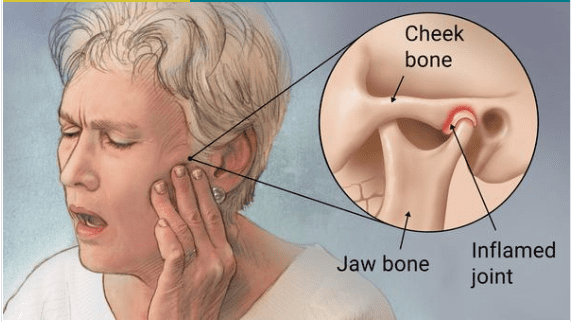
Arthritis of the Temporomandibular Joint
What is Arthritis of the Temporomandibular Joint?
Temporomandibular Joint arthritis is characterized by chronic wear and tear (degeneration) of the TM Joint hard and soft tissues of the joint.
The temporomandibular joint (TMJ) is the joint that attaches your mandible (lower jaw) to your skull. The joint can be located on both sides of your head in front of your ears. It permits your jaw to open and close, allowing you to speak and eat.
What are the types of arthritis that can involve your jaw?
Osteoarthritis
Osteoarthritis is a familiar form of degenerative arthritis, which can involve any joint or junction in your body. It’s associated with joint overuse, and it evolves more expected as you age.
Osteoarthritis of the jaw is marked by the collapse of the hard and soft tissues near the jaw joints or junctions. This can alter the shape and functioning of the jaw.
Jaw injury may be on one or both sides of the jaw.
Rheumatoid arthritis
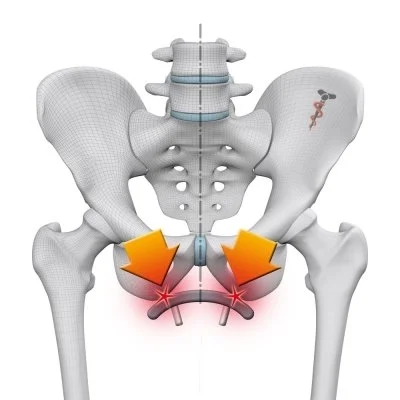
Rheumatoid arthritis (RA) is an autoimmune disorder that causes your resistant system to attack healthy tissue striping your joints or junctions. It’s a chronic inflammatory disease.
Jaw symptoms generally appear in the later phases of RA. Both sides of the jaw may be involved.
In a 2007 analysis of patients with RA, near to 93 percent of them had TMJ symptoms or collapse of the jaw bone. The same analysis found that the severity of the TMJ disease was connected to the RA severity.
Psoriatic arthritis
Psoriatic arthritis (PsA) is an inflammatory joint or junction disease that happens in approximately 30 percent of patients who have the skin disease psoriasis. It’s an autoimmune disease that’s supposed to conduct in families.
PsA is a chronic disease, but symptoms may arrive and go. If not managed early on, it can harm the jaw irreversibly, as reported in a 2015 analysis.
PsA is a spondyloarthritis kind of arthritis. Other kinds of arthritis in this group may even cause TMJ conditions.
The same 2015 analysis of 112 patients some with psoriasis only and some with both psoriasis and PsA located that both groups had symptoms of TMJ diseases.
Infectious arthritis
Infection of the temporomandibular joint (TMJ) may result from the direct attachment of contiguous infection or hematogenous reach of bloodborne organisms. The joint location is inflamed, and jaw motion is fixed and painful. Local signs of disease associated with proof of a systemic disorder or with an adjacent infection propose the diagnosis. X-ray effects are negative in the early phases but may display bone collapse later. If suppurative arthritis is presumed, the joint or junction is aspirated to verify the diagnosis and to determine the causative organism. Diagnosis must be made rapidly to stop endless joint or junction harm.
Treatment involves proper hydration, antibiotics, pain control, and movement restriction. Parenteral penicillin G is the medicine of selection until an exact bacteriologic diagnosis can be made on the basis of culture and sensitivity testing. For methicillin-resistant Staphylococcus aureus (MRSA) conditions of the oral structures, IV vancomycin is the antibiotic of preference. Suppurative infections are aspirated or marked and drained. Once the infection is prevented, passive jaw-opening activities assist to prevent scarring and limitation of movement.
