Understanding Chest Pain While Deep Breathing
Chest pain while breathing deeply may be due to various chest conditions, such as pleurisy, COVID-19, and pneumonia. The possible causes differ in severity and require different approaches to treatment.
- This pain typically intensifies with deep breaths, coughing, or sneezing and may be sharp, stabbing, or aching in nature.
- The pain is often associated with the pleura, the thin membrane lining the lungs and chest cavity.
- While some causes of chest pain with deep breathing are relatively benign, others may indicate more serious medical conditions such as pneumonia, pleurisy, or even cardiovascular issues.
Introduction
- Pneumonia: This respiratory illness can result in fever, coughing, dyspnea, and chest pain that gets worse when you take deep breaths.
- Pericarditis: An acute, stabbing pain that gets worse when you breathe deeply or lie down can be caused by inflammation of the sac that surrounds the heart.
- Wheezing, chest tightness, and shortness of breath are symptoms of asthma, a chronic respiratory disease that gets worse with deep breaths.
- Breathing heavily can cause chest pain, which can be an indication of several medical disorders such as pneumonia, pleurisy, or COVID-19. The possible causes differ in severity and necessitate distinct treatment approaches.
- Breathing shallowly may help ease the pain, which may worsen when you cough, sneeze, or move.
- Breathing heavily can cause chest pain, which can be an indication of several medical disorders such as pneumonia, pleurisy, or COVID-19. The possible causes differ in severity and necessitate distinct treatment approaches.
- Deep breathing-related chest pain can have a variety of causes. Not all causes of chest discomfort are dangerous.
- Chest pain can, however, occasionally indicate serious medical disorders like a heart attack that call for immediate care.
- Inflammation affecting the pleura is called pleurisy. The layer of tissue that divides the rib cage and the lungs is called the pleura.
- Pleurisy may result from a variety of conditions, including malignancy or infection.
Anatomy of Chest
- Several different chest tissues, such as the skin, ribs, intercostal muscles, pleura, esophagus, heart, aorta, diaphragm, or thoracic vertebrae, can cause pain.
- The sympathetic, vagus, phrenic, and intercostal nerves can all convey pain. Localizing the source of pain is challenging since the innervations of the deep tissues of the thorax share pathways with the central nervous system.
- A probabilistic approach to diagnosis will help in the decision-making process while attempting to determine the source of chest pain.
- The prevalence of coronary artery disease in various chest pain syndromes has been measured by several studies using coronary arteriography in patients referred for examination of recurrent chest pain.
- According to these investigations, anatomic coronary disease is present in 90% of patients with classic exertional angina. Compared to people with non-anginal pain, who have a 20–30% prevalence of coronary disease, patients with atypical angina have a 50–60% prevalence.
- However, care should be taken when interpreting these prevalence estimates. Women are less likely than men to have coronary disease, according to arteriography studies. Men with typical angina pectoris had a 93% prevalence of severe coronary disease in the Coronary
- Artery Surgery Study– while women with typical angina had a 72% prevalence. Moreover, the prevalence of age plays a significant role in the risk of coronary artery disease. Between the ages of 30 and 70, men’s risk of heart disease increases gradually; after that, it doesn’t increase much more.
- The risk increases more quickly for women between the ages of 60 and 80 after increasing gradually until then.
- According to arteryography studies, the prevalence of coronary disease is higher in patients evaluated at referral centers than in the general population. These individuals are carefully chosen for evaluation.
- Patients who fulfilled certain criteria for nonischemic chest pain were monitored to ascertain the underlying source of pain in research published by Sox et al. (1981). After being seen at a walk-in clinic, none of these patients showed any signs of ischemic heart disease.
- When analyzing a patient’s illness risk, try to determine the underlying frequencies of disease in their clinical contexts.
- The pericardium encloses the conical, hollow, muscular organ, the heart, located amid the mediastinum. It is located one-third to the right and two-thirds to the left of the midline, posterior to the sternum’s body.
- The heart weighs about 255 g for females and 310 g for males, with 12 x 8.5 x 6 cm measurements. It provides blood to various body areas so they can receive the nourishment they require. The Greek word “cardia,” which means “the heart,” is the source of the adjective “cardia.”
