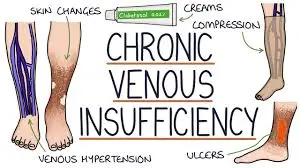
Chronic Venous Insufficiency
What is a Chronic Venous Insufficiency?
When blood cannot return to your heart from your leg veins, you have chronic venous insufficiency. Your veins’ valves normally ensure that blood travels in the direction of your heart.
Blood can, however, also flow in the opposite direction when these valves malfunction. Your legs may begin to pool blood as a result of this.
Overview
Damage to the veins in your legs might result in venous disease known as chronic venous insufficiency (CVI). This makes it more difficult for blood in your legs to return to your heart since these veins are unable to regulate blood flow as well as they should. Blood pools in the veins in your legs as a result of CVI, which raises the vein pressure there.
CVI can occur as a result of injury to any of your leg veins. one of them:
- Deep veins are huge veins that flow through your muscles deep within your body.
- Superficial veins are those that are near the surface of your skin.
- Deep and superficial veins are linked by perforating veins.
- CVI may initially give modest symptoms. However, this issue can have an impact on your quality of life and lead to major complications over time.
Post-thrombotic syndrome versus chronic venous insufficiency
Both names make reference to the same issue, which is damaged leg veins. Deep vein thrombosis (DVT) causes chronic venous insufficiency, resulting in post-thrombotic syndrome. A deep vein thrombosis (DVT) is a blood clot in a deep vein in your leg. “Post-thrombotic” refers to what happens following a blood clot (also known as a “thrombus”). When a blood clot disappears, it may leave scar tissue that affects the vein.
Post-thrombotic syndrome affects 20% to 50% of persons who have had DVT, usually within one to two years.
What is the prevalence of chronic venous insufficiency?
Venous illness is fairly common in general. Varicose veins, for example, suffer from around one in every three adults. Every year, approximately one in every fifty persons with varicose veins develops chronic venous insufficiency.
People over the age of 50 are more likely to suffer from chronic venous insufficiency. The danger increases as you become older.
About one in every twenty persons suffers from chronic venous insufficiency.
If you do not treat this condition, you may develop:
- Pain, Swelling, and Cramps
- Skin modifications
- Varicose veins
- Ulcers on the legs
Chronic venous insufficiency can cause pain and disability, but it isn’t typically a serious health concern.
Symptoms of chronic venous insufficiency
Symptoms of chronic venous insufficiency. Skin changes, discomfort, and swelling in your legs and feet are examples.
Chronic venous insufficiency produces several symptoms in your legs and feet. As your illness advances, your symptoms may worsen or you may discover new ones.
Signs and symptoms of chronic venous insufficiency include:
- Legs that are achy or weary.
- Leg tingling, burning, or “pins and needles” sensation.
- Nighttime cramping in your legs.
- Skin that is discolored and appears reddish-brown.
- Edema (swelling) in your lower legs and ankles, particularly after prolonged standing or at the end of the day.
- Itching or flaky skin on your legs or feet.
- Your legs may feel full or heavy.
- Your legs have leathery skin.
- Ulcers (open sores), mainly around the ankles.
- This scar tissue causes fluid to accumulate in your tissues. Your calf may appear huge and firm to the touch. When this happens, your skin becomes more prone to recurrent ulcers.
You may not be concerned about all of these issues at the same time. Perhaps you only have one or two. The severity of your signs and symptoms is determined by the stage of your condition.
What are the stages of chronic venous insufficiency?
Venous diseases are classified into six stages. “Venous disorders” is a broad term describing a variety of vein-related illnesses, including CVI. Clinical signs, which your provider can see or feel when they examine your legs, are used to categorize the stages.
Classification
Acute venous ulcer measuring 45 x 30 mm.
Clinical, Etiological (causal), Anatomical, and Pathophysiological variables are used to classify CEAP. The Widmer Classification for Assessment of Chronic Venous Insufficiency (CVI) distinguishes chronic venous insufficiency from varicose veins. It was created to aid in the assessment and management of chronic venous insufficiency.
