Congenital Muscular Dystrophy (CMD)
What is a Congenital Muscular Dystrophy (CMD)?
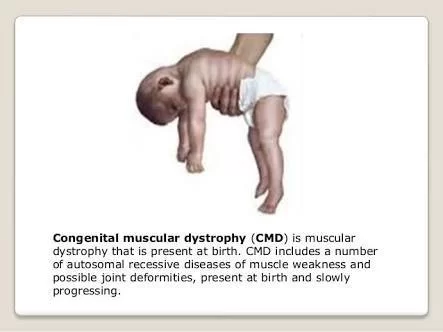
→ Congenital muscular dystrophy (CMD) refers to a group of muscular dystrophies that become apparent at or near birth. Muscular dystrophies in general are genetic, degenerative diseases primarily affecting voluntary muscles.
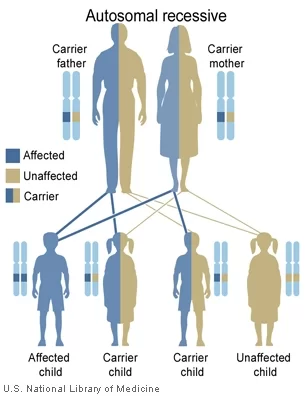
→ Congenital muscular dystrophies are autosomal recessively-inherited muscle diseases.
Signs / Symptoms
→ CMD will display some progressive muscle weakness or muscle wasting (atrophy), although there can be different degrees and symptoms of severeness of progression. The weakness is indicated as hypotonia, or lack of muscle tone, which can make an infant seem unstable.
→ Children may be slow with their motor skills; such as rolling over, sitting up or walking, or may not even reach these life milestones. Some rarer forms of CMD can result in significant learning disabilities.

Classification
(1) CMD with brain-eye – also called muscle-eye-brain disease is a rare form of congenital muscular dystrophy (autosomal recessive disorder) causing a lack of normal muscle tone which can delay walking due to being weak, also paralysis of eye muscles, and intellectual disability
(2) CMD with adducted (drawn inward) thumbs – a rare form of CMD causing permanent shortening of the toe joints and lack of muscle tone which can delay walking due to the individual being weak. Children have may mild cerebellar hypoplasia in some cases.
(3) CMD/LGMD without MR – first years of a newborn begins with weakness, which affects motive skills, walking can be accomplished in adolescence, deformity, and rigidity of joints. The joints, neck, and spine; progressive cardiomyopathy at the early ages; cardiac rhythm abnormalities may be present
(4) CMD/LGMD with MR – weakness and deformity and rigidity joints present at birth, poor muscle tone, slowly progressive; individuals may present with cerebellar cysts (or cortical problems), and microcephaly may be present as well. Abnormal flexibility might occur, and spinal curvature is possible.
(5) Large-related CMD – at the beginning of the newborn period, the issues the infant receives are; poor muscle tone and weak motor function; the individual will present with mental retardation and the structure of the brain will likely be abnormal.
(6) CMD with cerebellar atrophy – severe cerebellar hypoplasia, poor muscle tone, delayed in motor milestones, lack of coordination in motive skills, difficulty speaking, involuntary movements, and some intellectual disability. Furthermore, muscle biopsy does not reveal any deficiency.
(7) Walker–War burg syndrome – low muscle tone at birth or during early infancy; small muscles; the majority of affected children do not live more than 3 years of age. Eye structure problems are present, with accompanying visual impairment.
(8) CMD with primary laminin-a2 (merosin) deficiency (MDC1A) – intellect in such individuals is unaffected, proximal muscle weakening and rigid spine are present along with respiratory involvement (with disease progression).
(9) CMD with spinal rigidity – present at birth can have poor muscle tone and weakness, reduced respiratory capacity, muscles could be deformed, beginning early ages stabilization or slow decline spinal rigidity, limited mobility to flex the neck and spine, spinal curvature and progressing deformity and rigidity joints, minor cardiac abnormalities, normal intelligence.
(10)CMD with lamina abnormality – within the first year the infant is weak, and an individual may have problems later lifting arms and head. May need a nasogastric tube, limb weakness, and elevated serum creatine kinase.
