Reactive Arthritis
What is Reactive Arthritis?
Reactive arthritis is joint pain and swelling started by an infection in another aspect of the body most frequently the intestines, genitals, or urinary tract. This condition generally targets the knee joints, ankles joints, and feet.
Inflammation also can involve the skin, eyes, and the tube that brings urine out of the body (urethra). Yet, reactive arthritis was sometimes known as Reiter’s syndrome. It forms most frequently between ages 20 and 50.
Synonyms of Reactive Arthritis
Fiessinger-Leroy disease
Reiter’s syndrome
Epidemiology
Reactive arthritis is fairly infrequent, and the incidence in population-based investigations is said to be 0.6 to 27 per 100,000. Reactive arthritis is more familiar in adult men in the second and third decades of their life.
Approximately 1-3% of people with nonspecific urethritis will conceive an attack of arthritis. General, higher disorder activity and worse available ability are seen in the lower socioeconomic people.
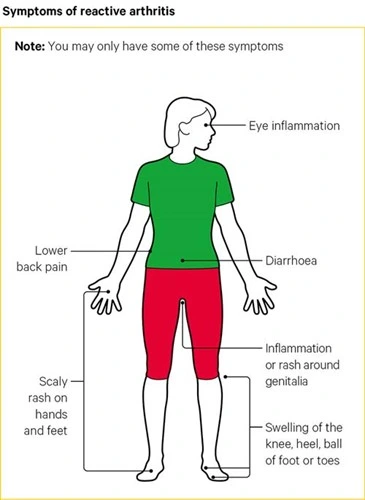
What are the Symptoms of Reactive Arthritis?
Familiar inflammation areas in reactive arthritis
The signs and symptoms of reactive arthritis commonly begin 1 to 4 weeks after the disclosure of a triggering infection. They might involve:
- Joint Pain and stiffness. The joint or junction pain associated with reactive arthritis most generally happens in the knee joint, ankle joints, and feet. Pain may also appear in the low back, heels, or buttocks.
- Eye inflammation. Many individuals who have reactive arthritis also create eye inflammation (conjunctivitis).
- Urinary problems. Risen frequency and distress during urination may happen, as can inflammation of the prostate gland or cervix.
- Inflammation of tendons and ligaments where they connect to bone (enthesitis). This occurs most frequently in the heels and the sole of the feet.
- Swollen toes or fingers. In some patients, toes or fingers might evolve so swollen that they appear like sausages.
- Skin problems. Reactive arthritis can impact the skin in a combination of ways, involving mouth sores and inflammation on the soles of the feet and palms of the hands.
- Low back pain. The pain grows to be more harmful at night or in the light.
Other symptoms
Joint or junction pain and swelling are the major symptoms of reactive arthritis. Nevertheless, it can induce other problems, like:
- scaled rashes over your hands or feet
- diarrhea, which may begin occasionally before the reactive arthritis
- mouth ulcers
- stinging and occasionally discharge when you wee (known as urethritis); this is induced by inflammation of the urethra
- a sore rash over the ending of your penis
- weight loss
- fever
What are the Causes of Reactive Arthritis?
The most familiar causes of reactive arthritis involve:
- stomach disturbances
- diarrhea
- further infections in the gut
- a throat infection – generally induced by streptococcus bacteria.
- slapped cheek syndrome
- glandular fever.
- The infection that induces reactive arthritis can be so mild that you may not sense unhealthy until you’re conscious of the pain in your junctions or joints.
It can also pursue an infection of the genitals or a sexually transmitted infection (STI), like chlamydia.
Chlamydia has no noticeable symptoms, particularly in females, but may cause discomfort when passing urine or a release from the vagina or penis. If you’re nervous, talk to your doctor or a sexual health clinic.
We don’t yet understand why some patient obtains reactive arthritis, but we do understand that it’s related to a gene that some patients inherit, known as HLA-B27. These patients appear to be more possible to conceive reactive arthritis and to bring it more than once in their life.
Risk factors
Specific factors raise your risk of reactive arthritis:
Age. Reactive arthritis appears most often in grown-ups between the ages of 20 and 40.
Sex. Females and males are equally probable to invent reactive arthritis in reaction to foodborne infections. Yet, males are more likely than females to produce reactive arthritis in reaction to sexually transmitted bacteria.