CVI is classified as follows by CEAP:
Clinical stages
- C0: no apparent venous illness characteristic
- C1: The presence of reticular or spider veins.
- C2: Visible varicose veins
- C3: Edema present but no skin changes
- C4: discolouration and pigmentation of the skin
- C5: A healed ulcer C6: An acute ulcer
Etiological stages
- Primary
- Secondary (trauma, birth control pill)
- Congenital (Klipper trenaunay)
- No cause is known
Anatomical stages
- Superficial
- Deep
- Perforator
- No obvious anatomic location
Pathophysiological stages
- Obstruction, thrombosis
- Reflux
- Obstruction and reflux
- No venous pathology
- If you are at stage 3 or higher, you have chronic venous insufficiency. In other words, having varicose veins does not automatically imply having CVI.
- However, varicose veins are a sign of blood flow issues that could worsen with time. As a result, it’s critical to notify your physician if you see any new varicose veins.
What is the root cause of chronic venous insufficiency?
Chronic venous insufficiency happens when the valves in the leg veins fail to function properly. The valves in your leg veins assist your blood flow in the right direction (toward your heart). When a valve is damaged, it is unable to close properly. Gravity takes over, and blood tries to rise to your heart. Instead, it flows backward, a condition known as venous reflux.
Tests and Diagnosis
A physical exam and ultrasound imaging are used to diagnose chronic venous insufficiency. Your provider will do the following during the physical exam:
Examine your legs thoroughly-Your clinician will examine your skin for clinical indicators of CVI, such as ulcers or changes in skin color.
Conduct a vascular ultrasound-This painless examination creates an image of your veins using sound waves. It identifies which areas of your veins are affected.
Other medical disorders that could be causing your symptoms will also be ruled out by your provider. Other tests, such as an MRI, might be necessary.
Many CVI patients also have peripheral artery disease (PAD). As a result, your provider may ask you questions or do tests to screen you for PAD. If you have both CVI and PAD, your provider will advise you on compression therapy treatment approaches and measures to follow.
Treatment of chronic venous insufficiency
In relieving pressure in your leg veins. Your provider may advise you to do this for at least 30 minutes three times per day.
Walking and other forms of exercise can improve blood flow in your leg veins. When you take a walk, your calf muscle contracts, assisting your veins in returning blood to your heart.
Weight control:
Excess weight can put a strain on your veins and damage the valves. Consult your doctor to determine what constitutes a healthy weight for you. Develop a healthy and achievable weight-loss strategy with your provider
Compression treatment
Compression therapy is frequently recommended by providers for the treatment of CVI. Compression therapy reduces edema and pain in your legs.
Compression bandages and stockings come in a variety of styles. Some provide greater compression than others. Tight stockings necessitate a prescription.
- Some stockings are “graduated,” which means they are tighter at your ankles and looser further up your leg. It is critical that you follow your provider’s recommendations for the type of compression you require and when to apply it.
- Many patients with CVI find it difficult to wear compression stockings for an extended period.
- However, compression therapy is critical for improving vein function and alleviating discomfort.
- Talk to your provider if you’re having trouble with compression therapy.
- You might require a different style of stocking. Alternatively, your provider may offer suggestions to make the treatment plan more manageable for you.
- If stockings are ineffective, your clinician may recommend intermittent pneumatic compression (IPC). IPC devices are inflatable sleeves worn on the legs that aid with blood flow via the veins.
- Compression therapy should be used with caution by people who have peripheral artery disease (PAD).
- Depending on the severity of your PAD, your provider may advise you not to use it at all. Follow your provider’s instructions exactly.
Medications
Among the medications used to treat CVI are:
Antibiotics to treat CVI-related skin infections or ulcers. These drugs do not address the underlying condition.
Anticoagulants, sometimes known as “blood thinners,” are medications used to treat and prevent blood clots.