(11)Fukuyama CMD – -in western countries this type of CMD is rare but is common in Japan. The effects this disease has on infants is a spectrum of severity, weakness in muscle tone within the first year, some infants may achieve walking, deformity and rigidity joints, spinal curvatures, seizures, eye involvement, and intellectual disability.
(12)Merosin-deficient CMD – present at birth weakness in muscle tone, spectrum of severity; may show hypotonia and poor motor development. Most individuals have periventricular white matter problems.
(13)Merosin-positive CMD – some forms of merosin-positive CMD are Early spinal rigidity, CMD with muscle hypertrophy, CMD with muscle hypertrophy, and respiratory failure.
(14)Ullrich congenital muscular dystrophy – present at birth is weakness, poor muscle tone, will have some deformity and rigidity joints, some joints will have excessive flexibility, spinal rigidity, curvature, respiratory impairment, soft skin, normal cardiac function, and normal intelligence.
Differential Diagnosis
In an affected individual, the congenital muscular dystrophy DDx is as follows (non-neuromuscular genetic disorders can occur).
- Metabolic myopathies
- Dystrophinopathies
- Emery-Dreifuss muscular dystrophy
Diagnosis
→ Lab study (CK levels)
A blood test will check the level of the muscle protein (creatine kinase (CK)). In about 40% of congenital muscular dystrophy cases, the level of CK is 5 to 20 times higher than normal.
→ MRI (of muscle, and/or brain)
To determine the kind of CMD, an MRI of the muscles may be utilized to display the pattern of affected muscles.
The technique may be performed under general anesthesia on children.
→ EMG
To measure the electrical activity in muscles, an EMG is utilized. To capture the electrical activity of the muscle, a tiny needle is implanted. This might indicate a pattern of abnormal muscle activation.
The technique may be performed under general anesthesia on children.
→ Genetic testing
A blood test that can be used for genetic testing may be available to you. This may assist in determining the kind of CMD that you or your kid has.
→ Muscle biopsy
Your precise kind of congenital muscular dystrophy may be determined with a muscle biopsy.
The technique may be performed under general anesthesia on children.
Treatment of Congenital Muscular Dystrophy (CMD)
→ The American Academy of Neurology recommends that individuals need to have monitoring of cardiac function, respiratory, and gastrointestinal. Additionally, it is believed that therapy in speech, orthopedic, and physical areas, would improve the person’s quality of life.
→ While there is currently no cure available, it is important to preserve muscle activity and any available correction of skeletal abnormalities (such as scoliosis). Orthopedic procedures, like spinal fusion, maintain/increase the individual’s prospect for more physical movement.
Mobility problems
Some kids with CMD are able to walk. For some, it may take longer, and they might not be able to walk until they are five years old or older. Some kids who can walk may lose their ability to walk as they get bigger and heavier. This is due to the possibility that when the youngster ages, their muscles won’t be able to handle the tension.
A specialist may be referred to your kid for:
Physiotherapy to improve the flexibility and strength of the muscles
physical assistance such as crutches, a wheelchair, or a walking stick; occupational therapy to support independence; leg splints to assist your kid in walking.

Heart problems
To check the rhythm of their heart, your kid will get electrocardiograms (ECGs) on a regular basis. They will require an echocardiography as well.
Swallowing problems
It’s possible that your child has trouble eating. To aid with eating, a gastrostomy or nasogastric tube may be implanted.
Prognosis
→ The condition is usually fairly stable as far as the muscle power in the legs and arms is concerned, and often the child appears to gain strength in the first decade of life. In several forms of congenital muscular dystrophy, the acquisition of new skills over time is possible, although some motor difficulties will always be present, depending on how the condition was at presentation.
→ In many congenital muscular dystrophy subtypes, muscle weakness can increase with time and can lead to respiratory problems. This may happen in children of various ages and is potentially a very serious complication which, if not recognized, can be life-threatening.
→ The severity of this condition varies greatly from person to person. As the severity varies even within the same form of congenital muscular dystrophy, it is important not to assume that certain motor developments will or will not take place, but rather to work with children so they can achieve the goals that are within their ability.
