Cervical Stenosis of spine : Physiotherapy exercise
Definition
Cervical stenosis of spine is a narrowing of the cervical spinal canal which may result in compression of the spinal cord and/or the nerve roots.
It can be caused by several things, including spondylosis (a degenerative process that results in bony overgrowths), arthritis, previous infections, or malignancy, among others. The symptoms of cervical stenosis are variable depending on the extent to which the spinal cord or nerve roots are affected.
They may include pain in the neck to shoulder region, numbness and/or tingling in the hands and fingers due to pinched nerves, muscle weakness in one or both arms, low blood pressure upon standing (orthostatic hypotension), difficulty urinating due to bladder dysfunction, and loss of bladder control (incontinence).
What is Cervical Stenosis?
- Cervical Stenosis is a compression of the spinal cord and/or the nerve roots which affect the function of the spinal cord or the nerve, and may cause symptoms associated with cervical radiculopathy or cervical myelopathy.
- Spinal stenosis may occur as a result of spondylosis (degenerative changes in the cervical spine) but can also be the result of traumatic (fractures and instability) and inflammatory conditions or caused by herniated discs or tumours.
- Cervical stenosis is most common in adults aged 50 or above, but can also affect younger people.
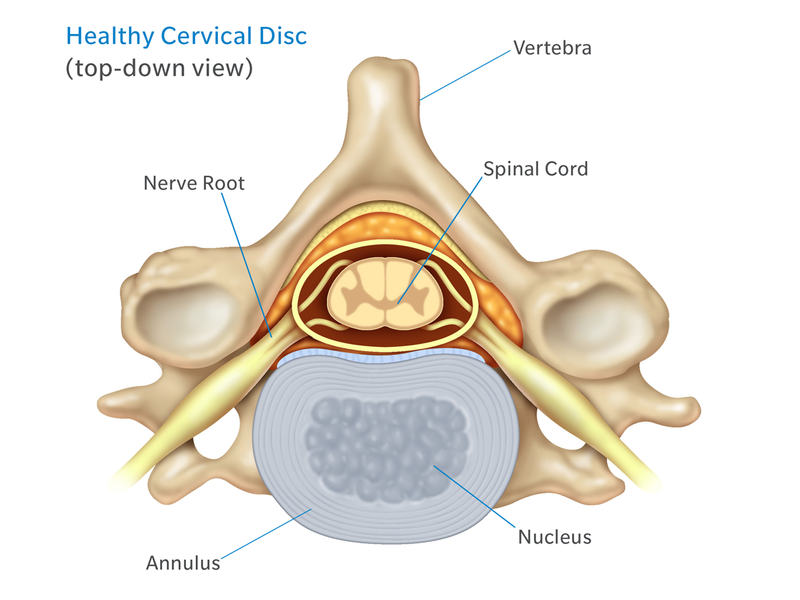
Anatomy Of The Cervical Spine :
- The cervical spine, is a complex structure of bones, nerves, muscles, ligaments, and tendons. The cervical spine is protect the spinal cord that passes messages from the brain to control all aspects of the body—while also remarkably strong and flexible, allowing the neck to move in all directions.
- The cervical spine also supports the weight of the head and allows a wide range of movement.
- There are 7 vertebrae in the cervical spine started from C1 through C7 top to bottom. Eight pairs of nerve roots, similarly starting from C1 through C8, branch off the spinal cord and exit the neck’s spinal column through the neural foramen (sometimes called neuroforamen).
- The top of the cervical spine vertebrae connects to the skull, and the bottom vertebrae connects to the upper back at about shoulder level. Side viewed of the cervical spine forms a lordotic curve by gently curving toward the front of the body and then back.
Types Of Cervical Stenosis
1. Foraminal Stenosis (Lateral Stenosis)
- The foramen between the intervertebral is the bony opening where spinal nerve roots exit – the spinal canal between two adjacent vertebrae. When one or more of these foramina spaces are reduced, it is called lateral spine canal stenosis (Foraminal).
- With foraminal canal stenosis, the spinal nerve has less space (compressed) and may become pinched, painful, and/or dysfunctional.
Other medical terms that might be used to more accurately identify the location of the spinal nerve compression include:
I. Lateral recess stenosis:
Lateral recess stenosis occurs when the spinal nerve is compressed just before it reaches the intervertebral foramen.
II. Far lateral stenosis:
- Far lateral stenosis occurs when the spinal nerve has already exited the intervertebral foramen.
2. Central Canal Stenosis
- The vertebral foramen is the bony opening in the center of the vertebra that protects the spinal cord as it runs down the spinal canal.
- When one or more of these vertebral foramina narrow, it is called central canal stenosis.
- With central canal stenosis, the spinal cord has less space and may become compressed, which can lead to pain and/or dysfunction experienced anywhere in the body below the level of compression.
What Are The Causes?