Traumatic arthritis
Infrequently, acute injury (like due to hard tooth extraction or endotracheal intubation) may lead to arthritis of the TMJ. Pain, tenderness and boundary of mandibular movement happen. Diagnosis is established primarily on record. X-ray effects are negative except when intra-articular edema or hemorrhage enlarges the joint or junction space. Treatment involves oral nonsteroidal anti-inflammatory drugs (NSAIDs), corticosteroids, a soft diet, application of heat, and restriction of jaw motion.
Infectious arthritis, osteoarthritis, traumatic arthritis, rheumatoid arthritis, and secondary degenerative arthritis can involve the temporomandibular joint.
Secondary degenerative arthritis
This arthritis generally forms in patients (usually females) aged 20 to 40 years with a record of trauma or persistent myofascial ache syndrome. It is marked by the restricted opening of the mouth, unilateral ache during jaw motion, joint or junction tenderness, and crepitus. When it is associated with myofascial ache syndrome, symptoms polish and wane.
Unilateral joint or junction involvement allows for determining secondary degenerative arthritis from osteoarthritis. Diagnosis is established on x-rays, which, as in osteoarthritis, commonly offer spurring, condylar flattening, lipping, or erosion.
The remedy is conservative, as it is for myofascial ache syndrome, although arthroplasty or high condylectomy may be required. An oral device (occlusal splint [mouth protection]) generally reduces symptoms. The device is worn continuously, excluding during meals, oral hygiene, and device cleaning. When symptoms settle, the size of time that the device is worn each day is slowly decreased. Intra-articular injection of corticosteroids may reduce symptoms but may damage the joint or junction if repeated frequently.
But those with PsA had particularly more symptoms of:
jaw opening issues
teeth nibbling and gripping
jaw noises
What are the symptoms of arthritis in your jaw?
The symptoms of arthritis in your jaw can vary relying on the harshness of arthritis. Some of the most familiar symptoms involve:
- ache, which can be a dull pain or a sharp stab when you push your jaw
- inflammation in or near your jaw junctions or joints
- limited joint motion or locking of your jaw
- jaw tenderness
- jaw stiffness, particularly in the morning
- a creaking, clicking, grating, or crunching noise (known as crepitus)
- problem chewing
- facial pain or pain near your ear or neck
- headaches
- tooth pain
Causes of Jaw pain
Jaw pain can include many causes, and occasionally there can be more than one cause. Pain in your jaw isn’t consistently associated with bone injury.
Besides arthritis, jaw ache may also be caused by:
- Repetitive movement. Some familiar culprits involve:
- regular gum chewing
- clenching or grinding your teeth
- fingernail biting
- Injury. This can be due to:
- an infection, such as a sinus infection
- a blow to the jaw
- stretching the jaw, such as with a dental method
- insertion of tubes during a medical approach
- Physical issues. Examples can involve:
- misalignment of your teeth
- inherited structural jaw issues
- connective tissue disorders
- Medications. Some prescription medications may impact your jaw muscles and cause pain.
- Emotional factors. Anxiety, depression, and stress can cause tension, tense jaw muscles, or cause jaw pain worse.
Risk factors
Factors that may raise the risk of inventing TMJ issues involve:
- Different kinds of arthritis, like rheumatoid arthritis and osteoarthritis
- Jaw injury
- Long-term (chronic) grinding or clenching of teeth
- Certain connective tissue disorders cause issues that may involve the temporomandibular joint
Diagnosis
Your doctor or dentist will examine your symptoms and discuss your jaw. He or she will likely:
- Attend to and sense your jaw when you open and close your mouth
- Mark the range of movement in your jaw
- Press on locations near your jaw to determine areas of pain or distress
If your doctor or dentist doubts a situation, you may require:
- Dental X-rays to display your teeth and jaw
- CT scan to supply detailed pictures of the bones affected in the joint
- MRI to indicate issues with the joint’s disk or covering soft tissue
- TMJ arthroscopy is occasionally used in the diagnosis of a TMJ condition. During TMJ arthroscopy, your doctor or physician inserts a small narrow tube (cannula) into the joint or junction space, and a small camera (arthroscope) is then inserted to regard the location and to assist to specify a diagnosis.
Treatment of Arthritis of the Temporomandibular Joint
In some patients, the symptoms of TMJ conditions may go out without medicine. If your symptoms continue, your doctor or physician may suggest a combination of treatment choices, frequently more than one to be done at the same time.
