.
Standing Floor Stretch: The patient should stand facing the wall and then place both hands on the wall in front of the patient. Place one foot in front of the opposite foot so that the front foot is about 30 cm from the wall and keep the back knee straight and the heel straight on the ground. Bend the front knee slowly until the patient feels tension in the back of the leg, after 30 seconds of extension return to the normal position, repeat three times during the session. Do three sessions a day.
Deep calf stretch: The patient should stand on a step with the heel hanging over the edge. The patient can hold something for support, then allow the patient to drop the heel to the ground and feel the stretch in the calf muscles and Achilles tendon. Hold this position for 30 seconds. In a single session, repeat this exercise three times. Do three sessions a day.
How to do the towel in stretch exercise: First, ask the patient to sit while placing a towel or bandage around the affected leg. Then hold both ends of the towel with the patient’s hands. Slowly rotate the ankle inward as if the patient were facing the sole of the foot. Then pull the towel up with your whole arm to deepen the stretch. On the other hand, the patient has a problem. Hold for 30 seconds per rep. Perform one set of three repetitions per session. Work out three times a day.
Towel Stretching Exercise: First ask the patient to sit down by placing a towel or even a bandage around the affected leg. Then hold both ends of the towel with the patient’s hands. This time, slowly turn the ankle outward, just as the patient faces the affected leg with the sole. Then pull the left side of the towel up to deepen the stretch. Repeat on the other side when it is tight. In one session, try to hold these stretches for 30 seconds and repeat the sequence three times. Do three sessions a day.
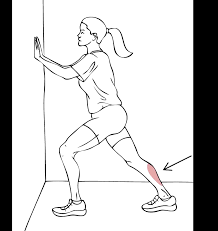
Standing Calf Stretch: To increase the stretch, the patient can move to a standing position: Stand upright against a wall or other support such as a chair, with one foot about 12 inches in front of the patient. Point your toes up. Slowly bend forward until the patient feels a stretch in the back of the leg. Hold this stretch for 30 seconds and then repeat the stretch on the other side. Do a total of 3 rounds.
Cross Ankle Stretch: First, tell the patient to sit comfortably with the left leg crossed over the right knee. Then hold the right leg with your hands, then use your right hand to bend the left toes and ankle down as the patient points the toes. The patient should feel this stretch in the ankle and forefoot. Repeat on the other side after holding this stretch for 30 seconds. Repeat three times during the session in one set. Do two exercises and two sets per day.
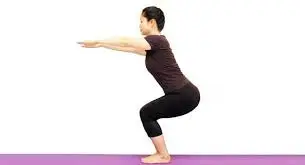
Chair Pose: To begin, stand in tadasana. Inhale as the patient raises both arms above the head, palms facing inward. As the patient inhales, slightly bend each knee and try to bring the thighs parallel to the floor. The body should form a right angle with the upper thighs. Hold this posture for a duration of 30 to 60 seconds. Breathe out and straighten your knees to exit it. Do three repetitions per session. Do three sessions a day.
Seated Leg and Heel Exercise: Start with your feet on the ground. Lift both heels off the floor and hold for 30 seconds before placing your heels back on the ground. Then lift your toes off the ground and hold them for 30 seconds before placing them back on the ground. Repeat three times during the session. Do three sessions a day.
Toe flexion stretch exercise: First, tell the patient to place their heels on the ground with their toes pointing up in the air in front of the patient. Bend your toes down and hold for 30 seconds, then relax. Then curl your toes and hold for 30 seconds before relaxing. Repeat three times during the session. Do three exercises per set in one day.
Toe Raise, Point, and Curl: The toe raise, point, and curl exercise has three steps and helps strengthen all parts of the foot, including the toes. How to do this exercise: The patient should sit in a straight chair with his feet on the floor. Then lift your heels keeping your toes on the ground. Stop when there are only footballs on the floor. Hold this position for ten seconds before lowering your heels.
Next, lift your heels and point your toes so that only the tips of your big toe and second toe touch the ground. Hold for ten seconds before lowering your heel. As a final step, lift your heels and turn your toes so that only the tips of your toes touch the ground. Hold this position for ten seconds. Increase flexibility and range of motion by repeating each step ten times per session for one day.
Big toe stretch: Keeping the big toe with a wide range of motion is important. The big toe stretch also has three steps and aims to stretch and relieve toe pain from wearing tight shoes. How to do this exercise: Ask the patient to sit in a straight chair with his feet on the floor. Bring the left (stomach) leg to the right thigh. Gently stretch the big toes up, down, and sideways with your fingers. Hold the big toe in each position for 30 seconds. Repeat this exercise three times in one session before switching to the other leg. Do three sessions a day.