Cervical Spinal canal stenosis is typically caused by one or more of the following factors:
Spinal osteoarthritis:
- When the smooth cartilage covering the facet joints (which connect the backs of adjacent vertebrae) start to break down, bones begin to rub against each other and may lead to the formation of abnormal bone growth, its called osteophytes or bone spur.
- The resulting inflammation and osteophyte formation can cause to narrowing of the foramina.
Degenerative disc disease:
- When discs lose hydration and start to flatten (Degeneration of Disc), the intervertebral foramina also start to narrow.
- A disc bulge can also reduce the The vertebral foramen into the spinal canal.
- Disc degeneration disease can also put more pressure on the facet joints and accelerate their degeneration as well.
Ligament thickening or buckling:
- Injured Ligaments that supports vertebrae in the spinal canal can ossify (thicken and turn into bony tissue) and encroach upon the spinal cord or nearby spinal nerves.
- Gradually ligaments may also become more susceptible to buckling into the spinal canal as spinal degeneration progresses.
Other factors may also contribute to spinal canal stenosis, such as spinal deformity or cyst growths such as Kyphosis, Scoliosis.
Sign And Symptoms of Cervical stenosis
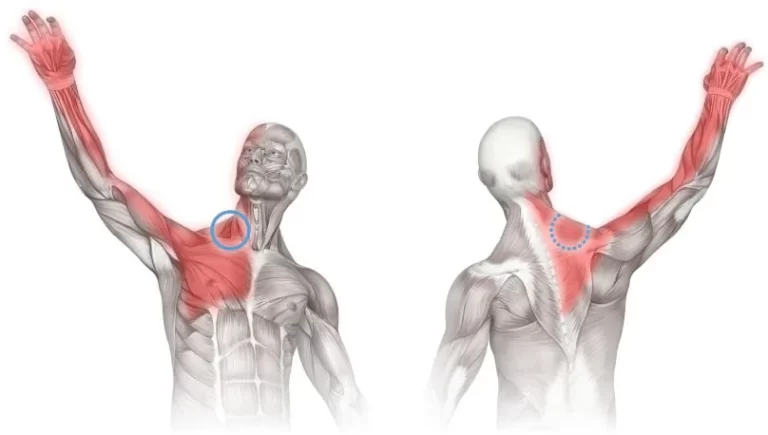
- Pain in the neck to shoulder or arms
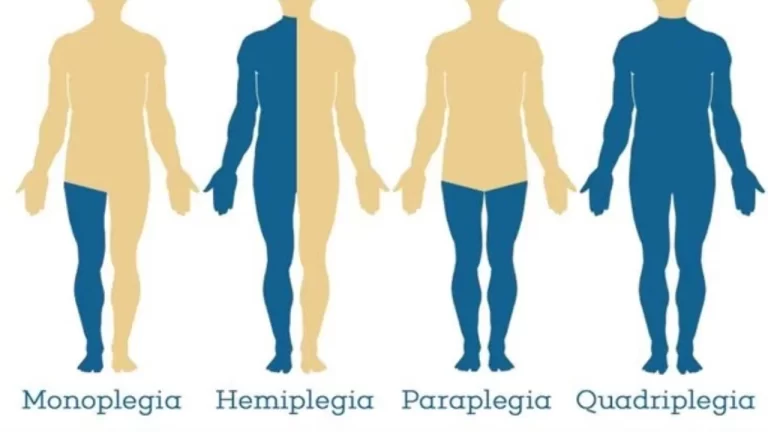
- Arm and leg dysfunction
- Weakness, stiffness or clumsiness in the hands
- Arm, Leg weakness
- Difficulty walking, stair climbing
- Frequent falling (Unbalancing)
- Urinary urgency which may progress to bladder and bowel incontinence
- Diminished proprioception
The progression of the symptoms may also vary in the following ways:
- A slow and steady decline
- Progression to a certain point and stabilizing
- Rapidly declining
Differential Diagnosis
- Diabetes
- Inflammatory spondyloarthropathy (e.g., ankylosing spondylitis)
- Paget’s disease of the bone
- Peripheral neuropathy (paralysis)
- Peripheral vascular disease
- Single level lumbar disc herniation
- Spinal cord tumor
- Vascular insufficiency (atherosclerosis of the aorta and/or leg arteries)
- Vertebral disc disease
- Kyphosis
- scoliosis
How To Diagnose?
Diagnosis of cervical stenosis is made by taking a patient history and performing a physical examination along with imaging studies such as computed tomography (CT) or magnetic resonance imaging (MRI). Treatment for cervical stenosis can vary depending on the severity of symptoms.
- Diagnosis can be made through imaging with extended release x-ray, CT, and MRI.
- With the availability of MRI, a plain radiograph is of limited value although dynamic views in flexion and extension modes can demonstrate dynamic instability or spondylolisthesis.