Unna boots are medicinal wraps. To create a semi-rigid bandage, this wrap combines multilayer compression with a wound cover comprised of zinc oxide gel.
Nonsurgical therapy
Nonsurgical CVI therapies include:
Sclerotherapy–
It involves injecting a foam or liquid solution into a spider or varicose vein. As a result, the vein collapses or disappears.
Endovenous thermal ablation:
This procedure focuses on big veins. It generates tremendous heat by using a laser or high-frequency radio waves. Follow your provider’s instructions exactly.
Surgery
More severe forms of venous insufficiency may necessitate surgery. Your doctor may advise you to undergo one of the following surgical procedures:
Surgical vein or valve repair
Taking out (stripping) the injured vein
Endoscopic surgery with minimally invasive techniques: To aid in seeing and tying off varicose veins, the surgeon puts a tiny tube with a camera on it.
Vein bypass surgery-
It involves the transplantation of a healthy vein from another part of your body. Only used in the upper thigh and as a last resort in the most severe instances.
What can a person do to avoid chronic venous insufficiency?
CVI cannot always be avoided. However, by making simple lifestyle adjustments, you can reduce your chance of CVI and other vein disorders. These are some examples:
- Avoid smoking and using tobacco.
- Avoid wearing constrictive apparel, such as girdles or belts.
- Don’t sit or stand for an extended period. “Try to stand up and walk around frequently.”
- Consume a heart-healthy diet. This includes lowering your sodium (salt) consumption.
- Exercise regularly.
- Maintain a healthy weight.
- If you’ve experienced DVT, your doctor may advise you to take anticoagulants.
FAQ
Is it possible to treat venous insufficiency?
Treatment will not be able to repair the damage to your vascular valves. However, it can alleviate your symptoms and improve your quality of life. Some procedures and surgeries can target and remove damaged veins, preventing blood from flowing through them.
Is it possible to treat venous insufficiency naturally?
To begin, I want to emphasize that there is no method to reverse the source of venous insufficiency, just the symptoms. Damaged venous valves cannot be restored, however there are numerous techniques to reduce the impact of the reflux they cause.
How can I naturally mend my veins?
7 Natural Ways to Strengthen Your Veins | The Center For…
Let’s go over seven natural techniques to strengthen your veins and boost your overall health.
Consume foods high in fiber.
Drink plenty of water….
Take vitamins and supplements.
Work exercise on a regular basis….
Put on compression stockings.
Smoking should be avoided.
Which vitamin is best for venous insufficiency?
B3 vitamin niacin
Niacin is one of the most beneficial vitamins for vein health. This type of B3 vitamin enhances blood circulation, lowers cholesterol levels, and reduces inflammation. Niacin is present in a variety of foods, including turkey, oatmeal, tuna, chicken, and turkey, as well as peanuts.
What is the latest venous insufficiency treatment?
Radiofrequency occlusion, also known as VenefitTM, is the application of heat from electrical energy to break the vein wall. A hollow tube with electrodes at its tip is placed through a tiny incision below the knee during this surgery. It warms the injured vein’s walls in 20-second spurts.
References
- Chronic venous insufficiency. (2021, August 8). Johns Hopkins Medicine. https://www.hopkinsmedicine.org/health/conditions-and-diseases/chronic-venous-insufficiency
- Professional, C. C. M. (n.d.-c). Chronic venous insufficiency (CVI). Cleveland Clinic. https://my.clevelandclinic.org/health/diseases/16872-chronic-venous-insufficiency-cvi
- Dumain, T. (2018, January 19). What is chronic venous insufficiency? WebMD. https://www.webmd.com/dvt/dvt-venous-insufficiency
- Wikipedia contributors. (2023d, December 8). Chronic venous insufficiency. Wikipedia. https://en.wikipedia.org/wiki/Chronic_venous_insufficiency
- The Healthline Editorial Team. (2023, June 12). Venous insufficiency. Healthline. https://www.healthline.com/health/venous-insufficiency#prevention



3 Comments