Medications
Along with other nonsurgical management, these drug choices may assist to reduce the pain associated with TMJ conditions:
- Pain relievers and anti-inflammatories. If over-the-counter pain drugs aren’t sufficient to reduce TMJ pain, your doctor or dentist may specify more powerful pain relievers for a little time, like prescription-strength ibuprofen.
- Tricyclic antidepressants. These drugs, like amitriptyline, are used mainly for depression, but in lower doses, they’re occasionally used for pain ease, bruxism management, and insomnia.
- Muscle relaxants. These kinds of medications are occasionally used for a few days or weeks to assist to reduce pain caused by TMJ diseases produced by muscle spasms.
Physiotherapy treatment for Arthritis of the TM Joint
Nondrug therapies for TMJ disorders involve:
Oral slings or mouth protection (occlusal devices). Frequently, patients with jaw aches will profit from wearing a smooth or well instrument inserted over their teeth, but the causes why these machines are useful are not well-understood.
Physical therapy. Along with activities to stretch and boost jaw muscles, treatments might involve ultrasound, moist heat, and ice.
Counseling. Information and counseling can assist you to understand the aspects and behaviors that may worsen your pain, so you can bypass them. Examples involve teeth clenching or grinding, relying on your chin, or biting fingernails.
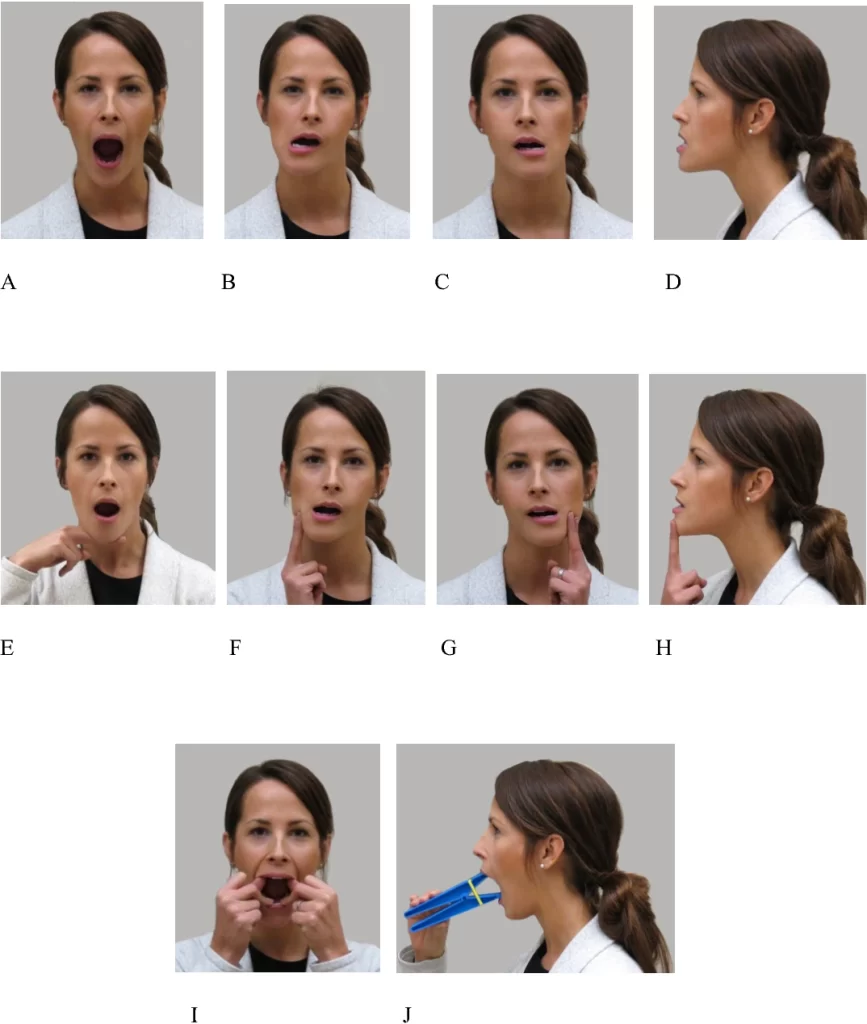
Relaxed jaw exercise
Relax your tongue smoothly on the roof of your mouth behind your upper front teeth. Permit your teeth to arrive separated while relaxing your jaw muscles.
