Syndesmotic Ankle Injury and Physiotherapy Management
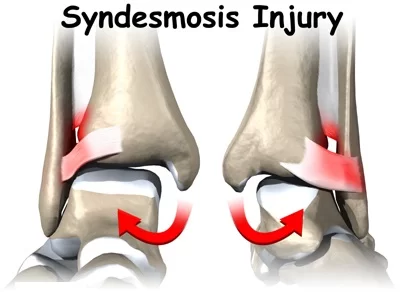
- A Syndesmotic ankle sprain is an injury of syndesmosis of the ankle. a syndesmosis is a fibrous joint between two bones linked by ligaments and a strong membrane.
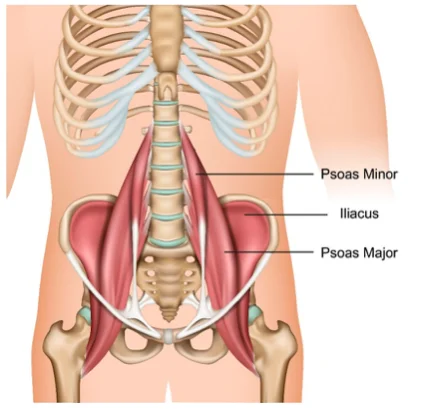
- The distal tibiofibular syndesmosis is a syndesmotic joint. It is formed between the distal tibia and fibula and it is attached by the interosseous ligament (IOL).
- the anterior-inferior tibiofibular ligament (AITFL), the posterior-inferior tibiofibular ligament (PITFL), and the transverse tibiofibular ligament (TTFL).
Anatomy-related syndesmotic ankle sprain
Articulating Surfaces:
- Distal fibula (rough medial convex surface)
- Distal tibia (the triangular notch of the lateral surface)
- This forms a mortise for the trochlea of the Talus
INTEROSSEUS MEMBRANE:
- Function:
- The inferior segment assists in stabilizing the tibiofibular syndesmosis. There exists controversy in the literature if the TTFL and the PITFL are two components of one anatomical structure or two different structures.
SYNDESMOSIS LIGAMENT
- Function
- The function of the syndesmosis ligament complex:
- Provide strong stabilization and dynamic support to the ankle mortise
- Maintain the integrity between the distal tibia and fibula
- Resist forces (axial, rotational, and translational) that attempt to separate the two bones
- Motions Available
- 2° fibula external rotation relative to the tibia
- As the ankle joint moves from end-range plantarflexion to end-range dorsiflexion the ankle mortise widens only about 1mm.
- Pathology/Injury
- Injury to the syndesmotic joint is described in the literature as an injury to the syndesmotic ligaments.
Clinical conditions:
- High ankle sprain or syndesmotic ankle sprain (syndesmosis injury)
- AITFL injury is normally combined with a tear of the IOL.
- Tibiofibular Diastasis
- Ankle fracture
- Syndesmotic Impingement (anterolateral soft tissue impingement)
- A fatty synovial fringe (small bundle of adipose tissue) moves during ankle movement.
- It rises during dorsiflexion and thus retracts between the tibia and the fibula and descends during plantarflexion thus lowering towards the ankle joint.
- May cause chronic pain after an ankle sprain.
ANKLE SYNDESMOSIS INJURY
- DescriptionA syndesmotic, or ‘high’ ankle sprain is one that involves the ligaments binding the distal tibia and fibula at the Distal Tibiofibular Syndesmosis.
- Injuries can occur with any ankle motion, but the most common motions are extreme external rotation or dorsiflexion of the Talus.
- The dome of the Talus is wider in the anterior than in the posterior, and these movements force apart the medial and lateral aspects of the mortise, respectively the tibial and fibular malleoli.
- Sufficient distraction of the distal fibula from the tibia can cause strain or rupture of one or more of the following ligaments: the anterior inferior tibiofibular ligament, superficial posterior inferior tibiofibular ligament, transverse tibiofibular ligament, interosseous membrane, interosseous ligament, and the inferior transverse ligament.
- Rupture injuries also commonly present with concomitant fractures of either malleolus (lateral being more common) or proximal fibular spiral fracture is known as a Maisonneuve fracture.
Etiology of syndesmotic ankle sprain
- Syndesmotic ankle sprains commonly occur to athletes participating in American football and downhill skiing.
- Football injuries are usually a result of forced external rotation of the foot while the athlete is prone, as in at the bottom of the pile.
- The injuries can also result from a blow to the lateral knee while the foot is planted and dorsiflexed, resulting in an eversion or external rotation moment at the talocrural joint.
- In downhill ski racing, the boot does not allow dorsi- or plantar-flexion movement, which can result in excessive allowance of talocrural external rotation and injury to the anterior or posterior tibiofibular ligament, as well as the interosseous membrane.
Clinical Presentation of syndesmotic ankle sprain
- Observationally the Syndesmotic will show significantly less swelling than a lateral ankle sprain, as well as demonstrate a loss of full plantar flexion and an inability to bear weight.