Toe stretching: First, toe stretching can improve toe muscle control. The patient can do this with both legs at the same time or even with other legs, it all depends on which one is more comfortable for the patient. To perform this exercise: The therapist must instruct the patient to sit in a chair with a straight back, feet lightly resting on the ground.
Without straining, spread your toes as widely apart as you can. Hold this position for thirty seconds. Repeat this exercise or movement three times during the session. Do three sessions a day. When a person has gathered their strength, they can try rubber around their toes. This provides resistance and makes the exercise more difficult later.

Golf Ball Swing Stretch: Rolling a golf ball under the foot can help a patient relieve arch discomfort and relieve pain associated with plantar fasciitis. How to do this exercise: Ask the patient to sit in a straight chair with his feet on the floor. After that, place a golf ball or other small or even hardball on the ground next to your feet.
Place one foot on the ball and move it, pressing as hard as it feels. The ball should massage the lower part of the affected leg. Continue for 30 seconds, then repeat the stretch with the other leg. A frozen water bottle can be a soothing option if you don’t have proper balls on hand. Throughout the session, perform this exercise three times. Work out three times a day.
Ankle stretching exercise: Place the other end of the sports tape on the right foot near the foot (not the toe of the shoe). Extend the right leg and pull the Sports Cord up until the patient has the desired resistance and weight. Extend the right toe down as if the patient were pressing the gas pedal in a car. Repeat ten times, holding for ten seconds each time. Repeat with the left leg after you’ve switched.
Exercise for stretching the finger flexors: First, instruct the patient to lie down on the bed in a relaxed position, such as supine. following, the patient is instructed to inhale deeply and exhale. Following this, the physiotherapist performs passive finger extension movement, which involves moving the foot’s finger toward the face side and maintaining that position for the following thirty seconds. Do it three times per session. Do two sessions per day
Exercise for stretching the finger extensors: First, instruct the patient to lie down in a comfortable position. After that, the examiner tells the patient to take a deep breath and release it, after which the physiotherapist passively performs a finger flexion movement, i.e. the examiner removes the toes from the face and holds it at the endpoint for 30 seconds. Do this 3 times during the session. Do three sessions a day.
Choice of shop
Range of Ankle Circuit Exercises: Ankle circuits can help with range of motion. The patient can perform ankle exercises both from a sitting and lying position: first, slowly rotate the ankle in circles to the left, then to the right. It may be even easier for the patient to try to draw the alphabet in the air with his foot. Lead with the big toe. Keep the movements small and focus on using only the foot and ankle, not the whole leg. In circles, try to do twenty in each direction with each leg. If the patient is doing the alphabet, do 2 sets of this exercise on both legs. During each session, increase the number of repetitions after 5-6 days.
Toe Stretch: This exercise is useful to prevent or even treat plantar fasciitis. This is a condition that causes heel pain when walking and difficulty lifting the toes. How to do this exercise: Ask the patient to sit straight in a chair with his feet on the floor.
After that, place the injured leg on top of the uninjured thigh. Then pull your toes up towards your ankle. There should be a stretch with the bottom of the foot and the heel. Hold for thirty seconds. Massaging the arch of your foot while stretching helps relieve tension and pain. Repeat the toe extension three times on each leg. Do three repetitions per session. Do three sessions a day.
Toe flexion: How to do this exercise – First, the patient is asked to sit straight in a chair with his feet on the floor. Put your left foot on your right thigh after that. Then move your toes down to your ankle. Then hold for 30 seconds after release. Do three repetitions per session. Do three sessions a day.
Ankle dorsiflexion exercise: Begin by asking the patient to assume a relaxed position, such as lying on the bed. The therapist should then instruct the patient to bend the leg as far as the patient can face the tools up. You should not be stuck at the endpoint. Repeat 10 times in one session. Do three sessions a day. As your muscles get stronger, increase the number of repetitions from ten to fifteen and twenty in one session.
Ankle extension (plantar flexion): Begin by asking the patient to assume a relaxed position, such as lying on a bed. After this, the physiotherapist should instruct the patient to move the leg away from the body equipment and down as far as the patient can, but should not hold the endpoint. Repeat ten times during the session in one set. Do 3 sessions a day. As your muscles get stronger, you increase the number of repetitions from 10 to 15 and 20 in one session.