Relations
- The left lung, the pleura (apex), the sternum’s body, and the surrounding costal cartilage are located anteriorly.
- The esophagus, descending thoracic aorta, azygos, hemiazygos, and thoracic duct are located posteriorly.
On the surface
- the primary pulmonary trunk division
- Conversely: diaphragm
- Laterally: pleura, lungs
Heart’s layers
- The heart wall is composed of three layers that are surrounded by the pericardium.
- The visceral layer of the serous pericardium forms the epicardium, which is the outer layer of the heart wall.
- The heart’s middle layer of muscle, known as the myocardium, contains both the conducting system and excitable tissue.
- the endocardium
- A layer of the concentric middle
- A layer beneath the heart.
- The subepicardial and subendocardial layers make up the majority of the remaining cardiac tissue.
Causes of Chest Pain While Deep Breathing
Chronic chest pain
- When a patient presents with persistent chest pain, coronary artery disease is the first diagnostic factor to be considered. Recurrent angina pectoris is the most typical clinical manifestation of coronary artery disease.
- One useful characteristic of coronary artery disease that aids in diagnosis is that certain drugs typically alleviate the pain. If anginal pain is relieved three minutes after taking sublingual nitroglycerin, coronary disease is most likely the origin of the pain.
- When beta blockers, calcium channel blockers, or long-acting nitrate preparations are started, the frequency of attacks decreases, indicating that coronary artery disease is the cause.
- Chest pain that comes back frequently is caused by esophageal illness. Esophagitis, which often results from stomach acid reflux, is a common cause of esophageal pain.
- The acid damages the mucosa chemically and inflames it, causing discomfort that tends to burn. Acid-peptic disease in the past and reflux symptoms like regurgitation or an acidic taste in the mouth are indicators of reflux esophagitis.
- Esophageal reflux disease (GERD)-associated chest pain typically flares up after meals and may be related to posture
- It is possible to set off pain episodes by bending forward at the waist. Because the recumbent position increases the amount of acid reflux into the esophagus, they frequently happen at night.
- This diagnosis is suggested by pain relief from antacids, topical lidocaine, or particular reflux-reducing techniques.
- Chest pain is frequently caused by problems related to the esophagus. While motor diseases cause pain by contracting and spasming the muscles that line the esophageal wall, reflux esophagitis causes discomfort by irritating the mucosa of the esophagus.
- Esophageal spasm is frequently reflux esophagitis’ subsequent symptom. When mucosal irritation and inflammation worsen, local nerve stimulation triggers muscle spasms.
- These patients will describe a pattern of pain that occurs after meals and is made worse by body posture, much like reflux esophagitis. Different types of pain may be reported by patients.
- Simple mucosal irritation episodes are characterized by pain that is described as “heartburn,” whereas muscular spasm episodes are characterized by a more intense, heavy-feeling discomfort. dysphagia-related motor disorders also occur in people without acid reflux illness, such as those who have diffuse esophageal spasms or achalasia.
- The pattern of episodes in these patients differs from that of acid reflux sufferers. Usually unrelated to body posture, the pain can happen during eating rather than after a meal. One of the most common symptoms in people with primary motor disorders is dysphagia.
- Calcium channel blockers and nitrates can alleviate esophageal motor problems by relaxing the smooth muscular wall of the esophagus.
- The clinician may encounter challenges when attempting to utilize drug response as a marker for undetected chest pain because these medications also alleviate the pain in the chest associated with coronary artery disease.
- The findings of a therapy trial, especially the speed of response, must be carefully interpreted by the doctor. When nitroglycerin is taken sublingually and pain subsides after three minutes, coronary artery disease is more likely to be the cause than esophageal motor problems.
- It is more likely that you have esophageal disease if relief only appears after 10 to 15 minutes. Lower esophageal sphincter relaxation and esophageal reflux aggravation can be caused by nitrates and calcium channel blockers, which can worsen the symptoms of esophagitis from reflux.
