Biceps Tendinopathy Physiotherapy Treatment & Exercise
Introduction
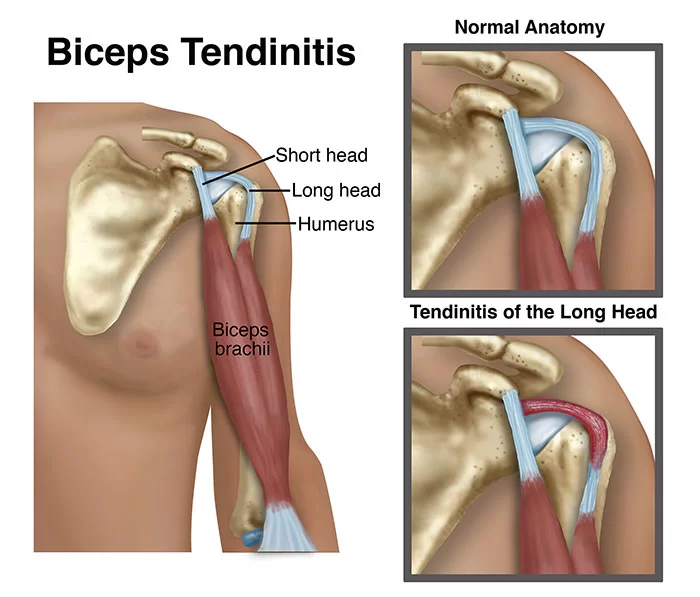
Biceps tendinopathy is a condition characterized by inflammation, irritation, or degeneration of the biceps tendon, which connects the biceps muscle to the shoulder or elbow. It is a common cause of shoulder pain, particularly in individuals who engage in repetitive overhead activities or sports that involve repetitive arm movements.
Physiotherapy plays a crucial role in the management of biceps tendinopathy, aiming to reduce pain, improve function, and restore normal strength and range of motion. The treatment approach may vary depending on the severity of the condition, individual factors, and specific symptoms.
Tendons are tough bands of tissue that connect bones to muscles. Overuse and repetitive motions can damage tendons, resulting in discomfort and reduced function. This is called tendinopathy.
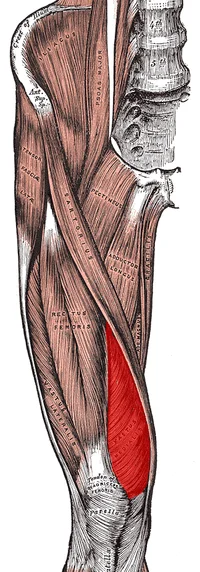
Proximal biceps tendinopathy is the inflammation of the tendon around the long head of the biceps muscle tendon. Biceps tendinitis can affect patients’ ability to perform many daily activities. The main function of the biceps muscle is elbow flexion and forearm supination. Additionally, while the arm is in external rotation, the biceps provide ten percent of the total power for shoulder abduction. The front of the upper arm’s biceps muscle is utilized for lifting, bending the elbow, and reaching over the head.
The bottom part of the biceps muscle tendon connects to a bone in the forearm. while the upper part of the tendon attaches to the front of the shoulder joint in two places. Biceps tendinopathy or even tears of the upper biceps muscular tendon can result from reaching, lifting, tugging, or throwing repeatedly.
Biceps Tendinopathy Symptoms
Patients with biceps tendinopathy typically have pain that worsens at night, pain in the front of the shoulder. Pain may increase with repetitive overhead reaching and lifting, pulling. With tendinopathy, symptoms often appear gradually over time, however, they might appear suddenly in persons with biceps rupture or tendinitis.
If a proximal biceps muscle tendon ruptures, the person will feel swelling, sudden pain, and bruising. in the lower biceps muscle tendon It may be possible to feel or see a lump. Shoulder pain is sometimes completely decrease after the rupture occurs. Surprisingly, 25 percent of muscle strength decreases after proximal biceps tendon rupture.