Reverse ankle exercise: First ask the patient to assume a relaxed position, such as lying on the bed. After that, the therapist should instruct the patient to move the foot internally as much as the patient can, but the endpoint should not be caught. Repeat 10 times in one set in one session. Do three sessions in one day. As the muscles get stronger, the number of repetitions improves from 10 to 15 and 20 in one exercise.
Ankle rotation: Begin by asking the patient to assume a relaxed position, such as lying on a bed. After this, the physical therapist should instruct the patient to extend the leg as far as the patient can, but the endpoint should not be taken. Repeat ten times during the session in one set. Do 3 exercises in one day. As your muscles get stronger, increase the number of repetitions from ten to fifteen and twenty in one session.
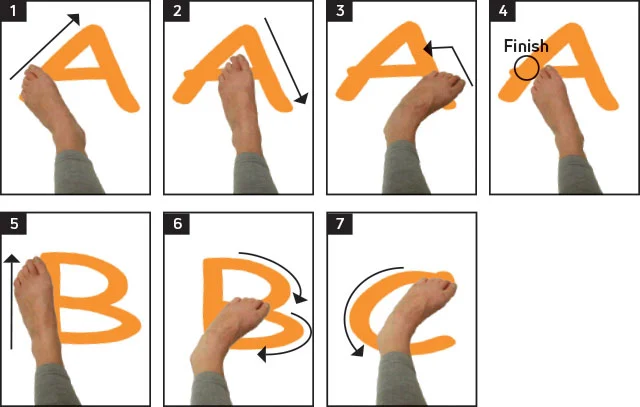
Alphabet: First, draw the letters of the alphabet in the air, describing them with your foot. Use both lowercase and uppercase and make sure you move from the ankle, not the hip. Do ten times during the session, but do not hold the endpoint. Do three sessions a day.
Scope of finger flexion exercises: First, ask the patient to assume a relaxed position, such as lying on the bed. After this, the therapist must instruct the patient to move the fingers down, but the therapist makes sure that the patient does not hold this position at the endpoint and then releases it. Do this ten times during the session. Do three sessions a day. If the patient can do this exercise, the number of repetitions increases from 10 to 15 to 20.
Finger extension exercise: Begin by asking the patient to assume a relaxed position, such as lying down. After this, the physiotherapist must teach the patient to raise the fingers, but the physiotherapist will ensure that the patient does not hold this position at the endpoint and then release it. Do 10 times per session. Do 3 sessions a day. If the patient can do this exercise, increase the number of repetitions from ten to twenty to thirty.
Strengthening exercise
Towel exercise: first place the towel on the ground in front of the chair. After that, tell the patient that with the heel on the floor, try to lift the towel by grabbing it with the toes. Repeat this exercise ten times during the session. Do three sessions a day. This exercise can be made more difficult by adding a small weight to the towel. If the patient can lift the towel ten times, increase the number of repetitions by 10-15-20.
Lifting and holding the big toe: First, the therapist should instruct the patient to place the feet on the ground, lift only the big toe, and keep the rest of the toes on the ground. After 30 seconds of holding this, release the tension. Repeat this exercise three times during the session. Do three sessions a day.

Toe curls: Do toe curls to develop the flexor muscles in the toes and legs, which improves overall strength. How to do this exercise – The therapist should tell the patient to sit straight in a chair with his feet on the floor. Place a small towel on the ground in front of your body, short side towards your feet. Place the toes of the affected leg on the short side of the towel. Try to grab the towel between your toes and pull it toward you. Repeat this exercise ten times before switching to the other leg. To make the exercise more difficult, try pressing the opposite end of the towel with a heavy cuff.
Marble crunch: Marble crunch can increase leg and toe muscle strength. How to do this exercise – Start by asking the patient to sit up straight in a chair with their feet on the floor. Place an empty bowl and about 10-20 marble bowls on the floor in front of the patient’s feet. Using only the toes of the affected leg, instruct the patient to pick up each marble and place it in an empty bowl. Repeat this exercise with the other leg. Do this exercise ten times during the session. Do three sessions a day. As the patient feels comfortable and finds this exercise easier, increase the number of repetitions from 10 to 20.
Heel Raises: First, this exercise can be done both at home and in the clinic, the patient must stand near a wall or a chair against which the patient can balance. Slowly raise the left leg back until the leg is at a 90-degree angle. Return to the starting position shortly after staying for ten seconds. Repeat five times on each leg.

Ankle Circles: Raise your leg about 20 inches off the ground. After that, with the toe up, turn the foot to the left and then back to the right. Revert to the starting position after waiting for ten seconds. Repeat ten times with each leg in one session. Do three sessions a day.
