Antispasticity Drugs
Introduction
Antispasticity drugs are medications used to treat spasticity, which is a condition characterized by muscle stiffness, involuntary muscle contractions, and abnormal muscle tone.
Spasticity is a neurological condition characterized by muscle stiffness, involuntary muscle contractions, and exaggerated reflexes. It is commonly associated with conditions that affect the central nervous system, such as multiple sclerosis, cerebral palsy, spinal cord injury, or stroke.
Spasticity occurs due to an imbalance in the signals between the brain and the muscles, leading to abnormal muscle tone and movement. In a healthy nervous system, muscles receive signals from the brain to contract or relax in a coordinated manner. However, in individuals with spasticity, there is a disruption in this communication. The underlying cause of spasticity varies depending on the specific condition or injury affecting the nervous system.
When the signals from the brain to the muscles are disrupted or damaged, an excessive amount of excitatory signals is transmitted to the muscles. As a result, the affected muscles become hyperactive and resistant to movement. This increased muscle tone can lead to stiffness, tightness, and difficulties with coordination and range of motion. Spasticity can affect different muscle groups and vary in severity from mild to severe. It may manifest as muscle spasms, clonus (repetitive, involuntary muscle contractions), or hypertonia (increased muscle tone). These symptoms can interfere with daily activities, impair mobility, and cause pain or discomfort.
The management of spasticity often involves a multidisciplinary approach, including medication, physical therapy, occupational therapy, and assistive devices. Antispasticity drugs, as discussed earlier, are commonly prescribed to help reduce muscle spasticity and improve functional abilities. These medications work through various mechanisms to relax muscles, inhibit nerve signals, or modulate neurotransmitters involved in muscle control. Individuals with spasticity need to work closely with healthcare professionals to develop a personalized treatment plan that addresses their specific needs and goals. Regular monitoring, adjustments in medication dosages, and a comprehensive rehabilitation program can help individuals effectively manage spasticity and improve their quality of life.
What are Antispastic drugs?
Antispasticity drugs are medications used to reduce muscle spasticity, which is a condition characterized by involuntary muscle contractions or stiffness. The counter-spasticity support forestalls contracture by empowering the augmentation of the wrist and digits. For usage with patients with raised tone in wrist, hand, or fingers. These drugs are commonly prescribed for individuals with conditions such as multiple sclerosis, cerebral palsy, spinal cord injury, or stroke, which can cause spasticity. Here are some examples of Antispasticity drugs:
Baclofen: Baclofen is a commonly prescribed Antispasticity medication that acts as a muscle relaxant. It works by inhibiting the release of certain neurotransmitters in the brain and spinal cord, which helps reduce muscle spasms and stiffness.
- Mechanism of action: Baclofen is a gamma-aminobutyric acid (GABA) agonist. GABA is an inhibitory neurotransmitter in the central nervous system (CNS) that helps regulate muscle tone. Baclofen binds to GABA-B receptors in the brain and spinal cord, leading to an increase in inhibitory signals and a decrease in excitatory signals. This action reduces the hyperexcitability of neurons responsible for muscle spasticity.
- Administration: Baclofen can be taken orally in tablet form or delivered via an intrathecal pump, which delivers the medication directly into the spinal fluid.
- Side effects: Common side effects may include drowsiness, dizziness, muscle weakness, fatigue, and gastrointestinal disturbances.
Tizanidine: Tizanidine is another muscle relaxant that is used to treat spasticity. It acts by blocking certain nerve signals that cause muscles to tighten, resulting in muscle relaxation.
- Mechanism of action: Tizanidine drug is an alpha-2 adrenergic agonist. It acts on alpha-2 receptors in the CNS, inhibiting the release of excitatory neurotransmitters, particularly norepinephrine. By reducing the transmission of these signals, tizanidine helps relax muscles and relieve spasticity.
- Administration: Tizanidine is usually taken orally, typically in tablet form.
- Side effects: Common side effects may include drowsiness, dizziness, dry mouth, weakness, and low blood pressure.
Dantrolene: Dantrolene is a medication that directly affects the muscle cells and inhibits the release of calcium, which is necessary for muscle contraction. By reducing calcium levels in the muscles, dantrolene helps relieve spasticity.
- Mechanism of action: Dantrolene acts directly on the skeletal muscle fibers rather than the CNS. It inhibits the release of calcium from the sarcoplasmic reticulum within muscle cells. By reducing calcium levels, dantrolene interferes with the muscle contraction process and helps alleviate spasticity.
- Administration: Dantrolene is available in oral tablet form.
- Side effects: Side effects may include drowsiness, muscle weakness, fatigue, dizziness, and liver toxicity (rare but potentially serious).
Diazepam: Diazepam belongs to a class of medications called benzodiazepines and is sometimes used to manage spasticity. It acts on the central nervous system to produce muscle relaxation and reduce muscle spasms.
- Mechanism of action: Diazepam is a benzodiazepine that enhances the inhibitory effects of GABA in the CNS. By increasing GABA activity, it produces sedative, anxiolytic, muscle relaxant, and anticonvulsant effects. Diazepam helps reduce spasticity by relaxing muscles and decreasing muscle hyperexcitability.