Causes of Biceps Tendinitis
The term “biceps tendinopathy” refers to an inflammatory tenosynovitis that most frequently affects the long head of the biceps muscle tendon as it travels through the bicipital groove in the proximal humerus. it is clinical pathology ranges from acute inflammatory tendinitis to degenerative tendinopathy. Primary shoulder pathology is more common than Primary bicipital tendinitis. causes are not well understood of primary bicipital tendinitis.
Other Associated Shoulder Pathologies Include
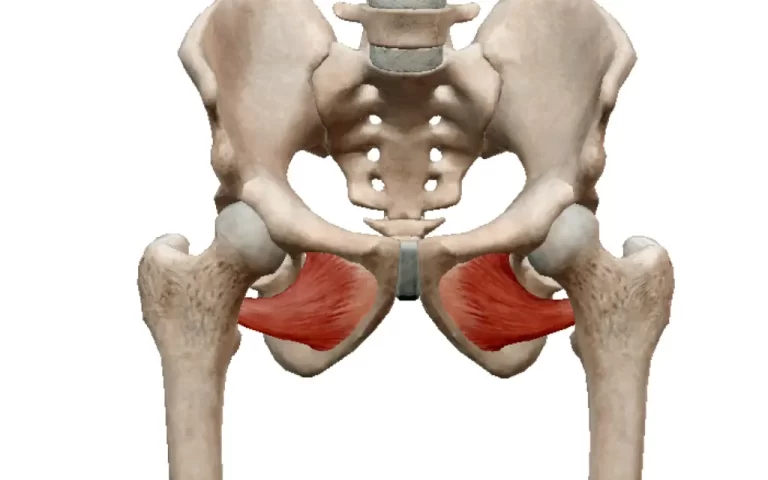
Chronic Rotator cuff tendinopathy and Chronic Rotator Cuff Tendinitis, Subscapularis injuries, LHB tendon instability/dislocation (seen in association with subscapularis injuries/tears), Direct or indirect trauma, Inflammatory conditions Internal impingement of the shoulder, Glenohumer arthritis External impingement/Subacromial impingement syndrome.
The primary Long head of biceps tendinitis represents about 5% of cases of proximal biceps pathology. Although much less common, Primary solitary cases, although considerably less frequent, are generally seen in young athletes who compete in baseball, softball, volleyball, gymnastics, swimming, and other sports.
The long head of biceps tendinopathy most frequently affects tendons with subscapularis injuries or Rotator cuff pathology. In the setting of Rotator cuff tears, 45% of cases had additional LHB instability and 90% of cases demonstrated connected LHB tendinopathy.
The first step in the pathogenesis of LHB tendinitis/tendinopathy is tenosynovitis and inflammation in its early phases as a result of constant friction, traction, and shoulder rotation. In the tendinous part of the bicipital groove, inflammation first appears.
Due to swelling and/or related hemorrhage, the tendon widens, further damaging it as it gets mechanically irritated in its small area. The consequently elevated pressure and particular traction sites make the tendon more vulnerable to pathologic shear stresses.
The synovial lining of the glenohumeral joint is also directly extended into the sheath of the biceps tendon. As a result, concurrent or antecedent RC disease might seriously endanger the LHB tendon. The LHB tendon in the bicipital groove is still movable in the early stages of the illness. A thickening, fibrosis, and vascular compromise of the LHB sheath occur as the pathophysiology progresses. The LHB tendon endures degenerative changes, and these changes eventually result in scarring, fibrosis, and adhesions that decrease the LHB tendon’s mobility.
The LHB tendon experiences increased shear stresses along its course as a result of the tendon being pathologically connected to the groove, aggravating any existing traction sites.
The LHB tendon may eventually rupture in advanced, end-stage circumstances at its origin close to the superior glenoid tubercle or when it emerges from the bicipital groove close to its musculotendinous junction.
clinical characteristics and presentation. The following are characteristics of proximal biceps tendinitis. Insidious, non-traumatic start of anterior shoulder discomfort. When the proximal biceps is unstable, clicking or audible popping can be heard.
Pain during sleep and during the night. Exacerbation of symptoms while overhead activities
shoulder pain that travels down the front arm. Sports from the past or the present, including baseball, volleyball, and other overhead games
History or current manual/physical laborer occupations
In addition, a thorough history includes a detailed account of the patient’s occupational history and current status of employment, hand dominance, history of injury/trauma to the shoulder and/or neck, and any relevant surgical history.