- Recurrent chest discomfort can be the result of myocardial ischemia, which can occasionally happen when there are no permanent blockages in the coronary arteries. Ischemia may result from intramural small vessel occlusion.
- Although small vessel disease is a rare cause of chest pain, such lesions are more common in diabetics. It ought to be taken into account only after more plausible etiologies have been ruled out. Myocardial ischemia can also be brought on by thyrotoxicosis, hypertrophic cardiomyopathy, and valvular aortic stenosis.
- These disorders typically cause discomfort that is comparable in quality and pattern to coronary artery disease. These entities are typically easy to detect since they are almost always accompanied by physical examination findings typical of the underlying disease.
- In the absence of obstructive coronary disease, myocardial ischemia can be caused by coronary vasospasm. Although the pain typically follows an erratic pattern, it often has characteristics with the discomfort experienced in obstructive coronary disease.
- The patient may awaken from sleep due to pain that is usually not brought on by exercise. Emotional stress is cited by some patients as a trigger.
- Sublingual nitroglycerin often alleviates the discomfort, while long-acting nitrates or calcium channel blockers reduce the frequency of attacks.
- Ninety percent of patients suffering from coronary vasospasm experience alterations in their ECG when experiencing discomfort. Therefore, coronary vasospasm is improbable if electrocardiographic alterations do not occur during pain.
- The cause of prolonged chest pain is controversially linked to mitral valve prolapse (MVP). Studies using echocardiography and clinical settings have shown that MVP is frequently observed in otherwise healthy persons.
- According to population research, the incidence of chest pain is not greater in people with mitral valve prolapse than in people without the condition. However, there are many clinical reports of people for whom persistent chest pain could only be identified as the result of mitral valve prolapse.
- There is no “typical” MVP chest pain syndrome; instead, the individuals in these trials experience a variety of pain characteristics and patterns.
- Since there is no known cure for the condition, it should only be ruled out as a cause of recurrent chest pain after other plausible explanations have been exhausted disorder.
- The primary purpose of identifying mitral valve prolapse is to identify patients who may have arrhythmias and endocarditis.
- According to prospective research, patients who experience severe problems also have an irregular ECG or a late systolic murmur in addition to the mid-systolic click.
- Echocardiography is therefore not required to rule out mitral valve prolapse unless a patient presents with physical examination and/or ECG results that indicate a risk of consequences.
- Recurrent chest discomfort may be caused by the chest wall, yet there is currently a lack of clarity about the clinical diagnosis of chest wall disorders.
- Chest wall pain can vary widely in its location and quality; diagnosing it can be aided by knowing what caused it.
- Often pleuritic, chest wall pain is made worse by moving the arms. or upper body. Palpation or manipulation of the chest wall can generate discomfort in the majority of individual
Causes of acute chest pain
- When a patient experiences a new episode of chest pain or a rise in the frequency or intensity of recurring chest pain, the doctor must act quickly to manage the patient.
- The decision of whether to admit the patient must be made because some of the illnesses are potentially fatal.
- Assessing the patient’s reaction to therapeutic interventions is frequently not a possibility. An organized approach to management is necessary.
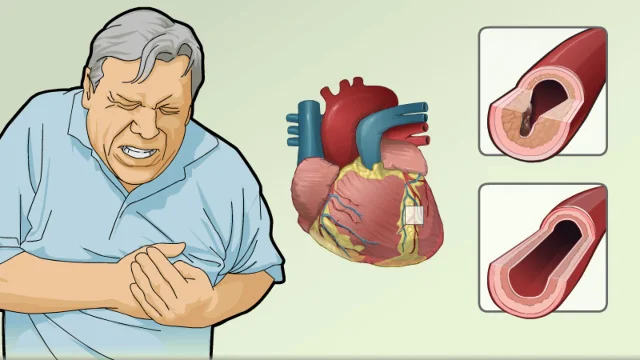
- Myocardial infarction is the most common diagnosis for acute chest discomfort. This potentially fatal ailment needs to be treated right away.
- Angina pectoris and myocardial infarction: Pain are similar in nature and location, but myocardial infarction pain is typically more severe, prolonged, and intense.