- Administration: Diazepam is available in oral tablet form or as an injectable solution for intravenous or intramuscular administration.
- side effects: Common side effects may include drowsiness, dizziness, confusion, muscle weakness, and dependence with long-term use.
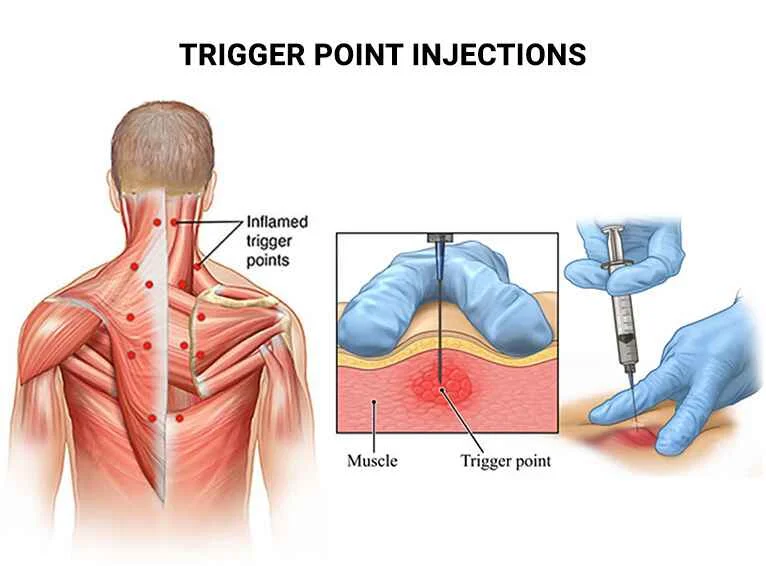
Botulinum toxin injections: While not a drug in the traditional sense, botulinum toxin injections, such as Botox, can be used to treat localized spasticity. This toxin blocks the release of acetylcholine, a neurotransmitter involved in muscle contraction, in specific muscles, leading to muscle relaxation.
- Mechanism of action: Botulinum toxin is produced by the bacterium Clostridium botulinum. When injected into specific muscles, it blocks the release of acetylcholine, a neurotransmitter responsible for muscle contraction. By inhibiting acetylcholine, botulinum toxin weakens the muscle, leading to temporary relaxation and reduced spasticity.
- Administration: Botulinum toxin injections are administered directly into the affected muscles by a healthcare professional.
- Side effects: Common side effects may include injection site pain, bruising, muscle weakness, and flu-like symptoms. Rare but serious complications can arise from the spread of toxins to unintended areas.
Other medications, such as gabapentin, clonazepam, or tizanidine, may also be prescribed depending on the individual’s condition and response to treatment. It’s important to note that the choice of Antispasticity drug depends on the individual’s specific condition, the severity of spasticity, and other factors. These medications should be prescribed and monitored by a healthcare professional familiar with the management of spasticity. It’s essential to note that the appropriate choice of Antispasticity drug depends on various factors, including the individual’s specific condition, the severity of spasticity, medical history, and potential drug interactions. Close monitoring by a healthcare professional is necessary to determine the most effective treatment and manage any side effects.
Pharmacological effect of Antispastic drug
Antispastic drugs are medications used to treat spasticity, which is a condition characterized by increased muscle tone and stiffness. These drugs work by targeting the central nervous system to reduce muscle spasms and promote relaxation. The pharmacological effects of antispastic drugs include:
- Muscle Relaxation: Antispastic drugs act on the muscle tissue and nerves to decrease muscle tone and relieve spasms. They may inhibit the release of neurotransmitters involved in muscle contraction or enhance the action of inhibitory neurotransmitters that promote muscle relaxation.
- Increased Inhibition: Antispastic drugs enhance the inhibitory pathways in the central nervous system, primarily involving gamma-aminobutyric acid (GABA), which is an inhibitory neurotransmitter. By increasing the activity of GABA or facilitating its binding to receptors, these drugs suppress excessive neuronal firing and reduce the excitability of motor neurons, leading to muscle relaxation.
- Reduction of Reflex Activity: Spasticity often involves exaggerated reflex responses, such as deep tendon reflexes. Antispastic drugs can modulate these reflexes by dampening the excitability of the reflex arc. They may inhibit the transmission of signals along the reflex pathway or reduce the responsiveness of motor neurons to sensory input, thereby decreasing the exaggerated reflex activity.
- Improved Range of Motion: By reducing muscle tone and stiffness, antispastic drugs can improve joint mobility and increase the range of motion. This effect allows for greater flexibility and ease of movement.
- Pain Relief: Spasticity can often be associated with pain due to increased tension and abnormal muscle contractions. Antispastic drugs can help alleviate pain by reducing muscle spasms and restoring a more normal muscle tone.
It’s important to note that different antispastic drugs may have varying mechanisms of action and pharmacological effects. Examples of commonly used antispastic drugs include baclofen, tizanidine, dantrolene, and diazepam. These drugs may be administered orally, intramuscularly, or via intrathecal infusion (directly into the spinal canal) depending on the severity of spasticity and individual patient needs. The choice of antispastic drug and dosage is typically determined by a healthcare professional based on the specific clinical situation.
