Neuropathic pain
What is Neuropathic pain?
Damage or injury to the nerves in the central or peripheral nervous system can induce neuropathic pain. Some patients may experience chronic pain in the body as a burning sensation, sharp, while furthers experience tingling and numbness. Injury or disorder can injure the nerve fibers, disrupting the pain alerts the nerves transmit to and accept from different parts of the body.
Nerve injury can create new signals, distort existing signals, or control the usual signals from moving. Furthermore, it can occasionally make non-pain signals sense pain. These issues can cause aching symptoms, which can vary from mild to severe. Damage to the nervous system involves the senses, so a patient may have differences in the way they experience temperature, touch, motion, and pressure.
Types of Neuropathic pain
Many different types of neuropathy affect various nerves and parts of the body. Damage to one nerve is known as mononeuropathy, while damage to two or more nerves in various places is known as multiple mononeuropathies. In most patients, there is an injury to many nerves, which is known as polyneuropathy. The passages below will look at some other kinds of neuropathy and define which body parts they tend to involve.
Peripheral neuropathy
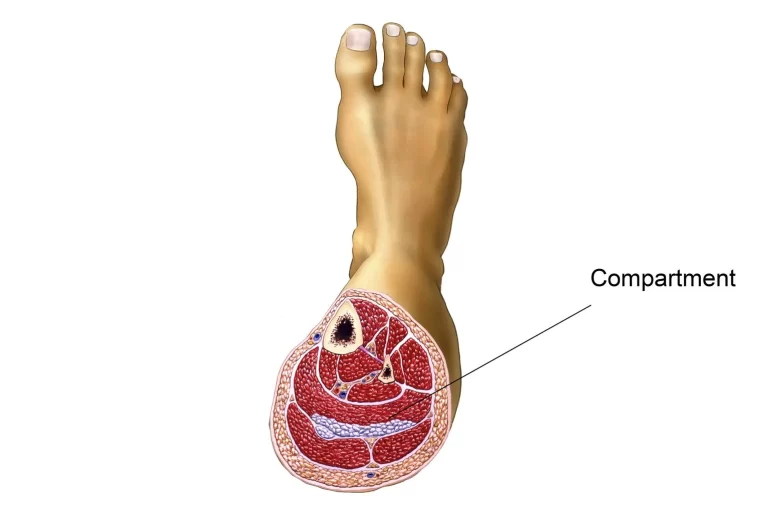
Peripheral neuropathy is a kind of nerve damage that involves the peripheral nervous system. The peripheral nervous system transmits signals between the central nervous system and the remains of the body.
Peripheral neuropathy can involve the extremities of the body, involving:
- feet
- legs
- arms
- hands
Autonomic neuropathy
Autonomic neuropathy involves the nerves that regulate the internal organs and controls essential roles like breathing and digestion. Autonomic neuropathy can cause a range of issues that can involve the blood pressure, heart, and digestive system.
Focal neuropathy
Focal neuropathy is generally damage to a single nerve within one of the following bodily areas:
- head
- hand
- torso
- leg
Bell’s palsy is a kind of focal neuropathy. This disease causes a sudden weakness or immobility on one side of the face. Focal neuropathy can also induce double vision and sudden weakness or ache in the front of the thigh and other regions of the body.
Proximal neuropathy
A rare kind of nerve injury is proximal neuropathy. This kind of nerve injury is generally only on one side of the body and can involve the buttock, hip, or thigh. Proximal neuropathy can induce severe aches and a problem with motion, as well as weight and muscle loss.
Diabetic neuropathy
Diabetes induces high blood sugar in the body. Over time, this can harm the blood vessels that provide vital oxygen and nutrients to the nerves. The reduction in oxygen and nutrients makes it hard for the nerves to work as usual. Diabetic neuropathy can contain any of the above kinds of neuropathy, but up to 50% of patients with diabetes will have peripheral neuropathy.
Compression mononeuropathy
Compression mononeuropathy guides injury to a single nerve from a compression injury or blood vessel disorder. Narrowing of the blood vessels can limit blood flow to the nerves, involving how they work. Injury or repetitive stress can cause compression in nerves as they pass over a joint or junction or via a tight course in the body. Carpal tunnel syndrome, which guides to compression of the median nerve at the wrist, is the most familiar example. A person may experience numbness, tingling, or swelling in the fingers, especially when using the hands or resting at night.