Some children will walk, but sometimes this can be delayed until the age of five or older.
→ Leg splints are often used to assist a child to walk. Some children who have achieved independent walking may lose this ability later on because, as they grow older and heavier, the muscles are unable to cope with a greater strain. Other children may not be able to walk at all.
→ The presence and the severity of other problems depend on the subtype of congenital muscular dystrophy. Some features, however, are generally found in many children with congenital muscular dystrophy, irrespective of the subtype.
Surgery
Surgery may be necessary to treat scoliosis and stop it from growing worse.
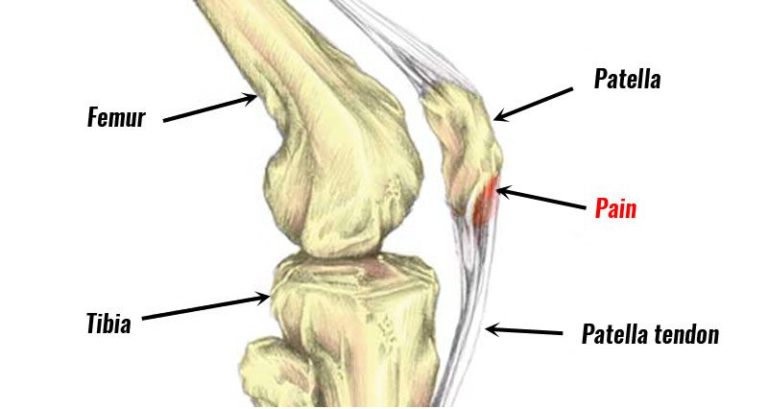
Releasing or extending the tendons surgically can help loosen up tight joints caused by tendon contractures. Movement should be enhanced by this.
Breathing Difficulties
Your child probably won’t be able to breathe on their own and will need a machine to aid them at night and occasionally during the day.
Cough assist devices can help older kids clear their secretions (phlegm) when they cough. Their strength in the muscles of their chest wall can be maintained by using an Ambu bag.
Children with CMD are susceptible to recurring chest infections. Antibiotics could be prescribed.
Educational Support
Many kids with CMD participate in school activities without experiencing any negative effects from their illness. To make the most of their time in school, some people might require additional assistance.
Palliative care
If you or your kid needs assistance coping with their condition, you may want to think about hospice care. The hospice may be able to assist with:
Counseling for pain control.
FAQ
What are the symptoms of CMD?
Symptoms of CMD are:
Low muscle tone, or hypotonia
Tightness, or contractures in the elbows, knees, hips, and ankles.
Respiratory issues are caused by weakened breathing muscles.
Eyesight issues.
Learning challenges.
How do you treat CMD disease?
Surgery to correct skeletal abnormalities; speech therapy; the use of various devices (e.g., canes, braces, walkers, wheelchairs) to assist with walking (ambulation) and mobility; physical and occupational therapy to improve muscle strength and prevent contractures.
What is CMD treatment?
CMD treatments are:
Physical treatment for weakened muscles.
Respiratory treatment for problems with breathing.
Occupational therapy for problems related to swallowing.
Cognitive function is addressed through behavioral therapy.
Nutrition and diet advice for people who have trouble swallowing or chewing.
How is CMD inherited?
The majority of CMD types have an autosomal recessive inheritance pattern. To put it simply, a recessive illness requires two copies of the faulty gene—one from each parent—to manifest. Though they wouldn’t often develop the illness, each parent would be a carrier of the gene defect.
What is the cause of CMD disease?
The cause of CMD disease are:
A genetic abnormality causes CMD. It happens when aberrant muscle function is caused by a defective gene. Even in cases when a parent does not exhibit symptoms, the gene can nevertheless be transferred from parent to kid. Alternatively, the kid may develop muscular dystrophy and be the first in their family.
Can muscular dystrophy be cured?
Muscular dystrophy (MD) has no known cure, however there are some therapies that can help control the illness. The therapy you receive will be customized to meet your needs because different forms of MD can lead to quite distinct difficulties.






3 Comments