Why do we use anti-spasticity drugs?
Antispasticity drugs are used to manage and alleviate the symptoms of muscle spasticity. Here are the primary reasons why these medications are prescribed:
- Reduce muscle spasms: Antispasticity drugs help reduce or prevent involuntary muscle spasms and contractions. These spasms can be painful, disruptive to daily activities, and affect mobility. By decreasing the frequency and intensity of muscle spasms, Antispasticity drugs can improve comfort and functionality. Muscle spasms are involuntary and often painful muscle contractions that can occur in individuals with spasticity. Antispasticity drugs help reduce the frequency and intensity of these spasms by modulating the neural signals that control muscle activity. By targeting the receptors or neurotransmitters involved in muscle contraction, these medications help restore a more balanced and controlled muscle function.
- Relieve muscle stiffness: Spasticity often causes increased muscle tone and stiffness, making it difficult to move and perform activities of daily living. Antispasticity medications work to relax the muscles, reduce hypertonicity, and alleviate the associated stiffness. This can enhance mobility, range of motion, and overall physical function. Spasticity is characterized by increased muscle tone, leading to stiffness and resistance to movement. Antispasticity drugs work to relax the muscles and reduce hypertonicity. They act on various pathways in the central nervous system to inhibit the release of excitatory neurotransmitters or enhance the inhibitory signals, resulting in a reduction in muscle tone. This relaxation allows for an improved range of motion and ease of movement.
- Improve functional abilities: By reducing spasticity and muscle tightness, Antispasticity drugs can enhance functional abilities and quality of life. They can help individuals with spasticity regain or maintain independence in activities such as walking, dressing, and self-care. Spasticity can significantly impact functional abilities and impair daily activities. Antispasticity drugs aim to enhance functional abilities by alleviating the symptoms of spasticity. By reducing muscle spasms, stiffness, and hypertonicity, these medications help individuals regain or maintain independence in tasks such as walking, dressing, and performing self-care activities.
- Increase range of motion: Spasticity can limit joint movement and flexibility due to the increased resistance and stiffness in the affected muscles. Antispasticity drugs can help improve joint range of motion by reducing muscle tone and allowing for easier and more fluid movement. Spasticity often limits joint mobility and flexibility due to increased muscle tone and resistance. Antispasticity drugs work to decrease muscle tone and allow for a greater range of motion in the joints. This improvement in mobility can lead to better overall movement, coordination, and posture.
- Facilitate physical therapy: Antispasticity medications are often used in conjunction with physical therapy and rehabilitation programs. By reducing muscle spasticity, these drugs can help facilitate the effectiveness of therapy sessions, enabling individuals to actively participate in exercises and therapeutic interventions. Antispasticity drugs are frequently used in conjunction with physical therapy and rehabilitation programs. They help facilitate the effectiveness of therapy by reducing spasticity and muscle tightness, enabling individuals to actively participate in exercises and interventions. This combination approach can lead to improved motor control, strength, and functional outcomes.
It’s important to note that Antispasticity drugs are not a cure for the underlying conditions causing spasticity, but rather help manage the symptoms associated with it. The choice and use of these medications depend on the individual’s specific condition, the severity of spasticity, and their response to treatment. Healthcare professionals with expertise in spasticity management can determine the most appropriate medication and dosage for each individual. The specific Antispasticity drug prescribed and the dosage depend on factors such as the underlying condition, severity of spasticity, and individual response. Regular monitoring and adjustment of medication are often necessary to achieve the optimal balance between symptom relief and minimizing side effects. Healthcare professionals experienced in spasticity management can provide personalized guidance and supervision throughout the treatment process.
Who can take Antispasticity drugs?
Antispasmodic drugs are medications that help alleviate or prevent muscle spasms or cramps. They work by relaxing smooth muscles, which are found in various organs and tissues throughout the body, including the gastrointestinal tract, urinary tract, and blood vessels. Certainly! Here are more details regarding the conditions for which Antispasticity drugs are commonly prescribed:
- Multiple Sclerosis (MS): MS is an autoimmune disease where the immune system mistakenly attacks the protective covering of nerve fibers in the central nervous system. This leads to disruptions in the transmission of nerve signals, resulting in various neurological symptoms, including muscle spasticity. Antispasticity drugs may be prescribed to individuals with MS to help alleviate spasticity and improve mobility.
- Cerebral Palsy (CP): Cerebral palsy is a group of disorders that affect movement, muscle tone, and motor skills. It is caused by damage to the developing brain, typically before birth or during early childhood. Spasticity is a common feature of cerebral palsy, leading to difficulties with muscle control and coordination. Antispasticity drugs can be used to manage spasticity and improve functional abilities in individuals with cerebral palsy.
- Spinal Cord Injury (SCI): Spinal cord injury occurs when the spinal cord is damaged, resulting in varying degrees of paralysis and sensory impairment. Spasticity is a common complication that can develop following a spinal cord injury. Antispasticity drugs may be prescribed to individuals with spinal cord injuries to help reduce muscle spasms, improve mobility, and enhance daily functioning.