Phantom limb syndrome
Phantom limb syndrome is a kind of neuropathic ache. A person may experience sensations or ache in a lost limb. The ache may be prickling, burning, or shooting. Nearly 80% of the person who has undergone amputation will feel phantom limb syndrome. Combined signals from the brain and spinal cord may be the reason for phantom limb syndrome. Symptoms will frequently reduce in the 6 months following surgery, but they can persist for years.
Trigeminal neuralgia
Compression or injury to the trigeminal nerve in the head can induce trigeminal neuralgia. MS, Stroke, and facial surgery can all cause injury to the trigeminal nerve. This kind of neuropathy can cause extreme pain in the face. Everyday actions like brushing the teeth and cleaning the face may activate pain.
Post-herpetic neuralgia
Postherpetic neuralgia (PHN) is a difficulty of shingles. Postherpetic neuralgia can involve regions of the body where a shingles rash was present. About 10-18% of people with shingles will produce postherpetic neuralgia, and older grown-ups with shingles are more probable to feel it.
Thoracic or lumbar radiculopathy
Thoracic or lumbar radiculopathy is a kind of mononeuropathy that involves one or both sides of the chest or abdominal wall. A person with type 2 diabetes is more probable to experience this kind of neuropathy. They frequently heal with time. More regarding the character of neuropathic pain
Related to the pain there may also be:
Allodynia. This suggests that the pain arrives on, or evolves worse, with a contact or stimulus that would not usually cause pain. For instance, a little touch on the face may activate pain if you have trigeminal neuralgia, or the force of the bedclothes may initiate pain if you have diabetic neuropathy.
Hyperalgesia. This indicates that you obtain extreme aches from a stimulus or touch that would commonly cause only little discomfort. For instance, a gentle prod on the aching location may cause extreme pain.
Paraesthesia. This indicates that you obtain unpleasant or aching sensations even when nobody is feeling you and no stimulus. For instance, you may have aching pins and needles, or electric shock-like feelings.
What causes neuropathic pain?
The most familiar causes of neuropathic pain can be separated into four main categories: disease, infection, injury, and loss of limb.
Disease
Neuropathic pain can be a symptom or difficulty of several disorders and diseases. These contain multiple myeloma, multiple sclerosis, and other kinds of cancer. Not everyone with these states will experience neuropathic pain, but it can be a problem for some.
Diabetes is liable for 30 percent of neuropathic patients, according to the Cleveland Clinic. Chronic diabetes can affect how your nerves work. Patients with diabetes generally experience loss of sensation and numbness, followed by burning, pain, and stinging, in their limbs and digits.
Long-term extreme alcohol input can cause many difficulties, involving chronic neuropathic pain. Injury to nerves from chronic alcohol usage can have long-lasting and aching outcomes.
Trigeminal neuralgia is a distressing situation with severe neuropathic pain on one side of the face. It’s one of the more familiar kinds of neuropathic pain and it can happen without a known reason.
Lastly, cancer therapy may cause neuropathic aches. Chemotherapy and radiation can both affect the nervous system and cause notable pain signals.
