Arthritis of neck
What is Arthritis of the neck?
Neck pain is often caused by many things — but it is most often related to getting older. just like the rest of the body, the disk and joints within the neck (cervical spine) slowly degenerate as we age. Cervical spondylosis also called arthritis of the neck, is the medical term for these age-related, wear-and-tear changes that occur over time in the lower cervical spine.
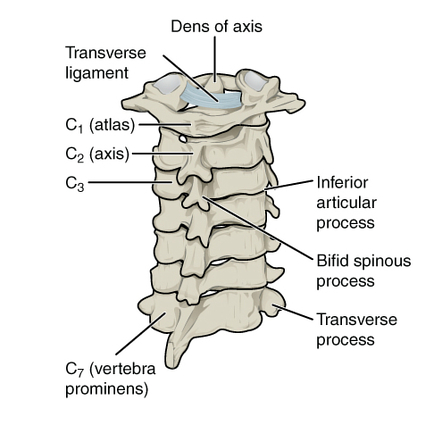
Anatomy of Cervical spine
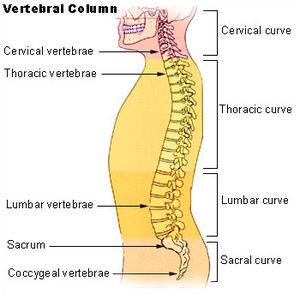
Your spine is formed up of 24 bones, called vertebrae, that are stacked on top of 1 another. These bones hook up to create a canal that protects the spinal cord.
The seven small vertebrae that begin at the bottom of the skull and form the neck comprise the cervical spine.
Intervertebral disks – In between your vertebrae are adjustable intervertebral disks. They act as shock absorbers once you walk or run.
Intervertebral disks are flat and round and a few half-inch thick. they’re made up of two components:
Annulus fibrosus – this is often the tough, flexible outer ring of the disk.
Nucleus pulposus – this is often the soft, jelly-like center of the disk.
Causes of Arthritis of neck
cervical spondylosis occurs naturally as you age thanks to changes in the spinal cord, which may include:
- Herniated discs — cervical spondylosis can occur when bulging discs put pressure on the medulla spinalis and nerve roots.
- Bone spurs — discs degenerate over time, which prompts your body to supply more bone, leading to bone spurs. These bone spurs can put pressure on the cervical spine resulting in cervical spondylosis.
- Stiff ligaments — your neck ligaments get stiffer with age and may cause cervical spondylosis.
- Dehydrated discs — as you age, the cervical discs can dry out, which may cause bone-on-bone contact.
Risk factors
Risk factors for cervical spondylosis include:
- Age — as people age, they’re at a higher risk for developing arthritis in the neck.
- Genetics — there’s evidence that osteoarthritis is hereditary; therefore, some people could also be predisposed to the condition.
- Occupation — careers that involve repetitive neck motions can add extra stress to your neck.
- Neck injuries — if you’ve got had a previous neck injury, you’ll be at a higher risk to develop arthritis in the neck.
- Genetic factors — there’s evidence that arthritis in the neck is hereditary.
- Smoking — smoking can aggravate pain in the neck.
- Weight — overweight people put more weight on the joints and have a tendency to develop neck osteoarthritis sooner.
Neck Arthritis Symptoms
For many, neck arthritis is often a real pain in the neck — others may not experience any symptoms at all.
Some of the most common neck arthritis symptoms involve:
- Neck stiffness
- Pain within the shoulder or arms
- Neck pain
- Headaches that start in your neck
- Trouble sleeping
- Irritability
- Fatigue
- Myelopathy
- Numbness in your arm or hand
- the head or bend of the neck can not do
- Radiculopathy
- Grinding noise or sensation when rotating the neck
When cervical spondylosis leads to myelopathy, other symptoms can occur, like:
- Lack of coordination
- Difficulty walking
- Muscle spasms
- Loss of bowel and bladder control
- Abnormal reflexes
- Tingling, numbness, or weakness within the arms, hands, legs, or feet
- Dealing with symptoms of neck arthritis can be frustrating and, in rigorous cases, debilitating.