- The discomfort doesn’t go away with nitroglycerin and usually happens while at rest. It could be accompanied by dyspnea, diaphoresis, or uneasiness.
- A patient does not always have an infarction if there are no new Q waves or ST segment elevations on the A wide range of patients experiencing chest discomfort as a result of coronary artery disease fall under the umbrella of unstable angina pectoris syndrome.
- It has been demonstrated that treatment measures can lower the short-term risk of myocardial infarction in patients with unstable angina. Patients with angina pectoris with recent onset are included in the syndrome.
- For these people, relaxation or sublingual nitroglycerin relieves exertional discomfort. Patients with steady exertional pain but a fluctuating pain pattern are also included in this syndrome.
- These individuals report feeling pain when they are at rest or lesser level of exercise. It’s possible that nitroglycerin won’t help anymore.
- A variety of pathophysiologic processes could be in charge of unstable angina. The most frequent process is the atherosclerotic disease’s increasing severity.
- Unstable angina can also be brought on by vasospasm exacerbating atherosclerotic disease. pectoris.
- Medication changes are a major contributor to unstable angina in persons who have previously experienced stable angina.
- The patient may not follow the regimen as directed by the doctor, or the patient may misunderstand it. Sometimes nitroglycerin becomes antiquated and inefficient. Clues can be found by closely examining the patient’s prescription regimen.
- Acute chest pain can have a serious and potentially fatal cause: Dissection of the thoracic aorta. Early exclusion of dissection is necessary by the clinician since it necessitates particular, rapid treatment.
- The clinical manifestations of the two main forms of dissection differ. Though they can occasionally spread outside of the aortic arch, proximal dissections begin in the ascending aorta.
- About half of patients with proximal dissection report radiation to the posterior chest, while almost all experience anterior chest pain. Roughly two-thirds exhibit signs of prior hypertension.
- Consideration of this diagnosis should be given careful consideration of the physical examination since the majority have neurologic abnormalities, aortic regurgitation murmur, or pulse deficiencies.
Symptoms related to Chest Pain While Deep Breathing
- Heart disease is frequently linked to chest pain. However, a lot of heart disease sufferers report having a slight discomfort that they wouldn’t truly classify as pain.
- A heart attack or other cardiac condition may cause chest discomfort that feels like:
- Chest tightness or a searing sensation of pressure.
- severing or crushing pain that radiates to the shoulders, neck, jaw, back, and one or both arms.
- Pain that lasts more than a few minutes, intensifies with movement, disappears and reappears, or fluctuates in intensity.
- Breathing difficulty.
- Cold sweats.
- Weakness, dizziness, or lightheadedness.
- Heartbeats that race.
- Vomiting or nausea.
- A bitter flavor or the impression that food is returning
- To difficulty swallowing
- Pain that changes in intensity or quality with a change in posture
- Soreness that worsens with deep breathing or coughing
- Sensitivity to pressure on the chest
- The anguish that lasts for several hours
Diagnosis
- Not every ache in the chest indicates a heart attack. However, emergency department doctors usually screen for it first since it can be the most urgent risk to your life.
- They might also search for possibly fatal lung conditions like lung collapse or lung blood clots.
Immediate tests
- Cardiogram (also known as ECG or EKG): This brief examination gauges the heart’s electrical activity. Sticky patches called electrodes are put to the arms, legs, and sometimes the chest.
- The electrodes and a computer are connected by wires, and the computer prints or displays the test findings ECG may show if the heart is beating too rapidly or too slowly. An ECG may show if the heart is beating too rapidly or too slowly
- Blood examinations: Following cardiac damage following a heart attack, some heart proteins gradually seep into the circulation. Blood tests can be used to identify these proteins.
- Chest radiography: The size, shape, and health of the heart, major blood vessels, and lungs can all be seen on a chest X-ray.
- An A chest X-ray might also show lung issues including pneumonia or lung collapse.
- CT scan (computerized tomography): CT scans can identify an aortic dissection or a blood clot in the lung.
