Cold therapy (Cryotherapy)
What is Cold Therapy (Cryotherapy)?
- Cold therapy (Cryotherapy), also known as ice application, is the simplest and oldest way to treat injuries.
- Its worldwide use spread because of its effectiveness, convenience, low cost and ease of transportation.
- Ice is believed to control pain by instigating local anaesthesia. It also decreases oedema, nerve conduction velocities, cellular metabolism, and local blood flow.
- The effect of the cryotherapy depends on the method, the duration, temperature of the ice and the depth of the subcutaneous fat.
- The application of cold to the tissue after injury is a practice as old as medicine itself.
- Nowadays the local temperature of the tissue may be reduced by the application of various forms of ice or frozen gel packs or by the evaporation of volatile fluids from the skin.
- Often the skin temperature is reduced to 10’C.
Physical principles of cold therapy :
- When ice is applied to the skin, heat is conducted from the skin to the ice in order to melt it.
- To change its state, the ice requires considerable energy.
- The raise the temperature of 1 g of ice at 0’to 1 g of water at 37 ‘c requires 491 J.
- Whereas raising 1 g of water at 0’C to 37’C requires only 155 J.
- Consequently, when trying to cool tissues it is important to use ice during treatment and not just cold water.
Physiological effects :
Circulatory response
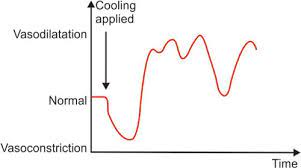
- The initial response of the skin to cooling is an attempt to preserve heat and this is accomplished by an initial local vasoconstriction.
- This hemostatic response has the effect of allowing the part to become very cold.
- After a shorter period, there follows a vasodilatation and then alternate periods of constriction and dilatation.
- This apparent hunting for a mean point of circulation is called Lewis’s hunting reaction.
Uses of physiotherapy in circulatory effect –
- Limit the extravasation of blood into tissue such as sport injury
- Reduce swelling
- Increase circulation
- The reduced metabolic rate of cooled tissue
Neural response
- The skin contains primary thermal receptors.
- There are several times colder than warm receptors.
- The cold receptors respond to cooling by a sustained discharge of impulses, the rate of which increases with further cooling.
- The first fibres affected by gradual cooling is A fibers.
- Fibres affected = very low temperatures than the B and in last C are affected.
- For motor paralysis = fibres A
- Deep pain = fibres C
Reduce pain
- This is one of the major effects of ice.
- Ice has been used to relieve pain for many years.
- Ice is working on the pain gate theory.
Reduction of spasticity
- Spasms and muscle spasticity have been reduced by ice.
Techniques of application of Cold therapy :
- Ice towels
- Ice packs
- Immersion
- Ice cube massage
- Excitatory cold
- Cold compression unit
- Cold / ice sprays
Ice towel

- This is a popular method of application.
- Because there is little danger of producing an ice burn.
Preparation of ice towel
- Prepare the bed by removing the blankets and sheets, and cover it with waterproof material.
- Adequately expose the part to be treated.
- Protecting any clothing that the patient needs to wear.
- Prepare the ice solution by filling a bucket or large bowl with two parts flaked or crushed ice to one part water.
- This mix should give a mulch, in which two terry towels are immersed.
Application of ice towel

- The surplus water is wrung from one towel, leaving as much ice clinging to it as possible.
- It is then applied to the part being treated.
- The towels are changed when they have been in position for at least 30 seconds, but not longer than 2 minutes.
- Up to ten towels can be applied consecutively.
- Total treatment time is of the order of 15 -20 minutes.
Modification of technique :
- In the presence of swelling, it is permissible to elevate the limb and completely surround the joint with the ice towels.
- The patient can exercise with the towel in the position
- For spastic muscle with the towel, the patient applies relaxation/facilitation techniques.
Ice pack