- Ecchymosis may appear several days post-injury due to the injury of the interosseous membrane.
- Difficulty or inability to toe walk is often noted. History includes chronic pain, prolonged recovery, recurrent sprains, and the formation of heterotopic ossification within the interosseous membrane.
- The most common MOI is when the foot is in external rotation with excessive dorsiflexion.
Examination
Observation
- Gait analysis
- Palpation:
- Tenderness proximally over the anterior tibiofibular ligament and proximal along the interosseous membrane
- Palpate the medial and lateral malleoli for the existence of a fracture
- Fibula needs to be palpated from distal to proximal, including the proximal tibiofibular joint to rule out Maissoneuve’s fracture.
- Distal Pulses: Ensure pedal pulses are present
- Girth Measurements: Notable swelling of the ankle: do Figure 8 girth measurements
Special Testing
- Dorsiflexion External Rotation Stress Test (Kleiger’s Test)
- Determines rotator damage to the deltoid ligament or the distal tibiofibular syndesmosis.
- Performed by having the knee flexed by 90 degrees with the ankle in a neutral position and applying an external rotational force to the affected foot and ankle.
- (+) test: Pain in the anterolateral ankle. An indicator of deltoid ligament damage would be if there is a displacement of the talus away from the medial malleolus.
2. Squeeze Test
- Separation of the tibia and fibula
- Identifies a fibular fracture or syndesmosis sprain.
- Performed by squeezing the tibia and fibula together above the injury.
- (+) test: Pain will be reproduced along the fibular shaft if it’s a fibular fracture and the distal tibiofibular jt for syndesmosis sprain.
3. Cotton Test
- Assess for syndesmosis instability with diastasis.
- Performed: steadying the distal leg with one hand while grasping the plantar heel with the opposite hand and moving the heel directly from side to side
- (+) test: Any lateral translation would indicate syndesmotic instability
Physiotherapy management of syndesmotic ankle sprain
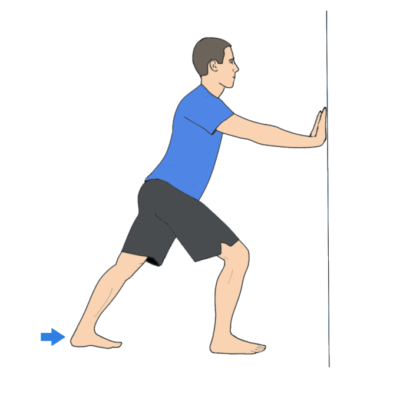
1.) Calf Stretch with Step
2.) Calf Strengthening Exercise
3.) Lunging Calf Stretch
Goals:
First two weeks:
- ROM, decrease pain and swelling, protect ligaments against further injury
- Week 3 and onward: Restore normal ROM, strengthen ligaments and supporting muscles, training to improve endurance and balance
- The most important long-term goal is to prevent re-injury!
- Patient Education
Weight-bearing protocol
- Caution against vigorous physical activity until full weight-bearing and dynamic balance has normalized.
- Gait training with crutches or boot/brace
- Fall risk
- Assistive Devices: Crutches must be maintained until a normal, pain-free gait is obtained
- Walking boot or stirrup brace for unstable injuries.
Modalities:
- RICE (rest, ice, compression, elevation) initially for 15 min 3x a day(. However, Bleakley et al suggested that there is little evidence to support the use of RICE, although it is a widely accepted treatment
- Non-steroidal anti-inflammatory drugs and comfrey ointment have been shown to improve short-term recovery following an acute ankle sprain.
Therapeutic Exercise/ Neuromuscular Re-education:
- First two weeks: AROM flexion, ankle alphabet, dorsiflexion/plantarflexion and inversion/eversion with theraband
- Weeks 3-4: Standing Stretch, seated dorsiflexion stretch with theraband, double heel raise progressing to single heel raise, and dorsiflexion stretching on a step stool
- Progressive weight-bearing and treadmill gait training to promote normal gait patterns.
- Neuromuscular Re-education: ankle proprioception, postural reflexes, and balance
- Ex: Single-leg stance, disk or balance pad training, aquatic therapy
- Progress to jogging, cycling, agility, jumping, and sport-specific drills.
- Modify exercises to avoid hyperdorsiflexion (stresses mortise joint), subtalar eversion, and loaded external rotation.
Manual Therapy:
- Passive accessory movement of the talocrural and subtalar joints and passive stretching may help stiffness. (Level of evidence 3A)
- Green et al: those subjects who used RICE with manual therapy were more likely to reach this normal ROM within the first 2 weeks of the ankle sprain than those who received RICE alone.
- Collins et al: Subjects showed immediate ROM gains when Mulligan’s movement with mobilization was applied in the sub-acute sprains and in patients with recurrent sprains.
- Landrum et al: Reported that one 30-second A-P talocrural joint mob immediately increased ankle dorsiflexion ROM after prolonged mobilization.




4 Comments