Follow-up testing
- Echocardiography: Videos of the beating heart are produced by using sound waves. To obtain better images of the heart, a more thorough echocardiography may occasionally be performed.
- To get a better look at various cardiac regions, a tiny gadget may be inserted down the throat.
- Stress assessments: These examinations frequently entail stationary cycling or treadmill walking while the heart rhythm is monitored.
- Exercise-induced cardiac responses are demonstrated by exercise tests. If you are unable to exercise, you may be prescribed medications that have similar heart-related effects.
- catheterization of the heart: This test aids medical professionals in identifying cardiac artery blockages. Usually in the groin or wrist, a long, thin, flexible tube is placed into a blood vessel. That led straight to the heart.
- The tube allows the dye to enter the heart’s arteries. The dye makes the arteries more visible in films and X-rays.
Treatment of Chest Pain while Breathing Deeply
Treatment for chest pain differs based on the underlying cause of the discomfort.
Medications
- Relaxants for the Arteries: Usually administered as a tablet under the tongue, nitroglycerin relaxes the cardiac arteries to facilitate easier blood flow through the constricted areas.
- Certain medications for high blood pressure can relax and dilate blood arteries.
- Aspirin: You’ll probably be prescribed aspirin if medical professionals believe that your chest pain is caused by a heart condition.
- Thrombolytics are another name for clot-busting medications: You might be given these medications if you are experiencing a heart attack.
- These function to break up the clot preventing blood flow to the heart muscle.
- Thinners of Blood: In the case that a clot develops in an artery leading to your heart or lungs, you will probably be prescribed medication to stop further clot formation.
- medications that lower acid.
- If stomach acid spilling into the chest is the source of the pain, the esophagus, a healthcare provider may suggest these medicines.
- They lessen the stomach’s acid production.
- Drugs that Fight Depression: Your doctor may recommend antidepressants if you get panic attacks to assist in managing your symptoms. It may also be advised to seek talk treatment, such as cognitive behavioral therapy
Surgical and other procedures
- Angioplasty and stent placement: This procedure aids in clearing a blockage in a heart-related artery. A narrow tube with a balloon on the end is inserted by the medical professional into a big blood vessel, typically in the groin.
- The tube is guided to the obstruction by the provider. The balloon becomes bigger. This makes the artery wider. Along with the tube, the balloon is deflated and taken out.
- To keep the artery open, a tiny wire mesh tube known as a stent is frequently inserted.
- Coronary artery bypass surgery: Through this kind of open cardiac surgery, a blockage in the heart is circumvented by creating a new blood vessel. The new channel is created by the surgeon using a blood artery from another area of the body.
- Emergency repair surgery: An aortic dissection, commonly known as an aortic rupture, may require immediate cardiac surgery. It’s a potentially fatal illness.
- Lung reinflation: A healthcare professional may place a tube in your chest to inflate a compressed lung.
Physiotherapy Treatment
Gentle range of movement exercises
- It’s critical to begin slowly moving as soon as comfort permits after chest wall damage. It can take up to 8–12 weeks for even a damaged rib to recover completely, therefore you must increase your general exercise gradually during this time.
- After a physiotherapy evaluation, you will receive instructions on particular activities that can help you heal.
- Your thoracic spine and chest muscles may become imbalanced due to fear of movement and defensive postures; this can result in discomfort that lasts longer than the healing time of the injury.
- Thus, it is advised to mobilize as soon as possible to increase spinal mobility and avoid chronic pain.
Breathing exercises
- It’s critical to prevent chest infections and other rib damage problems. A spirometer, a device that monitors the volume of air you breathe in and out, may be used in conjunction with physical therapy breathing exercises.
- This will help you get a better sense of what it should feel like to inhale deeply and fully. To facilitate deeper breathing and a productive cough—both of which are necessary to help you expel any phlegm from your chest—we frequently employ a method known as The Active Cycle of Breathing.
Active Cycle of Breathing Technique (ACBT)
- The ACBT method can assist in releasing certain areas from your chest. Occasionally, weariness and pain can reduce how hard you cough.
- To help you more easily evacuate the secretions from your lungs and into your main airway, the trachea, the ACBT uses several breathing techniques.