- Stroke: A stroke occurs when blood flow to a part of the brain is disrupted, leading to damage in the affected area. Spasticity can develop as a result of stroke, causing muscle stiffness and involuntary contractions. Antispasticity drugs may be used as part of the treatment plan for stroke survivors to manage spasticity and improve motor function.
- Traumatic Brain Injury (TBI): Traumatic brain injury is caused by a sudden impact or trauma to the head, leading to brain damage. Depending on the location and severity of the injury, spasticity may occur as a consequence of TBI. Antispasticity drugs can be considered in the management of spasticity in individuals with traumatic brain injuries.
- Individuals with gastrointestinal disorders: Antispasmodic drugs are commonly prescribed to people with gastrointestinal conditions such as irritable bowel syndrome (IBS), functional dyspepsia, or inflammatory bowel disease (IBD). These medications can help relieve abdominal pain, cramping, and spasms associated with these conditions.
- Patients with urinary tract disorders: Antispasmodics may be used to manage urinary tract disorders like overactive bladder (OAB) or bladder spasms. These medications can help reduce the frequency and urgency of urination and relieve bladder spasms, which can cause discomfort or involuntary urine leakage.
- People with menstrual cramps: Antispasmodic drugs can be used to relieve menstrual cramps (dysmenorrhea). They help relax the smooth muscles in the uterus, reducing the intensity and duration of the cramps.
- Individuals with certain respiratory conditions: Antispasmodic drugs may be prescribed to individuals with conditions that involve bronchial spasms, such as asthma or chronic obstructive pulmonary disease (COPD). These medications help relax the smooth muscles of the airways, allowing for easier breathing.
- Patients with vascular disorders: In some cases, antispasmodic drugs may be used to manage conditions that involve spasms in blood vessels, such as Raynaud’s disease or peripheral vascular disease. These medications help dilate the blood vessels, improving blood flow and reducing symptoms like cold fingers or toes.
It’s important to note that the use of Antispasticity drugs should be determined on an individual basis. The specific condition, severity of spasticity, response to treatment, and overall health of the person are taken into consideration when prescribing these medications. A healthcare professional with expertise in managing spasticity, such as a neurologist or physiatrist, should evaluate and prescribe the appropriate antispasticity drug for each individual.
Contraindication of Antispastic drugs
While antispasmodic drugs are generally safe and well-tolerated, there are certain situations where their use may be contraindicated. Contraindications are specific circumstances or conditions in which a particular medication should not be used due to potential risks or complications. Here are some contraindications associated with antispasmodic drugs:
- Hypersensitivity or allergy: If a person has a known hypersensitivity or allergic reaction to a specific antispasmodic medication or its ingredients, its use is contraindicated. Allergic reactions can range from mild symptoms like rash or itching to severe reactions like difficulty breathing or anaphylaxis.
- Glaucoma: Antispasmodic drugs can cause an increase in intraocular pressure, which can be problematic for individuals with certain types of glaucoma. These medications can potentially worsen the condition and may be contraindicated for individuals with narrow-angle or closed-angle glaucoma.
- Urinary retention: Antispasmodics that affect the smooth muscles of the urinary tract can worsen urinary retention, a condition where a person has difficulty emptying their bladder. If someone already has urinary retention or bladder outlet obstruction, the use of antispasmodic drugs may be contraindicated.
- Bowel obstruction: Antispasmodic drugs that act on the gastrointestinal tract can slow down bowel movements. If someone has a known or suspected bowel obstruction, the use of these medications may be contraindicated as they can potentially exacerbate the obstruction.
- Myasthenia gravis: Myasthenia gravis is a neuromuscular disorder characterized by muscle weakness and fatigue. Antispasmodic drugs that have anticholinergic effects can further weaken the muscles and worsen the symptoms of myasthenia gravis. Therefore, caution is required, and their use may be contraindicated in individuals with this condition.
It’s important to note that contraindications can vary depending on the specific antispasmodic drug being used. Always consult with a healthcare professional, such as a doctor or pharmacist, to determine the suitability and safety of a particular medication based on your circumstances and medical history.
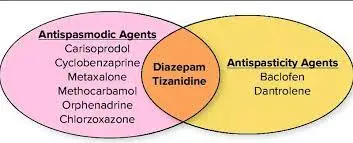
Classifications of Antispasticity drugs
Antispasticity drugs can be classified into different categories based on their mechanisms of action. Here are the classifications and a detailed explanation of each:
GABAergic Agents:
- Baclofen: Baclofen is a GABA-B receptor agonist. It enhances the inhibitory effects of gamma-aminobutyric acid (GABA), which is an inhibitory neurotransmitter in the central nervous system (CNS). Baclofen reduces spasticity by binding to GABA-B receptors and inhibiting the release of excitatory neurotransmitters, leading to muscle relaxation.