Calf Strengthening Exercise: This is a simple exercise where patients only need to stand on their toes for ten seconds with both feet firmly in place before slowly lowering to the ground. Repeat this ten times or more if necessary.
Leg dorsiflexion: To perform this movement, lie on your back with your hands behind your head. Slowly bend only the knees (keeping them straight) until the knees are over the knees, keeping both feet on the floor. Slowly extend your knees back to the starting position and repeat this exercise 10 times or more if necessary.
Toes pick up: This exercise can help strengthen your toes and improve flexibility. The movement of the toes is controlled by a complex group of muscles (mainly the flexor and extensor muscles of the finger), which are easily weakened by an injury to the foot or ankle joint.
To get started: Place a pile of 20 small objects (such as jacks, hard candies, or even small rocks) on the ground. To move them to a different pile, utilize your toes to pick them up. Do 3 exercises for 3 sets twice a day.
Toes raises: This exercise can help strengthen both the toes and calf muscles. How to do this exercise – Ask the patient to hold onto a wall or counter for balance. After that, stand on the toes as far as the patient can go without pain. Hold the position for the next 10 seconds, maintaining the tension, then release. In the initial phase, do three sets of ten exercises, and always do three sets of thirty exercises. As the patient gets stronger, he may begin to do single-legged toe-ups, which puts more weight on the affected leg.
Ice Bottle Massage Exercise: This is the best exercise for cooling down (literally). The patient should prepare by filling a plastic bottle with water and freezing it overnight. Supplement to the exercise routine: Ask the patient to place a frozen water bottle on the ground. After that, roll the leg over it three times a day for 1-2 minutes. Always move your foot, but don’t stop and let the bottle rest in one place. If the cold causes discomfort, the patient can place a kitchen towel between the bottle and the leg. If you feel pain or even tingling, stop this exercise and avoid it.
Sitting leg and heel: The patient’s feet are flat on the ground so they can move. Lift both heels off the ground and hold for ten seconds before returning to the floor. Then lift your toes off the ground and hold for ten seconds before returning to the ground. Repeat ten times.
Strengthening ankle flexors with a band: First, the patient is asked to sit in a chair and tie a band around a stable surface that does not move, such as a heavy table. Extend your leg and wrap the other end of the strap around the top of your leg. Bend your leg so that the band resists the movement. Hold for 10 seconds. Repeat ten times during the session. Do three exercises a day to strengthen. After 5-6 days, increase the weight from 500 grams to 1 kilogram and also increase the number of repetitions.

Ankle extensors are strengthened with a bandage: first, ask the patient to sit in a chair. After that, take the other half of the tape with both hands, wrap it around the ball of the injured leg, and stretch the leg in front of you. Then take your leg away from your face. Hold this position for the next 10 seconds. Repeat 10 times in one session. Do three sessions a day.
Ankle inverters strengthen with a strap: first, tie the strap around the leg of the chair or maybe on the same side as the table with the injured leg. Then wrap the other end of the tape around the inside of the affected leg. After that, try to turn the leg inwards. For the subsequent ten seconds, sustain this stance. Perform this physical activity ten times in a single session. Do three sessions a day. When the patient has adapted to the weight of 500 grams, increase the weight to 1 kilogram and increase the number of repetitions.
Ankle-hand strengthening exercise with tape: first tie the tape to the leg of the chair opposite the injured leg. After that, wrap the other end around the outside of the affected leg. Then the therapist must teach the patient to try to turn the leg and hold for ten seconds, repeating this exercise 10 times in one session. Do three exercises and three sets per day. When the patient has adapted to the weight of 500 grams, increase the weight to 1 kilogram and increase the number of repetitions.

Steps: Start with the injured leg at the bottom of the step and the good leg on the floor. Extend the knee so he can lift himself onto the affected leg, then lower it. Repeat this exercise ten times in one session, at least 3 exercises and three sets per day. If the patient is satisfied with low repetitions, increase the number of repetitions.
Walking on the sand: Walking barefoot on the sand is a great way to stretch and strengthen your legs and calves. It’s generally good exercise because the soft texture of the sand makes walking more physically demanding. Do this exercise – Go to the beach, the desert, a volleyball court, or some other place with sand. Remove shoes and socks. At first, make three laps on the sand, after 5-6 days increase the laps to six.
How can I prevent ankle pain?
It may not always be possible to prevent ankle pain. But by maintaining good health, you can keep your bones, ligaments, and tendons strong. To prevent ankle pain caused by an injury, you should:
- Maintain a healthy weight: Carrying extra weight puts strain on the joints, including the ankle.