- CT can help differentiate calcified disks or bone osteophytes from “soft disks,” differentiate ossification of the posterior longitudinal ligament from a thickened posterior longitudinal ligament and detect bone fractures or lytic lesions.
- MRI is the gold standard, it is able to show intrinsic cord abnormalities, the degree of spinal stenosis, and differentiate other conditions such as tumors, hematoma, or infection.
- If a patient has a pacemaker and cannot obtain an MRI, a CT myelogram can be performed to identify the level and degree of stenosis.
Cervical stenosis Treatment :
Treatment of Cervical stenosis is mainly medical, surgical and Physiotherapy, Surgical treatment option is the last option if Medical and Physiotherapy treatment is not giving good results then your doctor’s advice is to go for surgery.
1. Medical ( Non-Operative) Treatment
- Initial treatment can include both conservative and non-surgical methods.
- These methods includes:
- Anti-inflammatory and analgesic medications such as NSAIDs.
- epidural steroid injections
- Physiotherapy treatment such as:
- stretching
- strengthening
- anaerobic fitness to improve and stabilize muscles
- posture correction
2. Cervical stenosis surgery :
- Surgery is for only those who fail repeated nonoperative treatments (aimed at improving symptoms and function rather than preventing neurologic complications) and only considered after attempting nonsurgical modalities, or if a patient’s symptoms result in disability.
- If a patient presents with rapidly progressive neurological deficits or if there is the presence of bladder dysfunction, urgent surgery is necessary such as cauda equina syndrome, conus medullaris syndrome, trauma, or an intraspinal canal tumor.
- The surgical approach is multilevel decompressive laminectomy with or without lumbar fusion.
- Lumbar fusion is generally reserved for patients with spondylolisthesis.
3. Physiotherapy Treatment
I. Treatment Without Surgery:
- Nonoperative treatments, such as physiotherapy treatment, are aimed at reducing pain and increasing the patient’s function.
- Physical therapy treatments helps the reducing pain, neck stiffness and also provide the patient of a long-lasting pain control and improved function without surgery.
- A Physio. rehabilitation program may require 1 or more months of supervised treatment session.
Ultrasound therapy, Interferential therapy (IFT), TENS, Intermittent Cervical traction (ICT) are common Physiotherapy programs that mostly selected by Physiotherapists.
Cervical stenosis exercises
Stretching exercises:
- These exercises are aimed at restoring the flexibility of the muscles of the neck, trunk, arms and legs.
Manual therapy:
- Cervical and thoracic joint manipulation to improve or maintain the range of motion.
Heat therapy:
- Heat Thearpy improves the blood circulation to the muscles and other soft tissues.
Cardiovascular exercises for arms and legs:
- This will improve blood circulation and enhance the patient’s cardiovascular endurance and promote good physical conditioning.
- Cardiovascular exercises includes free active movement exercise of the body such as aerobic exercises.


Aquatic exercises:
- Aquatic Exercises allow your body to exercise without pressure on the spine.
Ergonomics:
- Training of activity of daily living (ADL) and functional movements.
Exercises and techniques that may help relieve symptoms of spinal stenosis and prevent progression of the condition include:
- Specific strengthening exercises for the arm, trunk and leg muscles.
- Stretching
- Postural re-education
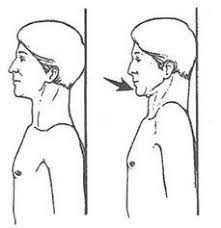
- Scapular stabilization
- Ergonomics and frequent changes of position, to avoid sustained postures that compress the spine
- Planning ahead so that you take breaks in between potentially back-stressing activities such as walking and yard work.
- Proper lifting, pushing, and pulling.
II. Post-Operative Treatment
Post-Operative physiotherapy is very necessary to restore muscle activities.
0-4 weeks:
- Posture education
- Cervical stabilization in supine
- Upper Extremity active range of movement as tolerated
- Cervical active range of movement as tolerated in pain-free range
- Gentle 2-finger isometrics
- Scapular retraction, shrugs, chin tucks
4-12 weeks:
- Upper Extremity theraband strengthening
- Scapular retraction strengthening
- Light weightupper extremity strengthening
- Cardiovascular exercises
- Ergonomics education
- TENS and ice for pain relief
12-24 weeks:
- Upper and extremity weight training
- Theraband PNF
- Push-up progression
- Work hardening
24+ weeks:
- Functional training
- Progressive weight training
- High impact aerobic activity
- May begin contact sports
Prognosis
- Cervical stenosis has significant morbidity and affects the quality of life.
- With time it can lead to chronic pain and muscle weakness.
- In some cases, it may lead to cauda equina syndrome.
- Patients with central spinal stenosis may have difficulty walking and have gait disturbances. While some patients may improve with time, the majority have a progression of the condition, leading to disability.
- The cost of managing cervical stenosis is enormous, and for patients can lead to high healthcare bills.





5 Comments