Injuries
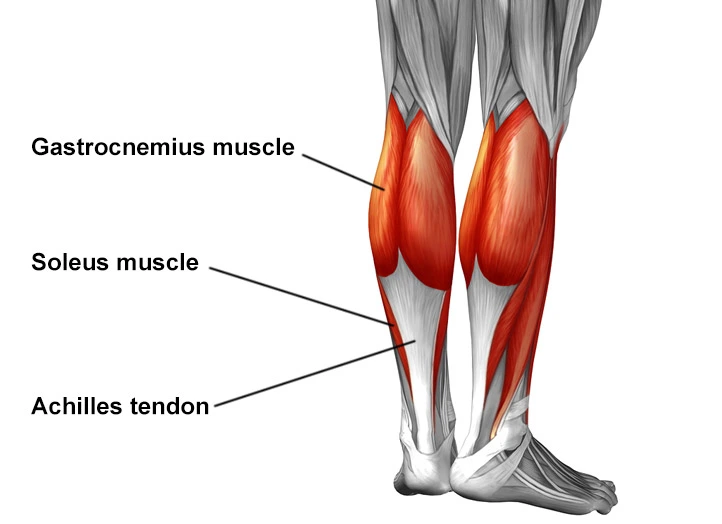
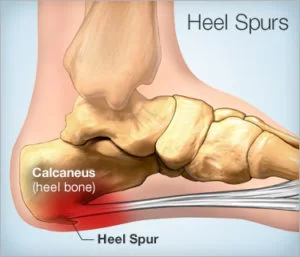
Injuries to muscles, tissue, joints, or junctions are an unusual cause of neuropathic pain. Also, leg, back, and hip issues or damages can cause lasting injury to nerves. While the damage may recover, the injury to the nervous system may not. As an outcome, you may experience constant aches for many years after the accident. Accidents or damages that involve the spine can cause neuropathic aches, too. Herniated discs and spinal cord compression can hurt the nerve fibers near your spine.
Infection
Infections infrequently cause neuropathic pain. Shingles, which are caused by the reactivation of the chicken pox virus, can activate several weeks of neuropathic aches along a nerve. Postherpetic neuralgia is an irregular complication of shingles, affecting constant neuropathic pain. A syphilis infection can also lead to a stinging, burning unexplained ache. A person with HIV may feel this unexplained ache.
Limb loss
An unusual form of neuropathic pain known as phantom limb syndrome can happen when an arm or leg has been amputated. Despite the loss of that limb, your brain still feels its receiving ache alerts from the removed body parts. What occurrence, yet, is that the nerves near the amputation are miscarrying and transmitting incorrect signals to your brain. In extra to arms or legs, phantom aches may be felt in the toes, fingers, ears, penis, and further body regions.
Other causes
Other causes of neuropathic pain contain:
- vitamin B deficiency
- carpal tunnel syndrome
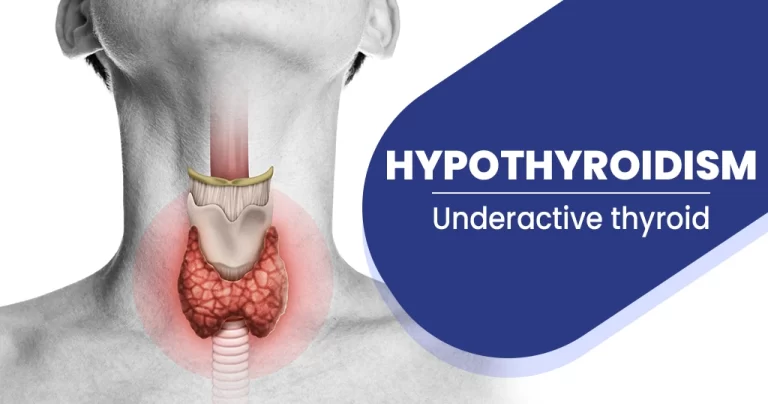
- thyroid problems
- facial nerve problems
- arthritis in the spine
- cancer and cancer therapies, like chemotherapy
- neurological diseases, like multiple sclerosis (MS)
- neurodegenerative diseases, like Parkinson’s disease
- stroke
- shingles
- HIV
- Hansen’s condition (leprosy)
- Guillain-Barre syndrome
- blood vessel disease
- vascular malformations
- autoimmune conditions
What are the Symptoms of Neuropathic pain?
Some symptoms of neuropathic pain can contain:
- extreme pain, which may sense like throbbing, shooting, or burning
- electrical-like sensations
- numbness
- a tingling sensation, or pins and needles
- decreased use of the senses, like problem-sensing temperatures
- skin that seems mottled or red
- itchiness
- changes in pain associated with the weather
Neuropathic pain can also cause a patient to be overly sensitive to touch. For instance, a person may find that the least pressure or friction from clothing or a soft touch can aggravate the nerves and cause pain.
Chronic pain can involve day-to-day life and impact a patient’s quality of life. Some side impacts of neuropathic pain may contain:
- a problem in sleeping, due to pain
- depression
- anxiety
Diagnosis
One of the challenges, of neuropathic aches, is the capability to evaluate them. There is a dual element to this: evaluating intensity, quality, and progress; and accurately diagnosing neuropathic aches.