Differential Diagnosis
- Acromioclavicular joint pathology
- Adhesive capsulitis
- Cervical spine pathology
- Glenohumeral osteoarthritis
- Glenohumeral instability
- Humeral head osteonecrosis
- Sub-acromial Impingement syndrome
- Rotator cuff tears
- Superior labrum anterior-posterior lesions (SLAP)
- Pulley lesions.
Biceps Tendinopathy Diagnosis
Usually, a physical examination and a person’s medical history are used to diagnose biceps tendinopathy. The physician moves the injured arm through a series of motions while assessing the patient’s discomfort during the physical examination. X-rays may be advised to assist analyze the conditions that contributed to the ailment or rule out other issues but are not often useful in verifying biceps tendinopathy or rupture.
The diagnosis of biceps tendonitis can be strengthened with the use of an ultrasound examination. Magnetic resonance imaging (MRI) can produce precise pictures of the biceps tendon, although it is costly and rarely used.
Diagnostic Procedures
1. Subjective Assessment
It’s crucial to obtain a thorough history during an examination and avoid relying entirely on these tests to diagnose rotator cuff pathology, subacromial impingement syndromes, and biceps tendon pathology due to the lack of specificity in these tests.
2. Objective Assessment
Palpation: Patients with biceps tendinopathy frequently experience pain with palpation over the bicipital groove, which is particularly noticeable in 10° of internal rotation.
Strength Testing: Strength testing of the shoulder, elbow, and wrist should all be completed to ensure no significant weakness of other structures. Because biceps tendinopathy is frequently connected with shoulder injuries, there could also be rotator cuff weakness.
Yergason test – The patient must supinate against resistance while holding the arm at his or her side with the elbow flexed at 90 degrees for the Yergason test. If the discomfort is directed to the bicipital groove, the test is regarded as positive.
Neers test: involves forward flexion position, and internal rotation of the arm. If the patient experiences pain, it is a positive sign of shoulder impingement syndrome or subacromial pain syndrome.
Hawkins test – the physician inserts their forearm in a neutral posture while lifting their shoulder to a 90-degree angle and flexing their elbow to that angle. The arm supports the humerus as it rotates internally. The test is successful if the bicipital groove hurts.
Speeds test: The patient extends their elbow and supinates their forearm while they attempt to bend their shoulder against resistance. A discomfort that extends to the bicipital groove indicates a positive test.
Imaging
Radiographs including Bicipital groove view radiography. Although routine radiographs are advised, they will often be normal in LHB tendonitis instances without accompanying diseases.
MRI – The best and most economical method for assessing isolated extra-articular tendinopathy is ultrasonography
Outcome Measures – The main outcome measures of biceps tendinopathy are DASH ( arm disabilities, hand, and Shoulder) scoring, Range of motion, Visual Analogue Scale (VAS)/ Numeric pain rating scale (NPRS), Simple Shoulder Test
Medical Treatment
Conservative: Initial treatment should consist of pain management and the use of NSAIDs. Injections of steroids may be useful in controlling pain if this fails. Corticosteroid injections along the tendon sheath may be necessary for more chronic appearances. The first line of treatment should always be cautious in people with low-functioning or complex medical conditions.
A biceps or tendinosis is often carried out by arthroscopic or open incisions.
The long head of the biceps tendon is cut by arthroscopic tendinosis as part of the surgical treatment of biceps tendonitis. This maintains normal biceps function while reducing pain levels sufficiently, according to research.
Limit lifting and reaching until symptoms improve. It is safest to use the following strategies.
Lift objects close to the body. Only lift light weights below shoulder level. Do sidestroke or breaststroke when swimming. Throw balls underhand or sidearm. Do not overhand serve in tennis. Avoid rapid, ballistic movements such as shoveling. For pain, an NSAID gel or patch may be advised. These are applied to the skin. Apply ice for 10 to 20 minutes each hour as needed to reduce pain and swelling.
Physical Therapy Treatment of Biceps Tendinopathy
As with other types of tendon rehab, this could begin with isometric training if the pain is the main problem before moving on to eccentric training and finally concentric loading.