- Crushed of flaked ice may be placed inside a specially made terry – towel bag or an ice towel folded into an appropriate shape.
Preparation of ice pack
- A gutter made of polythene sheet is folded and placed on the bed.
- A folded towel is placed underneath its edges in order to channel the water produced from the melting ice into a container at the side of the bed.
- The gutter will be positioned below the part to be treated
Preparation of the patient
- The part to be treated is exposed and put into a comfortable position over the prepared gutter.
- A vegetable or nut oil is spread over the skin on which the ice pack is to be placed.
- This is to try and prevent burn.
- Ice burn is produced by supercooling the skin.
- This may occur if water from the pack accumulates between the pack and the skin.
- It absorbs salts from the skin and becomes very cold.
- The layer of oil causes the water produced by the melted ice to run quickly and easily off the skin and into the gutter, so preventing supercooling.
- Oil also has a very low freezing point and prevents the pack from freezing itself to the patient’s skin.
- Melting of the ice is an essential part of the treatment as the water produced conducts heat from the skin to the ice inside the pack.
Application of the patient
- The wet ice pack is placed on top of the part to be treated.
- Packs should never surround a limb as this would inevitably put pressure on one aspect of the limb and could reduce circulation locally.
- Reduced circulation would prevent a normal circulatory response to cooling and might precipitate an ice burn.
- The pack may be left in position for between 10 and 20 minutes.
Immersion

- Immersion is a technique in which the part to be treated is immersed in an ice solution.
- Unfortunately, it is only practical to immerse certain areas such as hands, feet, and elbows.
Preparation of immersion
- The solution is made up of 50 percent ice and 50 percent water placed in a suitable container.
Application of the immersion
- The patient immerses the part in the solution and keeps it in either for a single ten – minutes session or for a series of shorter immersions until a cumulative total of ten minutes has been reached.
- Often the patient experiences intense pain in the immersed area, sometimes severe enough to cause him to faint.
- He should therefore be suitably supported and watched throughout the treatment.
Ice – cube massage

- Ice cube massage is a useful method of application as it does not require an ice machine.
- The freezer compartment of a domestic refrigerator is sufficient.
- This makes this technique useful in small departments, inwards, and most importantly in the home.
Preparation of ice-cube massage
- A large block of ice, and water frozen in a yogurt pot, has one end wrapped in a towel, and the other end is left free.
- The patient was adequately exposed and supported.
Application of ice-cube massage
- The exposed end of the ice block is massaged in a circular manner over the treatment area, applying only minimal pressure to the part.
- The maximum time of application is ten minutes.
- The desired effect may be achieved before this.
- This technique is particularly useful in the treatment of bedsores about 2 minutes.
- The skin is then gently dried.
- The ice application is repeated three or four times.
- A marked increase in circulation is achieved almost immediately and this should accelerate repair.
- A similar technique can be used on pressure areas that are treating to break down as the increase in circulation may prevent this happening.
Excitatory cold
- The marked sensory stimulation of ice on the skin may be used to facilitate the contraction of inhibited muscles.
- It is necessary first to ascertain the spinal root level supply of the inhibited muscle and then to find the area of skin which has the same root supply,
- Once this has been done, the ice is stroked quickly three times over the dermatomes, and the skin is then dried.
Cold therapy machine :
Following cold therapy machines are used commonly for treatment.
Cold compression unit

- Cold therapy with compression – Cold water is circulated in a sleeve which is put over the limb and part of it is inflamed at intervals.
Cold/ice sprays