Goldfish exercises (partial opening)
Put your tongue on the top of your mouth and one finger in front of your ear where your TMJ is found. Take your middle or pointer finger on your chin. Decline your lower jaw center and then close. There should be mild opposition but not ache. A variation of this activity is to put one finger on each TMJ as you decline your lower jaw center and closed similarly. Accomplish this movement six times in one set. You should accomplish one set six times every day.
Goldfish exercises (full opening)
Maintaining your tongue on the top of your mouth, put one finger on your TMJ and a further finger on your chin. Decline your lower jaw fully and back. For a variation of this activity, put one finger on per TMJ as you fully decline your lower jaw and back. Accomplish this movement six times to finish one set. You should finish one set six times every day.
Chin tucks
With your both shoulders back and chest up, stretch your chin directly back, making a double chin. Keep for three seconds and repeat 10 times.

Resisted opening of the mouth
Put your thumb beneath your chin. Open your mouth gradually, pressing gently against your chin for the opposition. Keep for three to six seconds, and then close your mouth gradually.

Resisted closing of the mouth
Press your chin with your index and thumb with one hand. Close your mouth as you put slowly pressure on your chin. This will assist boost your muscles that allow you to chew.
Tongue up
With your tongue adjoining the top of your mouth, gradually open and close your mouth.
Side-to-side jaw movement
Place an inch object, like piled tongue depressors, between your front teeth, and gradually shift your jaw from side to side. As the movement evolves more comfortably, raise the consistency of the thing between your teeth by piling them on the roof of the other.

Forward jaw movement
Place an inch of a thing between your front teeth. Push your bottom jaw forward so your lowest teeth are in front of your head teeth. As the movement evolves more comfortable, raise the thickness of the thing between your teeth.

Relaxation exercises
TMJ ache is frequently the effect of tension-producing pressure. Simple relaxation activities can assist.
Here are two relaxation exercises:
- Gradually inhale, permitting your stomach instead than your chest to extend. Exhale gradually while creating your exhalation last almost as long as your inhalation. Replay 5-10 times.
- While sitting or lying in a comfortably subsidized position, tense and remove tension from per muscle in your body. Start with the feet and perform upwards to the head.
- This second activity is a progressive relaxation activity to assist individuals to become more conscious of places of tension. It may also provide them with the talent to intentionally remove that tension.
Stretching exercises
Stretching exercises can assist with TMJ aches during an explosion. They lessen muscle and joint or junction tension, suggesting longer-term relief:
- Put the tip of your tongue on the top of your mouth. Open your mouth as broad as you comfortably can, and maintain for 5-10 seconds.
- Put the tip of your tongue on the top of your mouth. Slide your lower jaw out as distant as it will go and then back in as distant as it will go. Keep for 5-10 seconds per position.
- Gradually and steadily open your mouth as broad as it will comfortably open, with your tongue in an impartial position. Keep for 5-10 seconds then close your mouth. Subsequent, open your mouth barely and slide your lower jaw back and along 5-10 times.
- Shut your mouth. With your head looking straight forward, glimpse to the right with your eyes solely. Expand your inferior jaw to the left and keep for 5-10 seconds. Repeat on the opposing side.
- Put a thin thing, like a pencil or paintbrush, in between your front teeth. Glide your lower jaw ahead so that the thing relaxes in between your back teeth and front teeth. Keep for 20 seconds.
- As the fifth activity evolves more comfortably, patients can use broader things to divide their front and back teeth.
Surgical or other procedures
When other strategies don’t support, your doctor or physician might recommend procedures like:
- Arthrocentesis. Arthrocentesis is a minimally interfering method that involves the insertion of small syringes into the joint or junction so that liquid can be flushed via the joint or junction to clear the waste and inflammatory byproducts.
- Injections. In some patients, corticosteroid injections into the joint or junction may be useful. Rarely, injecting botulinum toxin type A (Botox, others) into the jaw muscles utilized for chewing may reduce aches associated with TMJ conditions.
- TMJ arthroscopy. In some patients, arthroscopic surgery can be as useful for treating different kinds of TMJ conditions as open-joint or junction surgery. A little thin line (cannula) is put into the joint or junction space, an arthroscope is then inserted and tiny surgical tools are operated for surgery. TMJ arthroscopy has more irregular risks and difficulties than open-joint or junction surgery, but it has some restrictions as well.