What does neck arthritis feel like?
Some people have cervical spondylosis and never even realize it. Others experience clear symptoms, like these four common signs.
- Headaches
Headaches that stem from neck arthritis are literally not headaches at all, but rather pain that you perceive as a headache. We call this a cervicogenic headache, which may be a secondary type of headache, one caused by another condition — during this case, the degeneration of the discs and vertebrae in your neck.
- Popping and grinding noises
Just like many arthritis types, cervical spondylosis makes its presence known whenever you twist, bend, or turn your neck. Some say it seems like they have gravel in their bones. This audible symptom may result from:
- Pressure changes form tiny gas bubbles that enter your joint
- Tendons or ligaments maneuvering around bones
- Bones rubbing against bones
- This symptom is named neck crepitus, and it’s going to be accompanied by some pain and stiffness as well.
- Muscle spasms
Cervical spondylosis is understood to trigger muscle spasms in the neck and shoulders. If you experience this, you’ll attest that it typically comes on suddenly and presents with sharp pain and stiffness. it’s going to even cause your head or neck to jerk to one side or feel stuck in a bent position until it resolves.
- Weakness and numbness
If your neck arthritis causes the space in your cervical spine to constrict, the nerves that pass in and out of that area can easily become compressed. Those nerves travel through your shoulders, down your arms, and into your hands and fingers, so if they become irritated, pinched, or damaged, you’ll feel the repercussions — weakness, numbness, and tingling — all the way right down to your fingertips.
Differential Diagnosis
There are other conditions to think about before making a diagnosis:
- Other non-specific neck pain lesions: postural neck ache, whiplash, acute neck strain
- Fibromyalgia and psychogenic neck pain
- Mechanical lesions: disc prolapse
- Diffuse idiopathic skeletal hyperostosis
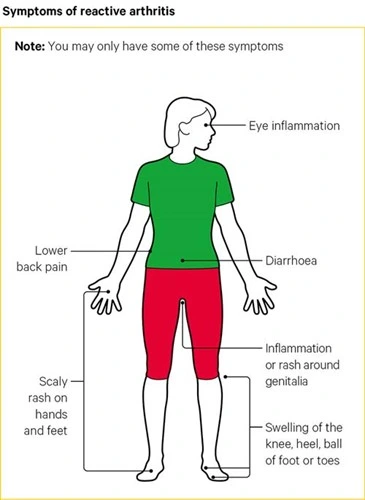
- Inflammatory disease: atrophic arthritis, Marie-Strumpell disease, polymyalgia rheumatic, rheumatoid arthritis, septic arthritis, reactive arthritis
- Metabolic diseases: Paget’s disease, osteoporosis, gout, or pseudo-gout
- Osteomyelitis or tuberculosis
- Malignancy: primary tumors, secondary deposits, or myeloma
Doctor Examination
Physical Examination
After discussing your medical record and general health, your doctor will conduct a radical examination of your neck, shoulders, arms, and, frequently, your legs. they’re going to conduct a number of tests, trying to find problems or changes in the:
- Strength in your arms, hands, and fingers
- Touch sensation
- Reflexes
- Blood flow
- Flexibility in your neck and arms
- Gait (the way you walk)
Your doctor can also gently press on your neck and shoulders — sensing for trigger (tender) points or swollen glands. they’re going to also ask questions to understand further about your symptoms and any injuries that may have occurred to your neck. These questions may include:
- When did the pain start?
- When does the pain occur? Is it continuous? does it come and go?
- Do certain activities make the pain worse?
- Have you ever had pain before?
- Have you ever been treated for pain?
- Do you have any numbness or weakness in your arms or legs?
- Do you have difficulty with fine motor skills, like handwriting or buttoning your shirt?
- Do you have a loss of balance or other coordination problems?
- Were you ever affected by an accident or had an injury to your neck?
Tests
Your doctor may order diagnostic tests to confirm cervical spondylosis diagnosis. These tests may include:
- X-rays – X-rays give images of thick structures, like bone. An X-ray will display the alignment of the bones along your neck. It also can show degenerative changes in your cervical spine — similar to the loss of disk height or the presence of bone spurs.
