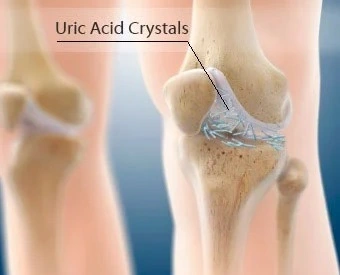
Gout of knee
What is Gout?
Synovial fluid is the component that the body produces to lubricate the joints. In gout, excess acid causes needle-shaped crystals to make in the synovial fluid. the acid may be a normal chemical in the blood that arrives from the breakdown of other chemicals in the body tissues. Some uric acid has situated in everyone’s blood. As your system tries to urge rid of the crystals in the synovial fluid, inflammation develops.
For a person with too much acid, this inflammation can cause painful arthritis, sometimes called gout. Gout was the 1st disease in which researchers recognized that crystals within the synovia could be the cause of joint pain.
Risk Factors For Gout
Some people are more vulnerable to gout than others and there is often little correlation between the levels of uric acid in the blood and knee gout
Symptoms of Gout in the knee
In fact, approximately 50% of individuals with gout do NOT have hyperuricemia or high acid levels.
There is a variety of other factors that increase your risk of developing gout knee pain:
- Genetics: there’s thought to be a genetic link in about 20% of cases
- Age: most ordinarily affects people over 40 with the peak incidence at 75
- Obesity: especially rapid weight gain. A BMI greater than 35 increases the danger three times
- Diet: accounts for about 12% of cases. Risk factors carry excessive alcohol input especially binge drinking, fructose-based beverages, and seafood
- Medical Conditions: renal disorder and/or metabolism problems
- Drug Treatments: most ordinarily diuretics (known as water tablets) used to treat high blood pressure, coronary failure, and edema
- Trauma: gout knee may evolve after damage or surgery
- Gout knee can develop any time after puberty, although, in women, it tends to plan menopause. this is frequently thought to be due to the positive effect of estrogen until then.
Common Gout Knee Symptoms
In most cases, the symptoms of gout within the knee develop rapidly over a few hours.
Common gout knee symptoms include:
- Knee Pain & Swelling: The knee quickly becomes hot, swollen, and red and typically becomes extremely sore
- Night-Time Onset: Gout knee symptoms usually start in the dark due to lower body temperatures
- Skin Changes: the skin around the knee joint often looks shiny and there may be small, firm lumps under the skin, referred to as a trophy
- Fever: Sometimes, gout leads to a raised body temperature
- Reduced Function: Gout knee often makes weight-bearing activities like walking and going up and down stairs incredibly painful
Who gets gout in the knee?
Gout affects about 4 percent trusted Source of adults in the United States. It tends to be more common in men because women usually have lower levels of acid. But after menopause, women start to possess higher uric acid levels. In conclusion, women tend to develop gout at an older age than men.
Experts aren’t sure why some people produce more acid or have trouble processing it. But there’s evidence that the condition is usually genetic.
Other things which will increase your risk of developing gout include:
- consuming plenty of high-purine foods
- consuming foods and drinks, especially alcohol, that increase acid production
- being overweight
- Having high vital signs or heart failure can also put you at a higher risk of developing gout. Diuretics, which are sometimes wont to treat these conditions also can increase your risk.
Diagnosis of Gout of Knee
Gout is often difficult to diagnose because its symptoms are similar to several different conditions. to assist diagnose gout, your healthcare provider may:
Ask you to supply your medical history, including:
- Your symptoms.
- Any other medical problems you have?
- Any medications you’re taking.
- Examine the affected joints.
- Order a laboratory test to test urate levels in your blood.
- Take a sample of fluid from one of your painful joints, a swollen bursa (a fluid-filled sac that cushions the joint), or a tophus to see for urate crystals using a special microscope.
- Order an ultrasound to test for urate crystal buildup in the affected joint as well as to diagnose other conditions that may be causing the symptoms.
How is gout within the knee treated?
There’s no cure for gout, but a mixture of medications and home treatments can help to manage knee pain and reduce the number of flare-ups you have.
Medication
Medications that will help reduce pain from a gout flare-up in your knee involve:
over-the-counter nonsteroidal anti-inflammatory drug drugs (NSAIDs), like ibuprofen (Advil) prescription-strength NSAIDs, like celecoxib (Celebrex) or indomethacin (Indocin) corticosteroids, which can be taken orally or injected into your knee joint to help ease pain and inflammation colchicine (Colcrys), maybe a pain reliever that targets gout pain but can sometimes cause nausea and other side effects Your doctor may additionally prescribe a low daily dose of colchicine to decrease your risk of future flare-ups.
Other drugs which will help to reduce your number of future flare-ups include:
allopurinol (Zyloprim) and febuxostat (Uloric), which limit the body’s acid production and may help to reduce the chances of gout forming in other joints
uricosurics, like lesinurad (Zurampic) and probenecid (Probalan), which help your body eliminate excess acid, though they’ll increase your risk of kidney stones
Home remedies
One of the most effective ways to manage gout is to limit your input of purine-rich foods and beverages. Remember, your body produces acid when it breaks down purine.