Strengthening and stretching programs are a common component of most therapy programs. Along with these techniques, therapists may also employ ultrasound, iontophoresis, deep transverse friction massage, low-level laser treatment, and heat. however, evidence for these modalities has low quality
Regarding a patient’s return to optimal function, the physical therapist must take into account both the patient’s subjective reaction to the injury and the physiological mechanisms of tissue healing. two points must be made as a preface to a discussion of the goals of treatment during injury rehabilitation.
It’s important to avoid overstretching healing tissue and implement a very gradual heavy-loading program. Controlled therapeutic stress is essential for collagen matrix production during tissue healing, but too much stress might harm new structures and hinder the patient’s recovery. To go from one stage of healing to the next, the patient must achieve specified goals. These goals might be influenced by ROM, strength, or activity. These rules must be established, and it is the physical therapist’s job to do so.
Modalities For Biceps Tendinopathy to Relieve Pain
TENS
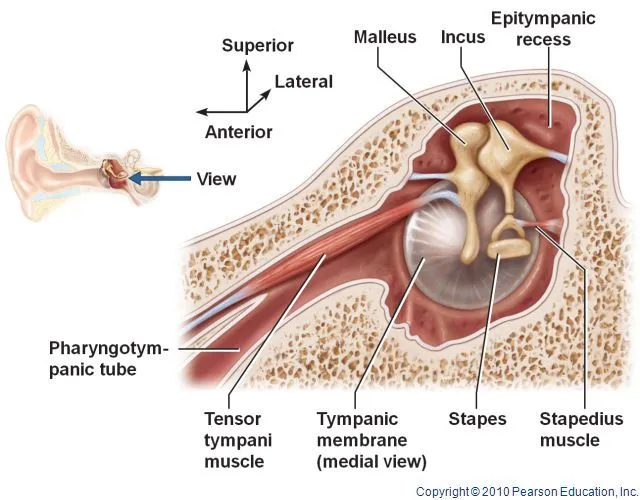
Biceps tendinopathy is treated with transcutaneous nerve electrical stimulation because it reduces discomfort, enhances muscular function, or boosts circulation. The TENS produces a current that is sent through your body via sticky pads on your back and stimulates your nerves. muscle contraction will trigger the TENS.
SWD
SWD successfully reduces symptoms, improves soft tissue healing, and relieves joint discomfort. short wave diathermy increases blood flow, Relieves pain, improves the mobility of tissues as they heal, better flexibility, and reduces inflammation.
DHT
The treatment for pain and injuries is deep heat therapy. In order to alleviate muscular spasms and increase blood flow to the injured area, heat relaxes the blood vessels and muscles. It could speed up your body’s healing process and ease discomfort.
LASER
The absorption of photons, which are connected to cytochrome C oxidase (CCO), is directly tied to the low-level laser therapy process since it is a photochemical reaction. Through this mechanism, LASER will enhance ATP synthesis and respiration rate, boosting the healing of tendon injuries. Your body’s natural healing processes are supported by LASER therapy, which speeds up recovery from injuries and severe pain.
ULTRASOUND
This modality Increased blood flow, Reduction in muscle spasms, and increased the extensibility of collagen fibers. Accelerate healing, Stretching of scars and adhesion, and reduce pain.
Exercises For Biceps Tendinopathy
Observe the advice of your healthcare provider: Always follow the detailed instructions given by your doctor and physiotherapist. They have a comprehensive understanding of your condition and can provide personalized recommendations for your recovery process.
Maintain good posture and technique when exercising: Pay close attention to your posture and technique. Injury or strain might result from using improper form or technique. Your physical therapist will give advice on how to keep your body in the right alignment and posture throughout each exercise.
slowly up the resistance: As your recovery progresses, you may gradually up the difficulty of your workouts. To avoid strain or overexertion, however, always do so while following your physiotherapist’s instructions.
Active Elbow Flexion and Extension
Gently elevate the palm of the affected side of your hand up to your shoulder while bending your elbow as far as you can. Then extend your elbow as far as possible. Repeat 15times. Do 2 sets of 15.