- Ethyl chloride was originally used but it is highly inflammatory and thus poses some risks.
- Fluoro methane is now used widely as it is noninflammable.
- The liquid is sprayed onto the area to be cooled in a series of strokes of about 5s each with a few seconds intervals between each.
- The nozzle is held at the angle of 45 or right angle from the skin surface.
Timing of cold therapy in some clinical Problems & Clinical Objectives :
| NO. | Clinical Problem | Timing | Clinical Objectives |
| 1 | Pain | Acute Phase (First 72 hours after a flare-up or injury) | To reduce pain |
| 2 | Inflammation | Acute Phase (First 72 hours after a flare-up or injury) | To limit the extent of the inflammatory reaction |
| 3 | Oedema | 72 hours – 7 days | To assist in phagocytosis of the dead cell material To control extraarticular swelling To quickly resolve intraarticular swelling |
| 4 | Swelling: Intraarticular | After 7-10 days | To assist in the resolution of swelling, normalization of movement, and return of a function (including strengthening) |
| 5 | Swelling: Extraarticular | After 7-10 days | To assist in the resolution of swelling, normalization of movement, and return of function (including strengthening) |
What is cold therapy used for?
Medical uses of Cold therapy in the following conditions are recommended.
Indication of cold therapy :
- To decrease swelling/edema following trauma – Cooling in water at 8 º C for 30 minutes decreases edema.
- To treat burns
- To inhibit spasticity – In spasticity, the muscle must be cooled; this process takes 10 minutes in thin patients and up to 60 minutes in obese persons.
- To reduce muscle spasm
- To reduce the acute inflammatory reaction
- To reduce pain
- To reduce limb metabolism (prior to amputation)
- To produce reactive hyperemia
- To facilitate muscular contraction for various forms of neurogenic weakness and for muscle re-education
- To treat restricted knee flexion due to traumatic lower extremity fractures – This improves the condition to a greater degree than superficial heat application, even if either is used in combination with passive stretching using mechanical traction.
- Immediate application of ice or cold packs for superficial burns and for burns on less than 20% of the total body surface area decreases pain, edema, erythema, and blistering.
- For optimal results in cases of trauma, cold should be applied before significant edema and hemorrhage occur.
Conditions treated by cold therapy :

- Acute soft tissue injuries e.g. ankle sprain, muscular sprain, ligament sprain
- Myofascial trigger points
- Tendinitis
- Acute swelling
- Bursitis
- Post orthopedic surgery e.g. TKR, ACL reconstruction, arthroscopic shoulder surgery.
- Acute sports injuries
- DOMS
Contraindications to ice treatment :
- Psychological conditions
- Cardiac conditions
- Peripheral nerve injuries
- Vasospastic disease [ Raynaud’s disease]
- Peripheral vascular disease
- Cold sensitivity
- RPS,
- Haemoglobinuria,
- Cryoglobulinemia,
- Urticaria
- Skin anaesthesia
Possible Risks/Undesirable Effects :
Inhibit Muscle Function
- Cooling can temporarily Inhibit muscle function with the potential for increased risk of injury/re-injury.
- Be cautious when having patients weight bear/undertake complex exercises after icing a lower extremity.
Ice Burn
- Elderly patients with impaired sensation and/or circulation will be more vulnerable to an ice burn, therefore consider using less intense icing techniques (e.g., moderately cold ice pack wrapped in an insulating layer(s) of towel/cloth).
- Younger patients with intact sensation and circulation may benefit most from the direct immersion of the limb in cold water and then progressively adding ice cubes.
- Cold gel packs stored in a freezer have a surface temperature below 0°C (32°F) and thus an insulating layer should be used between the cold pack and the patient’s skin.
Cryotherapy-Induced Nerve Injuries
- Most common when cold is applied in combination with compression.
- Check capillary refill during the application of ice combined with compression therapy to ensure adequate blood flow.
Generalized Cooling and Decrease in Core Temperature
- Shivering and piloerection are signs of a decrease in core temperature which may compromise patient safety (especially in the elderly and those with fever)
- The application of therapeutic cryotherapy should produce only local effects
Reduced ROM
- Ice may contribute to a shortening of collagen fibres in connective tissue
- After gaining ROM by warming, stretching, and then strengthening in the newest part of the ROM, it is likely counterproductive to cool the tissue in a shortened position
- If one wishes to cool the tissue post-stretch and exercise, it is best to do so with the tissue in a lengthened position
- In patients with significantly restricted ROM due to scar tissue, it may be preferable not to use ice






4 Comments