That means consuming less:
- red meat
- organ meats, like liver
- seafood, particularly tuna, scallops, sardines, and trout
- alcohol
- sugary drinks
- Cutting out some of these foods may similarly contribute to weight loss. It is an added bonus since carrying extra weight is a risk factor for gout.
Physiotherapy Treatment in Gout of knee
In some cases of gout when the joint flares up, treatment with a physiotherapist at Advantage Physiotherapy is often helpful in conjunction with medication. Your therapist may use modalities like ice, ultrasound, or laser to calm your joint down. you’ll also apply ice or a cold compress at home to soothe a joint flare-up with gout. In many cases, however, direct physiotherapy treatment to the joint is just too painful during a flare-up so resting and elevating the joint is the recommended treatment during this time.
Often when a joint is during a flare-up of gout, walking on the joint are often extremely painful or nearly impossible. Your physiotherapist can advise you on whether you should use a walking aid such as a cane/stick to assist your gait. Walking without the right support or with a limp for even a short period of time due to the pain of gout can cause you to develop incorrect gait patterns and put excess strain on the other joints of your body, particularly those within the lower extremities. Your therapist also will ensure that once your gout flare-up subsides that you are walking well and that you haven’t developed any poor long-term walking habits.
Being that repeated flare-ups of gout can eventually damage the joints and alter the way they move and function, it’s important that you maintain a good range of motion in the joints, also as the flexibility and strength of the muscles surrounding the joints. Your physiotherapist will assess the joints that are commonly suffering from gout in your case and will prescribe a range of motion, stretching, and strengthening exercises to assist maintain the maximum function of the joints. Proprioception exercises, which assist in maintaining the joint’s sense of position, also will be prescribed. All exercises should be done between flare-ups instead of during a flare-up. Exercising a joint inflamed by gout is usually too painful, and should be detrimental to the joint due to the uric acid crystals that can wear on the joint surface during extreme motions of the joint.
As mentioned above, a sedentary lifestyle without exercise, obesity, also as hypertension are all risk factors for developing gout. For this reason, at Advantage Physiotherapy, we feel it’s important for all patients with gout to take part in a cardiovascular exercise program in order to reduce these risk factors, which may assist in decreasing the number of flare-ups of gout that occur. Your therapist can advise you on an appropriate cardiovascular exercise for you to partake in and may devise a program of exercise for you to follow. Some clients will find that doing a cardiovascular exercise within the pool, together with their other stretching and strengthening exercises, is simpler and less painful on their joints. like the other exercises mentioned above, cardiovascular exercises are best done between bouts of gout instead of during a flare-up.
Another risk factor for gout, as mentioned above, is diet. Alcohol, a high carbohydrate diet, or one filled with rich meats or sugary drinks will affect your gout. Your therapist can refer you to a Nutritionist to debate altering your diet in order to help manage your gout. Treatment for gout may be a matter of management rather than elimination of the problem. By working closely together with your doctor, physiotherapist, and other healthcare professionals you’ll successfully manage the disease with as little impact as possible on your everyday life and activities.
- To Pain control
- Electrotherapy including
- Transcutaneous electrical nerve stimulation (TENS)
- Interferential Therapy (IFT)
- Short-wave Diathermy(SWD)
- Electrotherapy including
- Strengthening and range of movement exercises
- Cardiovascular activity
- Hydrotherapy
- Wax therapy
- Cryotherapy (cold therapy)
- Mobilisation techniques
- Home exercise program
Gout Knee Recovery Time
A common question with gout in the knee is how long does it last?
Ultimate cases of gout knee are acute, sudden, and short-lived. Left untreated, most episodes of gout knee calm down after a couple of weeks. Unfortunately, repeat occurrences are common and most people will experience a recurrence of gout knee pain anywhere from 6 months to 2 years later. 60% of gout victims will have a recurrence within 1 year.
Are The Any Possible Complications?
Sometimes, gout spreads from the knee and affects quite one joint at a time, like the big toe or hands. There is also a risk of uric acid causing crystals to form in the kidneys which can lead to inflammation, scarring, and kidney stones.
Gout Prevention
There is multiple things you can do to help with gout prevention. The prevalence of gout has doubled over the last 20 years. this is frequently thought to be due to the increase in life expectancy, dietary changes, and a rise in gout-associated diseases.
The best ways to decrease your risk of gout knee are to:
Avoid Excessive Alcohol Input: alcohol can increase urate levels, specifically beer, stout and fortified wines.
Lose Excessive Weight: obese people are more likely to suffer from gout – discuss weight loss together with your doctor.
Avoid Fructose-Sweetened Drinks: like soda.