Alpha-2 Adrenergic Agonists:
- Tizanidine: Tizanidine acts as an alpha-2 adrenergic agonist, which means it stimulates alpha-2 receptors in the CNS. By activating these receptors, tizanidine inhibits the release of excitatory neurotransmitters, particularly norepinephrine. This reduction in excitatory signals helps relax muscles, reduce spasticity, and improve muscle tone.
Direct Acting Muscle Relaxants:
- Dantrolene: Dantrolene is a direct-acting muscle relaxant that works by interfering with the release of calcium from the sarcoplasmic reticulum within muscle cells. By reducing calcium levels, dantrolene inhibits the muscle contraction process, resulting in relaxation and a decrease in spasticity.
Benzodiazepines:
- Diazepam: Diazepam is a benzodiazepine that enhances the inhibitory effects of GABA in the CNS. By increasing the activity of GABA, diazepam produces sedative, anxiolytic, muscle relaxant, and anticonvulsant effects. It helps reduce spasticity by relaxing muscles and decreasing muscle hyperexcitability.
Botulinum Toxin Injections:
- Botulinum toxin: Botulinum toxin, commonly known by its brand name Botox, is not a traditional drug but is used as a treatment for localized spasticity. It works by blocking the release of acetylcholine, a neurotransmitter responsible for muscle contraction, at the neuromuscular junction. By inhibiting acetylcholine, botulinum toxin weakens the muscle, leading to temporary relaxation and reduced spasticity.
These are some of the main classifications of Antispasticity drugs. It’s important to note that the choice of medication depends on various factors, including the underlying condition, the severity of spasticity, individual response, and potential side effects. Healthcare professionals with expertise in managing spasticity can determine the most appropriate medication and dosage for each individual, considering these factors and closely monitoring the treatment.
Continuing Education Activity About Antispasticity Drugs
This continuing education activity aims to provide healthcare professionals with an in-depth understanding of antispasticity drugs, including their classifications, mechanisms of action, and clinical applications. By expanding their knowledge in this area, healthcare professionals can enhance their ability to effectively manage spasticity and improve patient outcomes.
Learning Objectives:
- Understand the classification of antispasticity drugs based on their mechanisms of action.
- Explore the mechanisms of action of different classes of antispasticity drugs.
- Examine the clinical applications of antispasticity drugs in various neurological conditions.
- Discuss the potential side effects, precautions, and monitoring considerations associated with antispasticity drug therapy.
- Review evidence-based practice guidelines and recommendations for the use of antispasticity drugs.
How long should I use over-the-counter Antispasticity drugs?
However, as a general guideline, over-the-counter medications typically provide short-term relief for acute symptoms. They are not intended for long-term use without medical supervision. If you are experiencing persistent or chronic spasticity, it’s advisable to seek medical attention to determine the underlying cause and appropriate treatment options.
It’s important to follow the recommended dosage instructions provided on the medication packaging or consult with a healthcare professional for guidance. If your symptoms persist or worsen despite using over-the-counter Antispasticity drugs, it’s crucial to seek further medical evaluation to identify the underlying cause and explore alternative treatment options.
Remember, self-medication with over-the-counter drugs should be done cautiously, and it’s always best to seek professional medical advice for your specific situation.
How long do antispastic drugs take to work?
The time it takes for antispasticity drugs to work can vary depending on several factors, including the specific medication, individual response, and the severity of spasticity. Here are some general considerations:
- The onset of Action: Antispasticity drugs may have varying onset times, meaning the time it takes for the medication to start producing noticeable effects. Some medications may have a relatively rapid onset, with effects becoming apparent within hours or days. Others may require a longer time for the therapeutic effects to be noticeable, potentially taking weeks to achieve the desired outcome.
- Individual Response: Different individuals may respond differently to antispasticity drugs. Some people may experience a rapid and significant reduction in spasticity shortly after starting the medication, while others may require a more gradual adjustment period before experiencing noticeable improvements. The response to treatment can be influenced by factors such as the underlying condition, overall health, and individual variations in drug metabolism.
- Titration and Optimization: In many cases, antispasticity drugs need to be titrated or adjusted to find the optimal dosage for an individual. This involves starting with a lower dose and gradually increasing it over time until the desired therapeutic effect is achieved. This titration process allows for careful monitoring of the response to treatment and helps find the lowest effective dose while minimizing potential side effects.
- Treatment Duration: Antispasticity drug therapy is often considered a long-term management approach for chronic spasticity. The duration of treatment can vary depending on the underlying condition and the individual’s response to the medication. In some cases, antispasticity drugs may be used continuously to maintain symptom control, while in other situations, treatment may be intermittent or based on specific exacerbations of spasticity.
It’s important to note that the response to antispasticity drugs can be individual and may require ongoing monitoring and adjustments by healthcare professionals. Regular follow-up appointments with your healthcare provider will allow for an assessment of treatment effectiveness and potential modifications to the medication regimen. If you have specific concerns about the timeline for antispasticity drugs to take effect or are experiencing unexpected or prolonged delays in symptom improvement, it is best to consult with a healthcare professional who can evaluate your specific situation and provide personalized guidance.
How are Antispastic drugs prescribed?