Hereditary factors. A detailed genetic marker has been related to reactive arthritis. But most patients who have this feature never create the condition.
Associated Co-morbidities and Systemic Involvement
Musculoskeletal presentations are acute inflammatory arthritis, inflammatory back aches (in extreme patients), and enthesitis. Enthesitis is pain and inflammation at the insertion point of tendons and ligaments at the bony area. Dactylitis or “sausage digit”, plantar fasciitis, and Achilles tendinitis are the most familiar areas.
Skin lesions are very similar to those of psoriasis
Constitutional symptoms involve malaise, fatigue, fever, and weight loss
Cardiovascular involvement with aortic insufficiency, aortitis, and conduction defects happens infrequently.
Reactive arthritis is associated with and may be the presenting symptom of HIV. It is likewise associated with or aggravated by Salmonella, Shigella, Campylobacter, Yersinia, and Chlamydia.
Differential Diagnosis
The physician or doctor should be capable to rule out diseases that present with equal clinical conclusions. The most familiar differential diagnosis should involve:
- Gonococcal arthritis
- Gouty arthritis
- Still disease
- Septic arthritis
- Rheumatic fever
- Psoriatic arthritis
- Ankylosing spondylitis
- Rheumatoid arthritis
- Immunotherapy/immunization-related arthropathy
- Secondary syphilis
- Tubercular arthritis
Diagnosis
How is reactive arthritis diagnosed?
The procedure begins with a health record and a physical examination. Diagnosis can be challenging. This is because there are no particular tests that can verify the need. Some blood examinations may be accomplished to rule out other diseases, like rheumatoid arthritis and lupus. Other tests may involve:
- Erythrocyte sedimentation rate (ESR or sed rate). This test examines how fast red blood cells sink to the base of a test tube. When swelling and inflammation are current, the blood’s proteins plod jointly and evolve weightier than usual. They drop and settle quickly at the base of the test tube. The quicker the blood cells fall, the more intense the inflammation.
- Tests for infections. This contains a test for chlamydia. It may also contain tests for other infections that are connected to reactive arthritis.
- Joint aspiration (arthrocentesis). A small sampling of the synovial fluid is carried from a joint or junction. It’s experimented to see if bacteria, crystals, or viruses are present.
- Urine and stool samples. These are utilized to examine for bacteria or other signs of the condition.
- X-rays. This test utilizes a small quantity of radiation to make images of bones, tissues, and organs. X-rays are utilized to examine for swelling or damage to the joint or junction. This can scan for indications of spondylitis or sacroiliitis.
- Gene testing. An examination may be done to scan for HLA-B27.
Treatment of Reactive Arthritis
Medical Treatment
Treatment will lean on your age, symptoms, and general health. It will also depend on how hurtful the situation is. Treatment may also involve:
- Antibiotics to manage infection
- Nonsteroidal anti-inflammatory drugs to decrease inflammation
- Corticosteroids to decrease inflammation
- Immunosuppressive drugs like methotrexate prevent inflammation
- Strong biological immunosuppressants are offered as a shot
- Rest to reduce aches and inflammation
- Activity to maintain muscles and enhance joint function
Physiotherapy Treatment
Physical Therapy is useful during the healing stage of the disorder (after the worsening of symptoms has ended). Physical Therapy should pursue a program equal to that provided to people with arthritis.
Patient education – this is required to help joint safety and good body mechanics when conducting daily activities to support joint goodness.
Exercise regimen – that involves regular aerobic exercise, as well as activities that encourage the joint range of movement and muscle build-up should be utilized.
Aerobic activity should involve low-impact exercises, like walking, swimming, or a recumbant cycle, relying on the people’s cardiovascular status.
Strengthening should target muscles covering the involved joints to enhance its asset system.
for acute joint inflammation, supply suggestions to avoid overuse.
If enthesitis is present, heel aid and orthosis can be thought to reduce pain and thus enhance mobility. You may decide to suggest a short period of non-weight bearing, to reduce the inflammation and determine the force of the body on the inflamed junctions or joints.
Stretching and range of motion activities should be conducted to control muscle atrophy, particularly if several joints or junctions are affected. The purpose of physiotherapy is to avoid immobility and malformations and to encourage mobility and strength.