There are, yet, some diagnostic devices that may help clinicians in assessing neuropathic aches. example nerve conduction examinations and sensory-evoked potentials can recognize and quantify the degree of damage to sensory, but not nociceptive, ways by observing neurophysiological reactions to electrical stimuli.
Mechanical sensitivity to tactile stimuli is estimated with von Frey hairs, vibration sensitivity with vibrators, pinprick with weighted syringes, and thermal ache with thermos.
It is also very essential to conduct a thorough neurological evaluation to determine motor, sensory and autonomic dysfunctions. Eventually, there are multiple questionnaires used to determine neuropathic aches from nociceptive.eg., the Neuropathic Questionnaire11 and ID Pain.
How’s Neuropathic pain treated?
The purpose of neuropathic pain therapy is to determine the underlying disease or illness that’s liable for the pain, and treat it, if feasible.
An essential purpose is that your doctor or physician will aim to feed pain ease, assist you in keeping typical abilities despite the ache and enhance your quality of life.
Medical treatment
The most familiar therapies for neuropathic pain contain:
Over-the-counter pain medication
Nonsteroidal anti-inflammatory drugs (NSAIDs), like Aleve and Motrin, are occasionally used to treat neuropathic aches. Yet, many patients find these drugs aren’t useful for neuropathic aches because they don’t target the basis of the pain.
Prescription medication
Opioid pain drugs don’t generally relieve neuropathic pain as well as they decrease other kinds of pain. Plus, doctors or physicians may hesitate to define them for worry that a patient may evolve dependent. Topical ache relievers can be used, too. These contain capsaicin patches, lidocaine patches, prescription-strength ointments, and lotions.
Antidepressant drugs
Antidepressant drugs have shown great commitment to treating symptoms of neuropathic aches. Two common kinds of antidepressant medications are specified for a patient with this situation:
tricyclic antidepressants
serotonin-norepinephrine reuptake inhibitors
These may treat both the ache and symptoms of depression or anxiety induced by chronic aches.
Anticonvulsants
Anti-seizure drugs and anticonvulsants are frequently used to treat neuropathic aches. Gabapentinoids are most typically defined for neuropathic aches. It’s not clear why anti-seizure medications work for this situation, but investigators think the drugs interfere with ache signals and stop false information.
Nerve blocks
Your doctor or physician may inject local anesthetics, steroids, or further pain drugs into the nerves that are supposed to be liable for the wayward ache signals. These blocks are temporary, so they must be replicated to maintain working.
Implantable device
This invasive method needs a surgeon to implant a machine in your body. Some machines are used in the brain and some are used in the spine. Once a machine is in place, it can transmit electrical impulses into the spinal cord, brain, or nerves. The instincts may stop the periodic nerve signals and manage symptoms. These machines are generally used only in people who haven’t reacted well to other treatment choices.
Physiotherapy treatment in Neuropathic pain
Neuropathic pain frequently reacts badly to standard pain therapies and sometimes may get more harmful rather than better over time. For some patients, it can lead to severe disability. A multidisciplinary process that combines treatments, nevertheless, can be a very useful way to provide ease from neuropathic aches. The multidisciplinary method involves:
- TENS therapy
- Low-impact general physical activities
- Counseling
- Relaxation therapy
- Massage therapy
- Acupuncture
Physical therapy modalities and rehabilitation methods are necessary choices and must be evaluated when pharmacotherapy alone is not adequate. Physical therapy attacks the physical side of the stiffness, inflammation, and soreness with manipulation, activity, and massage, but it also functions to assist the body to recover itself by stimulating the creation of the body’s normal pain-relieving chemicals. This two-pronged strategy is what assists make physical therapy so useful as pain therapy.
Laser therapy
In addition to that, activity is beneficial to reorganize and sprouting the cortical body representation: the profound difference in the neuro matrix related to chronic aches it is an element of central sensitization.
TENS treatment has low-quality of proof for being useful in the therapy of aching peripheral neuropathy. Low-level laser treatment could otherwise have positive impacts on the managing of analgesia for neuropathic aches.