Antispastic drugs are typically prescribed by healthcare professionals, such as physicians, neurologists, or rehabilitation specialists, who have expertise in managing spasticity. The prescription process involves a comprehensive evaluation of the individual’s condition, medical history, and specific needs. Here are the general steps involved in prescribing antispastic drugs:
- Medical Evaluation: The healthcare professional will conduct a thorough medical evaluation, which may include a physical examination, a review of medical history, and an assessment of the individual’s symptoms and functional limitations. This evaluation aims to determine the underlying cause of spasticity, identify any co-existing conditions, and assess the severity of spasticity.
- Diagnosis and Treatment Plan: Based on the medical evaluation, a diagnosis will be made, and a treatment plan will be developed. The treatment plan may involve a combination of interventions, including Antispasticity drugs, physical therapy, occupational therapy, assistive devices, and lifestyle modifications.
- Medication Selection: The healthcare professional will consider several factors in selecting the appropriate antispastic drug. These factors include the individual’s underlying condition, the severity of spasticity, medical history, potential drug interactions, and individual response to medications. The choice of medication will be based on the specific mechanisms of action, efficacy, safety profile, and suitability for the individual’s needs.
- Dosage and Titration: Once the medication is selected, the healthcare professional will determine the appropriate dosage and titration schedule. The initial dosage is often started at a low level to minimize side effects and then gradually increased based on the individual’s response and tolerance. The goal is to find the lowest effective dose that provides optimal symptom relief while minimizing potential side effects.
- Patient Education: The healthcare professional will provide detailed instructions to the individual regarding the medication, including dosage, frequency, and any special instructions (e.g., taking with food). They will also discuss potential side effects, precautions, and what to do in case of adverse reactions. Patient education is crucial to ensure proper understanding and adherence to the prescribed medication regimen.
- Monitoring and Follow-up: Regular monitoring and follow-up appointments will be scheduled to assess the individual’s response to the medication. This allows for evaluation of the treatment’s effectiveness, monitoring for side effects, and potential adjustments to the medication regimen if needed. The healthcare professional may also guide lifestyle modifications, physical therapy exercises, or other adjunctive treatments to enhance the overall management of spasticity.
It’s important to note that the prescription process may vary depending on the healthcare system and the specific requirements of the individual’s condition. Collaboration and open communication between the healthcare professional and the individual is essential to optimize treatment outcomes and ensure individual needs are addressed.
What are the common side effects of Antispastic drugs?
Antispastic drugs can have various side effects, and the specific side effects experienced may differ based on the medication and individual factors. It’s important to note that not all individuals will experience side effects, and some side effects may be temporary or resolved with time. Here are some common side effects associated with antispastic drugs:
- Sedation and Drowsiness: Many antispastic drugs, such as baclofen and benzodiazepines, can cause sedation and drowsiness. Individuals may experience increased sleepiness, reduced alertness, or a feeling of being “drugged.” These effects can impair cognitive function and physical coordination.
- Muscle Weakness: Antispastic drugs that act on muscle relaxation, such as dantrolene, may lead to muscle weakness. This can affect strength and coordination, potentially impacting daily activities or tasks that require fine motor skills.
- Fatigue: Fatigue or excessive tiredness is a common side effect of some antispastic drugs. It can contribute to a decreased level of energy, physical stamina, and mental alertness.
- Dry Mouth: Many antispastic drugs, including medications like baclofen and tizanidine, can cause dry mouth. This can lead to discomfort, altered taste perception, difficulty swallowing, and an increased risk of dental problems.
- Gastrointestinal Disturbances: Antispastic drugs may cause gastrointestinal side effects, including nausea, vomiting, constipation, or diarrhea. These effects can vary in severity and may require additional management strategies, such as dietary modifications or the use of stool softeners or laxatives.
- Dizziness and Lightheadedness: Some individuals may experience dizziness or lightheadedness, especially when standing up or changing positions quickly. This can increase the risk of falls or accidents, particularly in older adults.
- Cognitive Impairment: Certain antispastic drugs, particularly those with sedative effects, can cause cognitive impairment, including difficulties with memory, attention, concentration, and decision-making. These effects may be more pronounced in higher doses or when combined with other sedating substances.
- Hypotension: Some antispastic drugs, such as alpha-2 adrenergic agonists, can lower blood pressure, leading to hypotension. This can cause symptoms like dizziness, lightheadedness, or fainting. It’s important to monitor blood pressure regularly during treatment.
- Mood Changes: Antispastic drugs may occasionally affect mood and emotions, leading to symptoms such as irritability, depression, or anxiety. These changes should be reported to a healthcare professional for further evaluation.
- Allergic Reactions: Although rare, allergic reactions to antispastic drugs can occur. Symptoms may include rash, itching, swelling, difficulty breathing, or other signs of an allergic response. Immediate medical attention should be sought if any allergic reactions are suspected.
It’s important to discuss potential side effects with the prescribing healthcare professional and report any adverse effects experienced. They can guide managing side effects, adjusting the medication regimen, or considering alternative treatment options if necessary. Adherence to the prescribed dosage and regular follow-up appointments can help minimize and address any potential side effects effectively.