- Magnetic resonance imaging (MRI) scans – MRI scans create better images of the body’s soft tissues, like muscles, disks, nerves, and spinal cord than X-rays. An MRI can help to decide whether your symptoms are caused by damage to soft tissues, like a bulging or herniated disk.
- Computerized tomography (CT) scans – More detailed than a plain X-ray, a CT scan can help your doctor better view your vertebral canal and any bone spurs.
- Myelogram – during this imaging procedure, contrast dye is injected into the vertebral canal and makes the nerve roots and spinal cord appear more easily. A CT scan is generally done directly following the myelogram while the contrast dye is still in the spinal canal.
- Electromyography (EMG) – Electromyography measures the electrical impulses of the muscles at rest and through contractions. Nerve conduction studies are often done together with EMG to determine if a spinal nerve is functioning properly.
- Other tests – In some cases, your doctor may order a biopsy to determine whether a rheumatoid factor — or any other antibody indicative of inflammatory arthritis — is present.
Treatment of Arthritis of neck
Nonsurgical Treatment
In most cases, Nonsurgical treatment is done for cervical spondylosis patients. Nonsurgical treatment options include:
Medications
- During the primary phase of treatment, your doctor may prescribe several medications to be used together to deal with both pain and inflammation.
- Acetaminophen – Mild pain is usually relieved with acetaminophen.
- Nonsteroidal anti-inflammatory drugs (NSAIDs) – Often prescribed with acetaminophen, NSAIDs like aspirin, ibuprofen, and naproxen are considered first-line medications for neck pain. They relieve both pain and swelling and should be prescribed for a number of weeks, counting on your specific symptoms. Other sorts of pain medication can be considered if you have serious contraindications to NSAIDs or if your pain is not well controlled.
- Oral corticosteroids – a brief course of oral corticosteroids can help relieve pain by reducing inflammation.
- Muscle relaxants – Medications like cyclobenzaprine or carisoprodol can be used to treat painful muscle spasms.
- Steroid-based injections – numerous patients find short-term pain relief from steroid injections.
The most routine procedures for neck pain include:
- Cervical epidural block – during this procedure, steroid and anesthetic medicine are injected into the space next to the covering of the medulla spinalis (epidural space). This procedure is usually used for neck and/or arm pain that may be due to a cervical disk herniation also referred to as radiculopathy or a pinched nerve. Illustration of injection in the cervical spine.
- Cervical facet joint block – during this procedure, steroids and anesthetic medications are injected into the capsule of the facet joint. The facet joints are located within the back of the neck and provide stability and movement. These joints can develop arthritic changes which will contribute to neck pain.
- Medial branch block and radiofrequency ablation – This procedure is employed in some cases of chronic neck pain. It is often used to both diagnose and treat a painful joint. During the diagnosis portion of the procedure, the nerve that supplies the facet joint is blocked with an area anesthetic. If your ache is relieved, then your doctor may have pinpointed the source of your neck pain. the subsequent step option may be to block the pain more permanently. this is often done by damaging the nerves that supply the joint with a burning technique — a procedure called radiofrequency ablation. Pain relief from an ablation generally lasts for several months. however, the nerve regenerates, and, pain can return.
- Although less invasive than surgery, steroid-based injections are prescribed only after an entire evaluation by your doctor. Your doctor will talk with you about the risks and advantages of steroid-based injections for your particular condition.
Surgical Treatment
In cases of neck arthritis where symptoms don’t improve with natural treatments, non-natural, medical intervention, could also be necessary.
Steroid-Based Injections
In some cases, a doctor may prescribe a steroid-based injection, which may be a mix of corticosteroids and a local anesthetic.
These injections are wont to reduce inflammation in the spinal canal and reduce symptoms of neck arthritis.
Surgery
Your doctor may determine that you simply need surgery for your neck arthritis if:
You’ve been diagnosed with cervical radiculopathy — where a nervus spinalis is being pinched by a herniated disk.
You’ve been diagnosed with cervical spondylotic myelopathy — your medulla spinalis is being compressed.