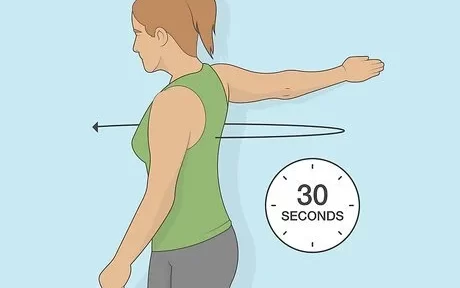
Biceps Stretch
Stand facing a wall, about 6 inches (15 centimeters) away. Perform a biceps stretch. Place your hand with the thumb towards the wall and raise your wounded arm out to the side. Maintain a straight arm. Until you experience a stretch in your, turn your body in the opposite direction of the lifted arm straight. As soon as you feel a stretch in your until turn your body in the opposite direction of the elevated arm. Hold 15 seconds. Repeat 3 times
Biceps Curl
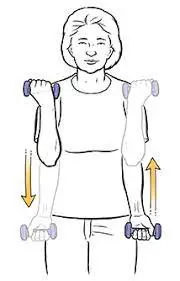
Holding a 500 gm or 1 kg weight in your hand as your comfort, stand and perform a biceps curl. Use a soup can or hammer in the absence of weight. Bring your hand (palm up) towards your shoulder while bending your elbow. Hold 5 seconds. Return to your starting posture by slowly straightening your arm. Two sets of eight to twelve should be performed.
Shoulder Flexion
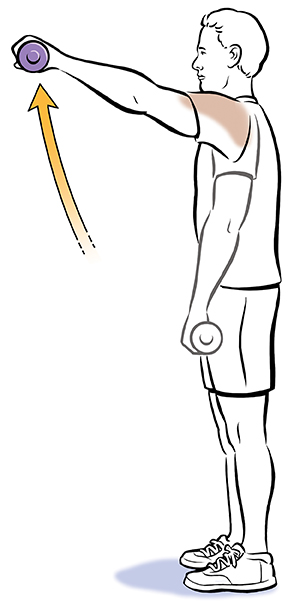
Standing with your injured arm hanging down by your side, perform a single-arm shoulder flexion. Keeping your arm Straighten your arm and extend it upwards towards the ceiling. Hold this position for 5 seconds. Do 2 sets of 8.
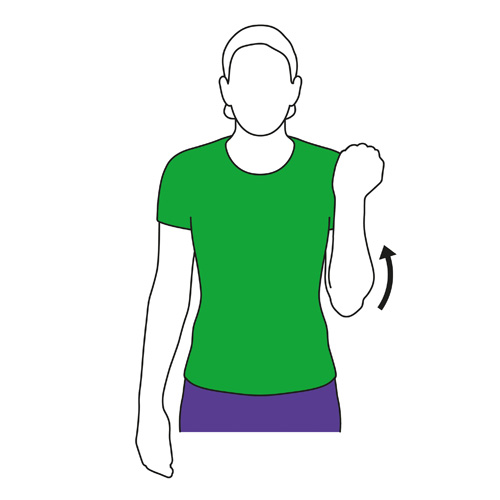
Shoulder Isometric Internal Rotation

Add weight as the activity gets easier. Resisted shoulder internal rotation: Place your injured arm closest to the door while standing sideways next to a door. Close the knot in the door at waist level after tying a knot at the tubing’s end with the hand of your affected arm, and hold the opposite end of the tube. Your damaged arm’s elbow should be bent 90 degrees.
Rotate your forearm across your body while keeping your elbow at your side. Then, slowly return to the beginning position. Keep your forearm parallel to the ground. Perform eight to twelve times in two sets.