Can Antispastic drugs cause allergic reactions?
Yes, allergic reactions to antispastic drugs are possible, although they are relatively rare. Allergic reactions occur when the immune system reacts adversely to a medication, perceiving it as a threat. Here are some details about allergic reactions to antispastic drugs:
Symptoms: Allergic reactions can manifest in various ways, and symptoms can range from mild to severe. Common symptoms include:
- Skin reactions: Rash, hives (itchy, raised welts on the skin), itching, or redness.
- Swelling: Swelling of the face, lips, tongue, or throat, which can lead to difficulty breathing or swallowing.
- Symptoms of the airway: Wheezing, shortness of breath, chest tightness, or coughing.
- Symptoms of the digestive system:: Nausea, vomiting, diarrhea, or abdominal pain.
- Anaphylaxis: A severe allergic reaction that can be fatal is anaphylaxis. It involves a rapid onset of symptoms, including swelling of the throat, difficulty breathing, a sudden drop in blood pressure, dizziness, and loss of consciousness. Anaphylaxis requires immediate medical attention.
Risk Factors: While allergic reactions can occur in anyone, some individuals may be at a higher risk. People with a history of allergies, asthma, or previous allergic reactions to medications may have an increased likelihood of experiencing an allergic reaction to antispastic drugs. However, it’s important to note that an allergic reaction can occur in individuals without a previous history of allergies.
Medications Associated with Allergic Reactions: While any medication has the potential to cause an allergic reaction, certain antispastic drugs may have a higher risk. Common antispastic drugs, such as baclofen, tizanidine, and diazepam, have been associated with allergic reactions, although such instances are relatively uncommon.
Seeking Medical Attention: If you suspect you are experiencing an allergic reaction to an antispastic drug, it is crucial to seek immediate medical attention. Allergic reactions can escalate rapidly and may require emergency treatment. Contact your healthcare provider, go to the nearest emergency department, or call emergency services if symptoms are severe.
To minimize the risk of allergic reactions, it’s important to provide a detailed medical history to your healthcare professional, including any known allergies or previous adverse reactions to medications. If you experience any symptoms of an allergic reaction after taking an antispastic drug, stop taking the medication and contact a healthcare professional for evaluation and guidance.
Please note that this information is not exhaustive, and it’s important to consult with a healthcare professional or pharmacist for personalized advice and information regarding allergic reactions to specific antispastic drugs.
Enhancing Healthcare Team Outcomes of antispastic drugs
Enhancing healthcare team outcomes when using antispastic drugs involves collaboration and coordination among various healthcare professionals involved in the care of individuals with spasticity. An interdisciplinary approach ensures comprehensive and effective management of spasticity. Here are some ways to optimize healthcare team outcomes:
- Multidisciplinary Team: Establishing a multidisciplinary team consisting of healthcare professionals from different specialties, such as neurologists, physiatrists, physical therapists, occupational therapists, nurses, and pharmacists, can enhance outcomes. Each team member brings unique expertise and contributes to the comprehensive assessment, treatment, and monitoring of spasticity.
- Communication and Collaboration: Effective communication and collaboration among team members are vital. Regular meetings, case conferences, and shared electronic health records facilitate information exchange, treatment planning, and coordination of care. This ensures that all team members are aligned in their approach and can make informed decisions regarding antispastic drug therapy.
- Comprehensive Assessment: Conducting a comprehensive assessment of the individual’s condition, functional abilities, goals, and preferences is essential. This assessment should involve input from different team members to gather a holistic view of the individual’s needs. By pooling their expertise, the team can develop a tailored treatment plan that includes antispastic drug therapy alongside other interventions.
- Individualized Treatment Plan: Antispastic drug therapy should be part of an individualized treatment plan that considers the specific needs and goals of the individual. The healthcare team should collaborate to determine the most appropriate antispastic drug, dosage, and treatment duration based on factors such as the underlying condition, severity of spasticity, response to previous therapies, and potential side effects.
- Education and Support: Providing education and support to individuals and their caregivers is crucial for optimizing outcomes. The healthcare team should educate individuals about their condition, the purpose and potential benefits of antispastic drug therapy, expected outcomes, potential side effects, and proper medication administration. Clear instructions and educational materials can enhance medication adherence and empower individuals to actively participate in their care.
- Regular Monitoring and Follow-up: Regular monitoring of the individual’s response to antispastic drug therapy is necessary. The healthcare team should establish follow-up appointments to assess treatment effectiveness, adjust dosages if needed, address any concerns or side effects, and evaluate functional outcomes. This ongoing monitoring ensures that the treatment remains tailored to the individual’s changing needs and promotes optimal outcomes.
- Rehabilitation Interventions: Antispastic drug therapy is often complemented by rehabilitation interventions such as physical therapy and occupational therapy. The healthcare team should collaborate to ensure that these interventions are aligned with the medication regimen and that therapy goals are integrated into the overall treatment plan. Regular communication between therapists and prescribing healthcare professionals facilitates coordination and adjustments to the treatment approach as needed.