Avoid Purine Rich Food: e.g. offal, certain vegetables, oily fish, pulses, e.g. asparagus and spinach.
See your Doctor: Get your doctor to review your regular medications just in case any of them may be predisposing you to gout. for instance, Allopurinol inhibits the formation of urate, probenecid increases its excretion by the kidneys.
Supplements: There are a variety of different supplements on the market that claim to lower uric acid levels and many gout sufferers swear by them.
One study showed that an intake of 1,500mg per day of vitamin C decreases the risk of gout by 45%. Always ask your doctor before starting any gout supplements.
Drink a lot of Water: to prevent dehydration. Aim for about 1.2 liters daily.
Living With Gout
There are numerous things you can do to help manage gout. you’ll make some life changes to help you have fewer gout flares and manage your symptoms, similar as:
Losing weight: If you’re overweight or obese, losing weight through a reduced-calorie diet and increased exercise helps reduce urate levels, which may help stop or lower the number of flares you have.
Making diet changes to assist reduce blood urate levels and gout flares, such as:
- Drinking fewer alcoholic beverages. This includes nonalcoholic beer.
- Avoiding drinks that have high-fructose syrup, like soda.
- Avoiding red meats and organ meats (liver, kidney, tongue, and sweetbreads) that are higher in purines and should increase the risk for other health conditions.
- Avoiding seafood, like shellfish (shrimp and lobster), sardines, and anchovies.
Following the Dietary Approaches to prevent Hypertension (DASH) eating plan. This diet is especially helpful for many gout patients who also have high blood pressure. The DASH eating plan can help improve high vital signs and may help lower blood urate levels. Lowering urate levels, this plan may help to prevent gout flares.
The DASH eating plan includes :
- Eating many vegetables, fruits, and whole grains.
- Consuming low-fat or fat-free dairy products, poultry, and oils.
- Limiting foods high in saturated fats.
- Limiting sugar-sweetened foods and drinks.
When you have a gout flare, you’ll do the following to help reduce symptoms from the flare:
- Applying ice to the affected area to assist reduce swelling and pain.
- Elevating the affected limb, if possible, to assist reduce swelling.
- Resting the affected joint.
When gout is related to frequent flares or tophi, lifestyle changes alone aren’t sufficient to manage gout, and medications to lower urate levels in your blood are the mainstay for managing gout. Taking the medications prescribed for this purpose by your doctor regularly is the key to preventing gout flares from being and preventing or reducing tophi. Nevertheless, maintaining a healthy weight and diet also is important to help lower the risk of cardiovascular complications, which are common among gout patients.
Regularly talk together with your doctor before making any changes to your diet or medications.
FAQ
Is gout a permanent disease?
One of the most common inflammatory arthritis is Gout. The disease is thanks to the deposition of monosodium urate crystals. These deposits are reversible with proper treatment, suggesting that gout may be a curable disease. Gout may be a treatable condition, and therefore the uric acid level can be decreased by medication and lifestyle changes. ask your healthcare provider about medications that can reduce uric acid levels. they will also discuss changes you can make to your diet and lifestyle to prevent and reduce gout attacks
Does gout increase BP?
It is generally understood that in gout high pressure is the rule with increasing hypertension during the acute attacks (pain), and within the later stages hypotension develops associated with cachexia, acidosis, and cardiac weakness. Eventually, severe pain — including that caused by gout — can raise blood pressure. which can be the only reason your blood pressure result was higher than usual. Effective treatment of gout should relieve the pain and pain relief could lower your sign
Is it good to walk with gout?
It is secure for people to walk with gout. In fact, doing joint-friendly activities like walking can help improve gout-related pain. Gout could also be a form of arthritis. It generally affects the big toe joint, but it can also affect the ankles, lesser toes, and knees. It affects one joint at a time. you’ll try walking or employing a stationary bicycle. Or consider taking a dip. Swimming and exercising in warm water may sense good on stiff joints. During a gout attack, rest, and don’t exercise. In between gout flare-ups, low to moderate-intensity exercise may help decrease your inflammation levels
Does turmeric help gout?
If you’ve got gout, try turmeric as a home remedy. It is most active chemical, curcumin, has potent anti-inflammatory and antioxidant properties. this might help ease gout-related inflammation and pain. When eaten in foods, turmeric is usually safe. Turmeric is one spice that’s easily available in everyone’s kitchen. it’s known to hold a property called curcumin which fights inflammation. aside from this, it also has anti-inflammatory and antibiotic properties. Drinking turmeric milk helps plenty in controlling high uric acid and maintains blood pressure.
What is the difference between arthritis and gout?
Both cause pain, swelling, and stiffness of the joints which may limit your range of motion. However, the cause differs. RA is an autoimmune disorder, which suggests the body’s own immune system attacks the joints, whereas the pain of gout is thanks to elevated levels of uric acid in the blood. Symptoms of gout occur when acid crystals accumulate in the joints and surrounding soft tissue, causing an inflammatory response within the affected areas.