Shoulder Isometric External Rotation
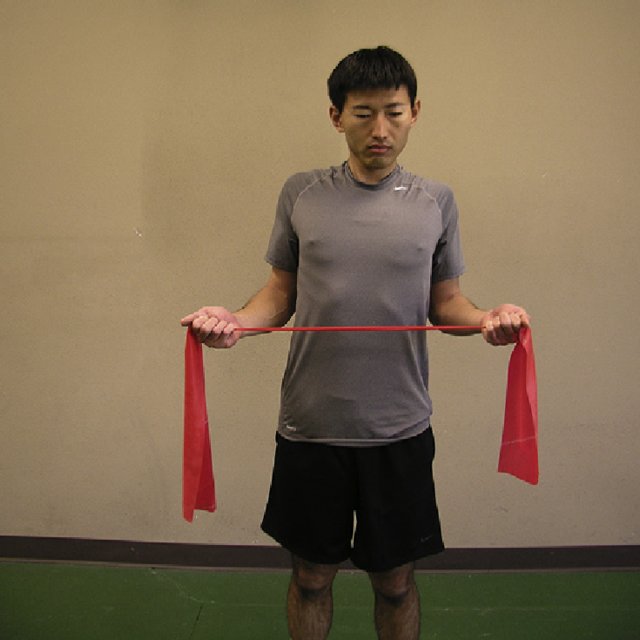
Standing sideways next to a door with your injured arm further away from the door will help with resisted shoulder external rotation. Close the knot in the door at waist level after tying a knot at the tubing’s end. With the hand of your wounded arm, hold the opposite end of the tube.
Cross your stomach with the damaged arm’s hand. Keeping Rotate your arm away from your waist while keeping your elbow at your side. Return to your starting position gradually. Make careful to maintain a 90-degree elbow bend and a parallel forearm to the ground. up to two sets of 15 repetitions and ten times in total.
Side Lying External Rotation

Laying on your side with your injured arm at your side and your elbow bent 90 degrees is known as side-lying external rotation. Raise your forearm towards the sky while keeping your elbow against your side. Hold for two seconds. Slowly lower your arm. Do 2 sets of 15.
As long as there is no pain, start out softly and raise the weight gradually.
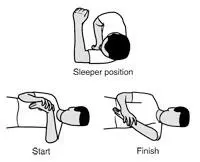
Sleeper Stretch
– Flex your hips and knees while lying on your injured side, and extend your arm straight in front of you. Your fingers should be facing upward when you bend the elbow on your afflicted side to a right angle. Then, slowly lower your arm towards the floor using your other hand. Keep your shoulder blades
lightly squeezed together as you do this exercise. Hold the stretch for 30 seconds. Repeat 3 times.
Exercise Therapy Should Include
Regaining a pain-free range of motion – PROM, Active-Assisted Range of Motion (AAROM), and shoulder manual therapy mobilization are some exercises that might help.
Proper scapulothoracic rhythm.
In the initial phases of rehabilitation, painful activities like abduction and overhead activities should be avoided as they might worsen symptoms.
A heavy, gradual loading strengthening regimen should start out with a focus on the biceps tendon, rotator cuff, and scapular stabilizers.
Summary
Remember, every individual’s condition is unique, and the treatment approach may vary. It’s essential to consult a qualified physiotherapist for a proper assessment and personalized treatment plan for your biceps tendinopathy. Early intervention and consistent adherence to the prescribed exercises can lead to better outcomes and a faster recovery.
FAQs
How long does biceps tendinopathy take to heal?
In 6 weeks to a few months, proximal biceps tendonitis often goes away without causing any lasting problems. It’s crucial to give the arm and shoulder ample time to rest, stretch, and get rehabilitation so that they can recover entirely. Resuming exercises and sports gradually might help stop the tendonitis from returning.
Can you fully recover from tendinopathy?
Generally, tendinopathy recovers completely without the need for any surgery. Rarely, nevertheless, severe untreated tendinopathy might result in tendon rupture.
Can I exercise with tendinopathy?
With an emphasis on resistance training, which has been proven to be successful in improving patient outcomes, exercise therapy is the primary modality of conservative treatment for tendinopathies
Is massage good for tendinopathy?
In general, massage treatment is effective in treating tendon ailments including tendinitis and tendinopathy/tendinosis. Friction treatment can alleviate several ailments, but each condition has a unique healing path.
Can you lift with tendinopathy?
You may still exercise your lower body muscles to improve your fitness level even if you have tendinopathy in your elbow or wrist. However, it is preferable to reduce the intensity of upper body resistance training for a week or two and concentrate on muscular flexibility.