Neurostimulation approaches involving spinal cord stimulation (SCS) and deep brain stimulation (DBS), transcranial magnetic stimulation (TMS), and cortical electrical stimulation (CES) have also been found useful in the therapy of neuropathic aches.
Mirror therapy
Activity and motion representation methods (that is, therapies like mirror therapy and motor imagery that use the observation and/or imagination of typical pain-free motions) have been proposed to be useful in neuropathic ache management. Newly, mirror therapy has been used for not only persons with phantom limb aches but also for persons with complex regional ache syndrome and strokes. Yet, the quality of proof supporting these interventions for neuropathic aches is weak and requires further analysis.

Exercise
Exercising for just 30 minutes a day on at least three or four days a week will assist you with chronic ache management by improving: Muscle Endurance, Power, Flexibility in the muscles and joints or junctions, and Stability in the joints or junctions. Maintaining a constant exercise habit will also assist in managing pain. Routine therapeutic activity will assist you to keep the capability to move and function physically, instead of evolving disabled by your chronic ache.
Studies are showing that activity may be an essential part of the therapy and prevention of neuropathic aches after chemotherapy. Although more data is needed and precise exercise prescriptions do not yet exist for persons obtaining cancer therapy. It has been also found that physical activity, like forced treadmill running and swimming, can adequately enhance mechanical allodynia and heat hyperalgesia in animal examples of neuropathic aches.
What is the prognosis for neuropathic pain?
Many persons with neuropathic aches can find some action of ease, even if their pain continues. Although neuropathic ache is not dangerous to a person, the presence of chronic ache can negatively affect the quality of life. Persons with chronic nerve aches may sorrow from sleep lack or mood disturbances, involving depression and stress. Because of the underlying neuropathy and absence of sensory feedback, persons are at risk of creating damage or infection or unknowingly inducing an escalation of current damage.
FAQ
What can I take for the pain?
For many, the ache from nerve injury can be intense even debilitating. Ask your doctor or physician what pills are available for the ache. Medicines can vary from over-the-counter pain relievers to pharmaceutical painkillers. Different other pill medications are also used to treat neuropathy aches, involving both anti-seizure and anti-depressant drugs. Though they may not destroy the pain, they can bring the edge off and assist calm overactive nerves. Reforming the peace can assist bring you your life back and permit you to concentrate on something further than the pain.
What negative side impacts should I worry about with prescription medications?
Many prescription drugs have a long list of adverse side consequences and those used to manage nerve aches are no exception. For instance, anti-seizure medications a popular therapy for neuropathy have a long list of side effects involving dizziness, drowsiness, blurred vision, nausea, confusion, and more. Knowing the possible risks upfront can assist you to make an informed conclusion about which drugs to try and which to avoid. Your doctor or physician can assist describe any potential risks and assist you to weigh them against potential advantages.
Should I be tested for a vitamin deficiency?
One of the potential reasons for peripheral neuropathy is a lack of vitamin B12. This essential vitamin assists build and keep a protective coating around the nerves called the myelin sheath. Also, vitamin B12 benefits boost and repair broken nerves. A deficiency in this essential vitamin has been related to nerve injury and peripheral neuropathy. If there are no evident reasons for your symptoms (i.e. chemotherapy, diabetes, recent surgeries, etc) ask your doctor or physicians about whether or not he/she thinks a vitamin deficiency could be contributing to the issue. If they deem it essential, they can run a simple test to decide whether a deficiency of vitamin B12 is playing a part in your peripheral neuropathy or not.
What is the difference between a neuropathic ache and a nerve ache?
Nociceptive ache is the body’s natural protection against damaging surfaces or actions. On the further hand, there is neuropathic ache. This ache is the consequence of injury to the nervous system and is usually chronic. Unlike nociceptive ache, neuropathic ache does not require to develop in reaction to any outside stimulation.
What is the difference between neuropathy and neuropathic pain?
Neuralgia and neuropathy are both words used to denote medical issues and diseases related to the nerves in the somatosensory system, a portion of the sensory nervous system. Neuralgia or neuropathy is also guided to as neurogenic ache or neuropathic ache.