Patients who have neurologic symptoms, like arm weakness, numbness, or falling, are more likely to work out symptoms that improve after having surgery.
Physiotherapy treatment in Arthritis of neck
Conservative and natural care helps numerous neck arthritis sufferers control their pain and slow the progression of the disease. samples of natural treatments are:
- Activity modification — stretching before certain exercises and activities, and participating for shorter periods of your time
- Yoga — relieves neck tension and stress by decreasing tension
- Herbal remedies — turmeric, for instance, is taken into account as an anti-inflammatory and may help reduce neck pain related to arthritis.
- Physical therapy — therapists assist patients to learn exercises that improve posture and strengthen the neck
- Pain relievers — naproxen and ibuprofen can relieve inflammation and alleviate pain
- Warm baths — these can soothe painful joints and relax your muscles
- Ice therapy — ice is understood to reduce inflammation, swelling, and pain
- Massage — this might provide temporary relief
- Chin tuck – these are one of the most effective exercises for combating neck pain. they help strengthen the muscles which pull your head back into alignment over your shoulders.
- Shoulder rolls – are commonly recommended to help strengthen the muscles that support your neck. they’re also great exercises to help keep your shoulders and neck joints fluid.
- Wall push-ups – Normal push-ups can put plenty of strain on your neck muscles — which isn’t ideal when trying to treat neck arthritis. Instead, numerous therapists recommend doing wall push-ups which still strengthen the muscles of the shoulders and assist your neck muscles.
- Soft cervical collar – this is frequently a padded ring that wraps around the neck and is gripped in place with velcro. Your doctor may advise you to wear a soft cervical collar to limit neck motion and permit the muscles in your neck to rest. A soft collar should only be worn for a brief period of time since long-term wear may decrease the strength of the muscles in your neck.
Physical therapy is generally the first nonsurgical treatment that your doctor will recommend. Specific exercises can help relieve pain, and also as strengthen and stretch weakened or strained muscles. In some cases, physiotherapy may include posture therapy or the application of traction to gently stretch the joints and muscles of your neck. physiotherapy programs vary in length but commonly last from 6 to 8 weeks. Typically, sessions are scheduled 2 to three times per week.
FAQ
How long does neck arthritis last?
Among those that do experience neck pain, the discomfort is typically short-lived, improving on its own within six to 12 weeks. Sometimes, cervical arthritis narrows the space where nerve roots exit the spine and pinch the nerve. atrophic arthritis in the neck may not get better; it can worsen if left untreated. whether or not symptoms improve, inflammation, swelling, and stiffness can return with atrophic arthritis in the neck.
What is the most aching arthritis you can have?
Rheumatoid arthritis can be one of the most acheful types of arthritis; it affects joints as well as other surrounding tissues, including organs. This inflammatory, autoimmune disorder attacks healthy cells by mistake, causing painful swelling within the joints, like hands, wrists, and knees. Some may stay about identical for years, but symptoms also can progress and get worse over time. Severe arthritis may affect chronic pain, and difficulty performing routine activities and make walking and climbing stairs painful and grueling. Arthritis also can result in permanent joint changes.
Should I worry if I have arthritis?
Some sorts of arthritis require prompt action. If you’ve got a type of arthritis that can cause permanent joint damage, getting treatment quickly can help preserve joint function and stop other serious health problems. On the opposite hand, infrequent or mild joint pains might not require a special or urgent doctor visit.
How fast does arthritis spread?
Experts confirm that when OA starts, it’s going to take years to reach a severe stage. However, in extreme cases, OA progresses rapidly to finish the destruction of the cartilage within a few months. a number of the factors that determine the rate of OA progression include The severity of your symptoms at the time of diagnosis.
Does arthritis need surgery?
Not everyone with arthritis will need surgery, but it can help to scale back pain and improve mobility. during this section, you’ll search out about the common types of surgery for people with arthritis, how it could facilitate your and what the recovery process involves. If an individual has severe joint damage due to osteoarthritis or inflammatory arthritis, they’ll require arthrodesis or fusion surgery. During this procedure, a surgeon will use hardware, like pins, plates, or rods, to hitch two or more bones.




One Comment