When healing takes place, people must be suggested not to overload their joints or junctions too soon, to avoid little traumas which can cause a relapse.
Immobilization and lethargy are frustrating as they can lead to contractures, reduced range of motion, reduced muscle strength, joint stiffness, and reduced flexibility, as well as overall reduced cardiovascular fitness, which can cause a waterfall impact on other body systems. The purposes of treatment should involve pain relief, improved actions of daily living, decrease joint swelling, and precluding joint or junctions injury and disability.
Lying knee hold
This activity maintains your thighs while bringing stress off your knees. Lie flat on the bed with your back on the floor. With both your knee joints straight, force the back of your right knee joint down firmly into the bottom by bending your thigh muscles. Maintain this position for 5 seconds, then soften and change to the other knee joint.
Attempt doing 5 reps of this activity 3 times per day.
If lying on the ground is too painful, you can lie on a mattress instead.
Star Touch
This is an altered version of a lunge that places less stress on your knee joints. Plus, it can assist you with your balance. Stand on one leg, flexing your knee joint just barely to maintain your balance. Imagine a 7-point star on the ground around you, choose up your other leg, and indicate your toe. Attempt to wipe all the points of the star on one side before changing to the other leg.
Attempt doing this 2 to 3 times per leg every day.
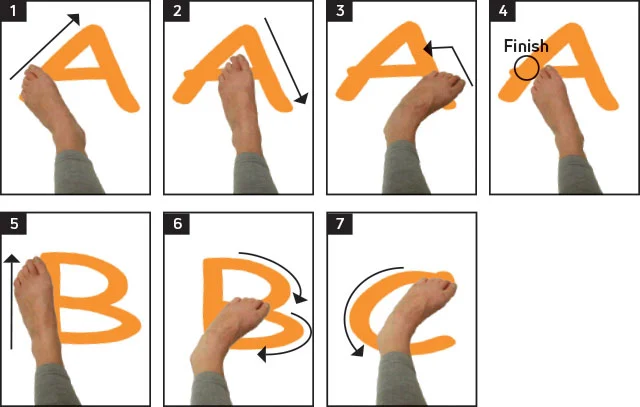
Ankle alphabet
Extend and strengthen your ankle joint at the exact time. Lie on your back in the supine position or sit in a chair in a sitting position with your back straight. Raise one leg and draw the alphabet with your toes as you bend your ankle joint. Then, do the exact on the different legs.
Attempt doing 1 set of the alphabet per leg once every day.
Standing calf raises
Boost your calves to bring stress off your ankle joints. Stand with your feet in a standing position about hip-width separated. Gradually raise yourself up as tall as you can onto your tip-toes, then gradually decline your heels down. Recount this calf lift up to 10 times, or more if you can do it.
If you’re having a problem maintaining your balance, hang onto a wall or the back of a chair for equilibrium.

Flex and point
Try out your ankle joints for added mobility. Lie on your back in a supine position with your legs straight out and your heels on the bottom. Bend your feet directly up so they point toward the roof, then gradually point your toes out from you as far as likely. Maintain this position for 3 seconds, then repeat.
Accomplish this exercise 10 times per day.
Wall push
This activity works your ankle muscles and leg muscles. Sit down in a chair in a sitting position subsequent to a wall with your feet flat on the bottom. Press the right side of your right foot up opposite to the wall, then force your foot exterior into the wall. Maintain this for 8 seconds, then repeat it 10 to 12 times before changing to your further foot.
You can also attempt this activity by twisting an opposition band around your right foot and maintaining the end of the band in your left hand. Gradually push outside out from the band, sensing the opposition in your ankle.