- Shared Decision-Making: Involving individuals and their caregivers in shared decision-making empowers them to actively participate in their care. The healthcare team should engage individuals in discussions about treatment options, risks, benefits, and expected outcomes. This collaborative approach ensures that the individual’s preferences and goals are considered in the decision-making process.
By promoting collaboration, communication, individualization, and ongoing monitoring, the healthcare team can enhance outcomes associated with antispastic drug therapy. This comprehensive approach addresses the multidimensional aspects of spasticity management and promotes the best possible care for individuals with spasticity.
Precautions to take when using the Antispastic drug
When using antispastic drugs, it is important to take certain precautions to ensure safe and effective treatment. Here are a few available precautions to regard:
- Healthcare Provider Guidance: Antispastic drugs should be prescribed and monitored by a qualified healthcare provider who specializes in the management of spasticity. Follow their instructions carefully regarding dosage, frequency, and duration of treatment. Do not make any changes to your medication regimen without consulting your healthcare provider.
- Allergy and Sensitivity: Inform your healthcare provider about any known allergies or sensitivities to medications. This is important to avoid potential allergic reactions or adverse effects. If you experience any signs of an allergic reaction, such as rash, hives, swelling, or difficulty breathing, seek immediate medical attention.
- Medication Interactions: Inform your healthcare provider about all medications, supplements, and herbal products you are taking, as they can potentially interact with antispastic drugs. Certain drug combinations may lead to increased side effects or reduced effectiveness. Your healthcare provider can help assess potential interactions and adjust your medication regimen accordingly.
- Pregnancy and Breastfeeding: If you are pregnant, planning to become pregnant, or breastfeeding, discuss the use of antispastic drugs with your healthcare provider. Some medications may have risks during pregnancy or while breastfeeding, and alternative treatment options may be considered.
- Driving and Operating Machinery: Some antispastic drugs can cause sedation, drowsiness, dizziness, or other central nervous system effects. It is important to be aware of how the medication affects you before driving, operating heavy machinery, or engaging in activities that require alertness and coordination. Follow your healthcare provider’s guidance regarding these activities.
- Alcohol and Sedatives: Avoid or limit the use of alcohol and other sedatives while taking antispastic drugs. These substances can potentiate the sedative effects of the medication and increase the risk of drowsiness, impaired coordination, and other side effects.
- Monitoring and Reporting: Regularly monitor your response to the antispastic drug therapy and report any unusual or concerning side effects to your healthcare provider. This includes changes in mood, behavior, or any new symptoms that arise during treatment.
- Dosage and Compliance: Take the prescribed dose of the antispastic drug as directed by your healthcare provider. Try not to change the measurements or stop the drug without talking with them. Adhere to the recommended schedule to maintain consistent therapeutic levels of the medication in your body.
- Storage and Disposal: Store antispastic drugs according to the instructions provided on the medication packaging. Keep them out of the distance of pets and children. Dispose of unused or expired medications safely by following local guidelines or consulting with your pharmacist.
It is important to note that these precautions may vary depending on the specific antispastic drug prescribed and individual circumstances. Always consult your healthcare provider for personalized advice and guidance on the precautions to take with your specific medication regimen.
Conclusion
This continuing education activity provides healthcare professionals with a comprehensive understanding of Antispasticity drugs, including their classifications, mechanisms of action, clinical applications, and considerations for their use. By applying this knowledge in practice, healthcare professionals can optimize the management of spasticity and improve the quality of life for patients with neurological conditions.
FAQ
Which muscle relaxant is antispasticity?
Antispasticity specialists — baclofen, tizanidine, dantrolene, and diazepam — help in further developing muscle hypertonicity and compulsory jerks. Antispasmodic specialists, like cyclobenzaprine, are principally used to treat outer muscle conditions.
Is baclofen an antispastic?
Baclofen is a prescription drug that is typically taken orally. It can also be injected into the spine (Gablofen). Baclofen is used to treat muscle spasms caused by brain injury or nerve damage. It is an antispastic muscle relaxant or spasmolytic.
What is the difference between antispasmodic and antispastic?
Antispasmodic medications are used to treat muscle spasms. A muscle spasm is an injury to muscles, tendons, or ligaments and is frequently associated with a sprain or strain of the low back. Antispastics, also known as spasmolytics, are medications used to treat muscle spasticity.
What drug is used for spastic paralysis?
Botulinum Poison (Botox) Infusions: The spastic muscle can be paralyzed with Botox injections, preventing it from contracting. Botox is injected in small amounts into carefully chosen locations based on the pattern of spasticity.
What are Antispasticity agents examples?
Antispasmodic agents (carisoprodol, chlorzoxazone, cyclobenzaprine, metaxalone, methocarbamol, and orphenadrine) and antispasmodic agents (baclofen, dantrolene) are the most common names for these substances.
Can baclofen increase spasticity?
Adverse Effects: It may cause a hypermetabolic state with hyperpyrexia, mental impairment, muscle rigidity, and severe rebound spasticity, which could lead to rhabdomyolysis and system failure involving multiple organs. The side effects enhance recommencing baclofen by a comparable portion as before the interference.