- ACBT is divided into four parts:
- Breathing with ease and control
- This is a typical, leisurely breath. Feel the rise and fall of your abdomen with one hand.
- inhaling deeply
- Inhale deeply and feel your lower chest open up as much as it can. Strive to maintain a relaxed neck and shoulders. Breathe in for up to three seconds, then gradually exhale.
- Sigh
- A quick, sharp breath is released through an open mouth to expel the fluids with power. Consider heating a mirror with steam.
- Cough
- Cough only when you believe the secretions are ready to be gone.
- Breathing exercises are beneficial for several health-related reasons. For example, to strengthen the respiratory muscles, improve ventilation, improve breathing efficiency, and relieve tension and anxiety.
Diaphragmatic Breathing
- As the diaphragm is responsible for 80% of breathing, diaphragmatic breathing is a sort of breathing exercise that helps develop this important breathing muscle.
- People who practice diaphragmatic breathing can feel more at ease and rested.
- Another name for this breathing technique is abdominal or belly breathing.
- Method:
- Place the patient in a position that benefits from gravity, such as a semi-Fowler’s position.
- Put one hand on your chest and the other on your stomach while concentrating on your diaphragm. Breathe deeply and slowly, observing how your hand moves. When breathing diaphragmatically, the stomach hand should move the most
- Breathe slowly: Inhale deeply to fill your lungs, then release the air gradually. Controlling the exhalation rate can be achieved by exhaling via the nose. Exhale, pause for a moment, then inhale once more.
Pursed- lip Breathing
- Pursed-lip breathing is a breathing method in which the mouth is closed while expelling via firmly pressed lips and inhaling through the nose.
- It is a useful technique for lengthening the exhaling duration so that more air may be evacuated with each breath cycle.
- People with obstructive lung illnesses, such as asthma which causes dyspnea during exertion, and chronic obstructive pulmonary disease (COPD), have been reported to benefit from this method.
Summary
- Breathing deeply might cause pain in the chest due to many reasons.
- These comprise inflammatory diseases such as pneumonia, pericarditis, and pleurisy. The same is true for COVID-19, COPD, and pulmonary embolism.
- Breathing deeply can potentially induce chest pain related to lung cancer.
- Additionally, chest pain may be a sign of a medical emergency, such as a heart attack.
- The underlying reason for chest pain determines how to treat it.
- A person should consult a physician if they experience any concerns regarding chest pain while deep breathing.
FAQ
Why does breathing cause a stabbing ache in my chest?
pericarditis, which typically manifests as an abrupt, intense, stabbing pain that worsens with deep breathing or lying down.
How come breathing feels so tight in my chest?
There are numerous causes for the tightness in your chest. Even though the pain or discomfort may be unsettling, a cardiac emergency is not usually the reason for the constriction. Alternatively, asthma, acid reflux, anxiety, or muscle strain could be the cause of your tightness.
Is it possible for gas to induce chest pain?
Although it can occasionally happen in the chest, gas discomfort is typically felt in the abdomen. Even while gas is uncomfortable, when it occurs on its own, it usually doesn’t warrant any concern.
What distinguishes gas from pain in the chest?
While gas-related chest pain is frequently transient and can be controlled with lifestyle changes or the right medical care, cardiac-related chest pain necessitates immediate medical attention. Always get immediate medical attention if you are having problems with your chest pain.
Reference
- Anatomy of the Human Heart. (n.d.). Physiopedia. https://www.physio-pedia.com/Anatomy_of_the_Human_Heart
- Hickam, D. H. (1990). Chest Pain or Discomfort. Clinical Methods – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK416/
- Rees, M. (2023, May 16). What causes chest pain when breathing deeply? https://www.medicalnewstoday.com/articles/chest-pain-when-breathing-deeply#summary
- Rib Injury Clinic. (n.d.). https://www.ribinjuryclinic.com/treatments/physical-therapy-rehabilitation/
- Breathing Exercises. (n.d.). Physiopedia. https://www.physio-pedia.com/Breathing_Exercises




2 Comments