- Strengthen another muscle: You can stabilize your ankles and lower your chance of injury by improving the strength of other muscles.
- Stop if you feel pain: Don’t ignore pain. If movement or activity feels uncomfortable, take a break. Contact your provider if the pain does not improve. Exercise through pain might exacerbate existing injuries.
- Warm up properly: stretch before exercise. Muscles and soft tissues (such as ligaments and tendons) are less damaged in the heat.
You can prevent ankle disease by maintaining good physical fitness, strength, and flexibility. Regular exercise is important to maintain bone strength and balance. Other behaviors that can prevent ankle sprains include:
- Warming up and stretching either before or following exercise
- Wear comfortable shoes that support the ankle
- Pay attention to your body’s warning signs and don’t push yourself too hard
Most ankle injuries can be avoided by taking precautions before strenuous exercise. Please get in touch with your doctor instantly if you suspect an injury or suffer from unusual ankle discomfort when exercising.
When should I call my doctor for ankle pain?
While most ankle sprains heal with a little TLC and home care, it’s important to know when the injury has progressed beyond that point. Those with extreme swelling or bruising and an inability to apply pressure or pressure to the area without significant pain should seek medical attention. Another general rule is to see a doctor if there is no improvement in the first few days.
Call your doctor if:
- Ankle pain is severe or does not go away after two to three days of home treatment.
- Pain and swelling occur suddenly.
- You experience a temperature or the affected area is red or warm to the touch, which are potential indicators of an infection.
- You cannot squeeze the ankle.
Numerous ailments and injuries can cause ankle pain. Walking can prove impossible due to discomfort, stiffness, and swelling. Most ankle injuries improve with home remedies such as elevating the leg and getting enough rest. A sprained ankle usually does not require surgery. If the pain is severe, you have a lot of swelling, or the pain doesn’t go away after a few days, contact your provider. Many non-invasive procedures are available to help you in getting back on your feet.
Home Remedies for Ankle Pain While Walking
- Rest: First try to avoid pressure on the affected foot or ankle. Do not exercise at this time, but try to gently move the affected area from time to time so that the area does not become stiff.
- Ice: Place an ice pack or frozen vegetables covered with a wet cloth on the painful area for ten minutes every two to three hours.
- Compression: wrap a crepe bandage around the affected area. It should be tight enough to support the injured area, but not so tight that it restricts blood flow. If the bandage is damaged, place a small piece of cotton between the skin and the bandage and the next toe, then tape them together.
- Elevation: To minimize swelling, elevate the affected limb.
- Supportive footwear: Make sure your shoes provide adequate foot and ankle support. Abstain clear of sandals, flip-flops, and extremely loose shoes. When you play sports, it is especially important to wear appropriate shoes. Activities such as basketball and volleyball can cause ankle injuries, especially without proper footwear.
FAQs
Can ankle pain go away?
The wound can delay healing fully for a few weeks to several months. After the pain and swelling are mostly gone, the injured ankle will still be slightly weaker and less stable than the uninjured ankle. You need to start doing exercises to strengthen your ankle and prevent future injuries.
Can ankle pain be treated?
Most foot or ankle pain can be treated without seeing a doctor. A soft tissue injury should heal within the first few days with some simple self-care tips. You may need to be careful and protect the affected area for several months until it heals completely.
Can bad shoes cause ankle pain?
In many cases, however, ankle pain is simply caused by wearing the wrong shoes. You may develop ankle pain if, Your tight shoes strain your ankle joints and cause inflammation. The shoes are loose, which increases the stress on your shin joint.
References
- Professional, C. C. M. (n.d.). Ankle Pain. Cleveland Clinic. https://my.clevelandclinic.org/health/symptoms/15295-ankle-pain
- Burke, D. (2018, March 16). Ankle Disorders: Causes, Symptoms, and Diagnosis. Healthline. https://www.healthline.com/health/ankle-disorders#prevention
- P. (2020, March 10). Start a PT Treatment Plan and Get Free of Ankle Pain. Marketplace Physical Therapy & Wellness Center. https://marketplacewellnesscenter.com/stomp-out-ankle-pain-by-getting-started-on-a-pt-treatment-plan/
- Prajapati, N. (2022, April 30). Walking-related ankle pain: causes, symptoms, remedies, and exercises. Samarpan Physiotherapy Clinic. https://samarpanphysioclinic.com/ankle-pain-while-walking-treatment/




4 Comments