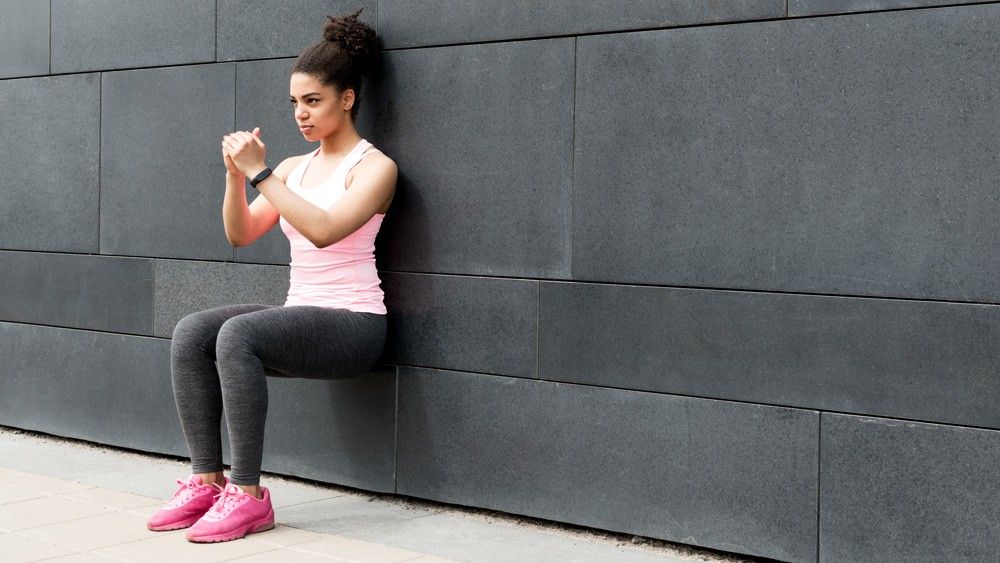
Knee bends
This squat divagation delivers support while boosting your legs. Stand approximately 12 in (30 cm) far from a wall with your feet about hip-width separated. With your back encountering the wall, gradually flex your knees, and glide your backside along the wall for help (and to assist you to maintain your balance). Stop flexing when your knees are roughly to go over your toes, then gradually glide back up along the wall.
Attempt doing about 10 repetitions 3 times in a row.
For a smoother motion, put an activity ball between your back and the wall.
Thigh contractions
Boost your quads to bring the stress off your knee joints. Sit in a comfortable chair in a sitting position with your back straight and your feet flat on the floor. Gradually straighten and lift your right leg, controlling when it’s totally straight. Press your right thigh muscles and maintain the position for 15 seconds, then drop your leg down and change sides. This might sense like you aren’t doing much, but you’ll see your quads reaching stronger in no time.
Attempt doing 3 sets of 15-second recurrences on both legs.
To complete this activity harder, attempt wearing a little ankle poundage on both legs.
Straight leg raises
Perform your thighs and your hips at the exact time. Sit in a chair in a sitting position with your feet lying on the bottom and your back straight. Gradually lift and straighten your right leg, bending your foot to point your toes upward. Maintain your leg lifted and proceed it gently up and down 10 times, but don’t allow your foot to touch the bottom. Then, change to the further leg.
Attempts 3 sets of 10 repetitions per leg.
Maintaining the pressure in your leg will assist to strengthen your muscles quickly, which will save your knee joints or junctions as you exercise or play sports.

Squats
Make the muscles in your thighs and your glutes. If you’ve done squats before, you understand simply how well they can tone and make leg muscles. Stand with your feet in a standing position shoulder-width separated and your toes meeting barely outward. Gradually reduce yourself by flexing your knee joints, transmitting your back end backward. Stop flexing before your knee joints extend over your toes, then gradually raise back up.
Attempt doing 3 sets of 10 repetitions.
If you have knee issues, use alert with squats. They’re great for making leg muscles, but they can also put a lot of pressure on your knee joints.

Lunges
Perform one leg at a time to create muscle in your thighs. Stand with your feet in a standing position shoulder-width separated, then step ahead with your right leg. Lower your back knee to flex toward the bottom and maintain your forward knee straight over your ankle joint. Then, press your upper legs and your glutes to produce a standing position before changing sides. You can complete this exercise with slightly more difficulty by having small dumbbells in each hand.
Attempt doing 3 sets of 5 repetitions per leg.
If you have a problem keeping your balance in a lunge, grab onto a chair for help.

How to Prevent Reactive Arthritis?
Genetic factors seem to recreate a role in whether you’re probably to create reactive arthritis. Though you can’t alter your genetic makeup, you can decrease your vulnerability to the bacteria that may conduct to reactive arthritis.