- Modified condylotomy. Modified condylotomy manages the TMJ indirectly, with surgery on the mandible, but not in the joint or junction itself. It may be useful for the treatment of aches and if locking is experienced.
- Open-joint surgery. If your jaw ache does not settle with more-conservative therapies and it occurs to be caused by a structural issue in the joint or junction, your doctor or dentist may recommend open-joint or junction surgery (arthrotomy) to restore or replace the joint or junction. Nevertheless, open-joint or junction surgery affects more risks than other methods do and should be evaluated very carefully, after examining the positive and negative.
If your doctor or physician suggests surgery or other methods, be sure to examine the possible advantages and risks, and ask what all your choices are.
Alternative medicine
Complementary and alternative treatment methods may assist control of the chronic pain frequently associated with TMJ conditions. Examples involve:
Acupuncture. A professional trained in acupuncture treats chronic aches by inserting hair-thin syringes at precise areas on your body.
Relaxation techniques. Intentionally delaying your breathing and bringing deep, steady breaths can assist relax tense muscles, which can decrease aches.
Biofeedback. Electronic instruments that observe the tightness of precise muscles can assist you to practice useful relaxation techniques.
Do any self-care measures help?
If your jaw ache isn’t too intense and isn’t interrupting your day-to-day life, you may want to try reducing your jaw pain with self-care steps.
Some alternatives involve:
- Resting your jaw. Avoiding opening your jaw broad and attempting to stick to eating more delicate foods that you don’t have to chew too much may supply relief.
- Ice or heat therapy. Using a cold compress can reduce inflammation, while a heating pad or hot water bottle may assist relax your jaw muscles.
- Jaw exercises. Accomplishing precise jaw exercises may assist to boost your jaw muscles and enhance the motion of your jaw joints or junctions.
- Relaxation exercises. If you grip your jaw when you’re worried, relaxation activities may assist you in sense more relaxed and slightly tense.
- Massaging your jaw muscles. Massaging your jaw muscles may assist to enhance blood flow and speed up recovery.
- Wear a mouthguard at night. If you’re prone to scraping your teeth when you rest, a mouthguard may assist to control this.
How to Prevent Arthritis of the Temporomandibular Joint?
Good dental care can assist to control TMJ aches by supporting tooth alignment. Cavities, damaged or missing teeth, and gum inflammation may cause the ache to be more harmful.
Individuals should brush and floss their teeth, and aspire to visit a dentist every 6 months unless suggested otherwise. Someone should ever inform their dentist if they have TMJ aches.
Some other techniques for controlling TMJ pain contain:
- detouring taffy, chewing gum, and other very chewy or difficult foods
- eating delicate food, especially if inclined to TMJ ache
- not chewing on the mouth or tongue
- It is also necessary to chew using both sides of the mouth. Some individuals with TMJ aches avoid chewing on one side because of the ache. Over the period, this causes the ache to be more harmful.
FAQ
What is the most often pathology associated with the temporomandibular joint or junction?
Degenerative joint or junction condition, or degenerative arthritis, is the most periodic abnormal situation that involves the TMJ. Primary degenerative arthritis is noticed in more senior patients and is associated with regular aging.
What is a normally expected finding when examining the temporomandibular joint?
The normal joint or junction functions relatively calmly. Hear for clicking or popping and crepitus or grinding sounds. The extent of the mandibular opening is estimated utilizing the length between the incisal edges of the upper and lower anterior teeth. Opening of smaller than 35 mm is assumed abnormal in a grown-up.
What muscle is involved in TMJ arthritis?
The muscles affected in temporomandibular conditions are the muscles of the mastication: masseter, temporalis, medial and lateral pterygoid muscles. Three major ligaments stabilize the TMJ: stylomandibular, temporomandibular, and sphenomandibular ligaments.
What nerve supplies the temporomandibular joint?
the trigeminal nerve
The innervation to the temporomandibular joint or junction is by branches from the mandibular section of the trigeminal nerve (CN V3), especially via the auriculotemporal branch, along with branches from the deep temporal and masseteric nerves.
What is special about the temporomandibular joint?
This joint or junction is unique in that it is a bilateral joint or junction that functions as one team. Since the TMJ is related to the mandible, the right and left joints or junctions must function jointly and therefore are not separate from each other. The temporomandibular joint or junction is the joint or junction between the mandible and the temporal bone of the skull.