Keep your meals at valid temperatures and cook them correctly. Doing these items allow you to avoid the many foodborne bacteria that can cause reactive arthritis, involving shigella, salmonella, yersinia, and campylobacter. Some sexually transmitted infections can activate reactive arthritis. Use condoms to assist to reduce your risk.
Tips to reduce your risk of infection
- Try to avoid close touch with individuals you know have an infection.
- Clean your hands regularly and bring about a small bottle of antibacterial hand gel.
- Maintain your mouth clean by brushing your teeth daily.
- Stop smoking if you’re a smoker.
- Make sure your food is kept and organized correctly.
- Attempt to maintain your house neat and clean, particularly the kitchen, bathrooms, and toilets.
Living with reactive arthritis
As well as specified treatments, there are several things you can do yourself.
Rest and exercise
When your joints or junctions are inflamed and hurting, you can sense fatigued and normally unwell. Fatigue plays a significant role in reactive arthritis and can have a tremendous effect on all parts of your life. It’s essential that you and the people near you remember this.
It’s equally as necessary to maintain moving. You could try:
- swimming in a heated pool – this permits you to exercise while the water keeps your weight
- stretching exercises – support the muscles and tendons that keep the joint or junction strong and flexible
- speaking to your line supervisor regarding working shorter hours
- questioning whether you can avoid any actions that are too challenging
- creating your workstation nicely fits your situation.
- Your doctor or physician can guide you to a physiotherapist or occupational therapist for detailed advice.
Obtaining a good night’s rest and identifying when you require to relax is really essential to your healing. If you’re seeing it hard to wind down relaxation techniques, like breathing activities, mindfulness, or meditation, may benefit you.
A proper bedtime habit can also cause you to feel okay. Attempt to get an early night and give yourself an hour before to have a warm bath and rest, attempt to avoid utilizing your computer, phone, or TV in that hour, as they can disrupt your rest.
Diet
There is no exact diet established to support reactive arthritis, but a well-balanced diet is essential to your general health and well-being.
Some patients say rose hip section and fish body oil decrease their demand for anti-inflammatory medications. They are understood to help your immune system and help reduce inflammation and joint or junction damage.
Complications
Complications of Reactive arthritis involve:
- Recurrent arthritis (15 to 50%)
- Chronic arthritis or sacroiliitis
- Ankylosing spondylitis (30 to 50% if the peoples are also HLA-B27positive)
- Urethral stricture
- Aortic root necrosis
- Cataracts
- Cystoid macular edema
Prognosis
Reactive arthritis generally has a self-limited duration, and the symptoms determine within 3 to 5 months. Symptoms lasting the past 6 months show a chronic element of the condition. Sacroiliitis is the most typical chronic joint or junction involvement. Peoples who are HLA-B27 positive have a more increased risk of repetition of ReA. 15-30% of people with ReA can create long-term arthritis or other joint or junctions abnormalities. The presence of hip involvement, unresponsiveness to NSAIDs, and ESR more significant than 30 portend a worse result.
FAQ
Why is Reactive Arthritis considered a systemic rheumatic disease?
It is regarded as a systemic rheumatic disease because it involves a combination of other organs like the mouth, eyes, skin, joints, heart, kidneys, and lungs.
Why are men more prone to Reactive Arthritis compared to women?
It is because they are more tending to be contaminated by STD-causing organisms which in favor could lead to Reactive Arthritis. In females, the condition is especially milder and may appear as a consequence of food poisoning.
What aggravates reactive arthritis?
Reactive arthritis is joint or junction pain and swelling activated by an infection in another part of the body most frequently the intestines, genitals, or urinary tract.
Can stress cause reactive arthritis?
The longer you’re disclosed to stress, the more damaging the inflammation can evolve. In a PLoS One analysis, patients with RA recognized tension as a trigger for illness flare-ups. Arthritis symptoms donate to stress, particularly when they’re unrelenting. Persistent pain, fatigue, and inadequate sleep create a nasty cycle.
How long does reactive arthritis stay?
Reactive arthritis is a kind of inflammatory arthritis. Unlike other kinds of inflammatory arthritis, for many individuals, reactive arthritis lasts a relatively short quantity of time – generally around three months to a year. Nevertheless, some individuals find it lasts longer and can have unexpected flare-ups years after they first contact it.





2 Comments