Coxa Vara: Deformity in Hip Joint
What is a Coxa Vara?
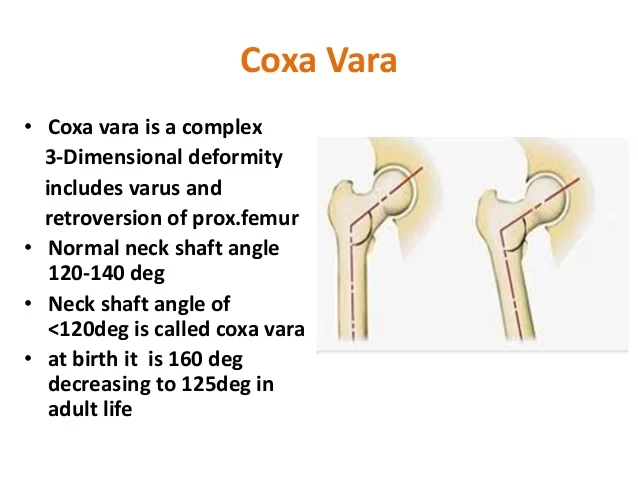
Coxa vara is a deformity of the hip, whereby the angle between the head and the shaft of the femur is reduced to less than 120 degrees. This results in the leg being shortened, and the development of a limp.
It is commonly caused by injury, such as a fracture. It can also occur when the bone tissue in the neck of the femur is softer than normal, causing it to bend under the weight of the body. This may either be congenital or the result of a bone disorder.
The most common cause of coxa vara is either congenital or developmental. Other common causes include metabolic bone diseases (e.g. Paget’s disease of bone), post-Perthes deformity, osteomyelitis, and post traumatic (due to improper healing of a fracture between the greater and lesser trochanter). Shepherd’s Crook deformity is a severe form of coxa vara where the proximal femur is severely deformed with a reduction in the neck shaft angle beyond 90 degrees.

It is most commonly a sequela of osteogenesis imperfecta, Paget’s disease, osteomyelitis, tumour, and tumour-like conditions (e.g. fibrous dysplasia).
Coxa vara can happen in cleidocranial dysostosis.
Anatomy and coxa vara:
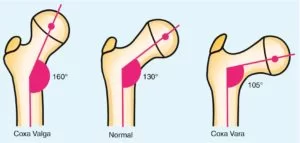
In early skeletal development, a common physis serves the greater trochanter and the capital femoral epiphysis. This physis divides as growth continues in a balance that favors the capital epiphysis and creates a normal neck-shaft angle (angle between the femoral shaft and the neck). The corresponding angle at maturity is 135 ± 7 degrees. Another angle used for the measurement of coxa vara is the cervicofemoral angle which is approximately 35 degrees in infancy and increases to 45 degrees after maturity.
Classification : ( Type Of Coxa Vara )
- Developmental.
- congenital (e.g. congenital short femur, PFFD)
- acquired (e.g. SCFE, infection, Perthes)
- dysplasia (e.g OI, Jansen, Schmid, SED)
- cretinism
Developmental Stages:
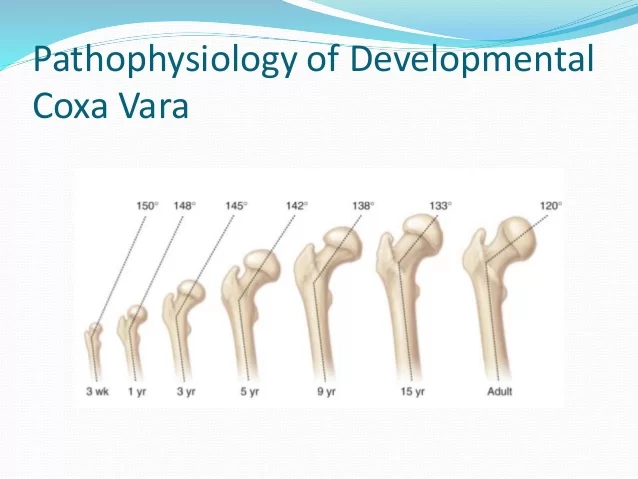
More common cause: primary defect in endochondral ossification of the medial part of the femoral neck.
Excessive interuterine pressure on the developing fetal hip.
vascular insult.
Faulty maturation of the cartilage and metaphyseal bone of the femoral neck.
Clinical feature in Congenital Coxa Vara :
presents after the child has started walking but before six years of age. Usually associated with a painless hip due to mild abductor weakness and mild limb length discrepancy.
If there is a bilateral involvement the child might have a waddling gait or Trendelenburg gait with an increased lumbar lordosis. The greater trochanter is usually prominent on palpation and is more proximal. Restricted abduction and internal rotation.
Differential Diagnosis
Congenital:
- Cleidocranial Dysplasia
- Chondrodysplasia Punctata
- Metaphyseal Chondrodysplasia
- Gaucher’s Disease
- Multiple Epiphyseal Dysplasia
- Proximal Focal Femoral Deficiency
- Spondyloepiphyseal Dysplasia Congenital
Acquired:
- AVN: (DDH or Perthes Disease)
- Fibrous Dysplasia
- SCFE
- Rickets
- Osteomyelitis of Hip
- Septic Arthritis
- Traumatic
- Paget’s Disease
Diagnosis:
The diagnosis of coxa vara typically involves a combination of medical history review, physical examination, and imaging studies.
X-ray :

Decreased neck shaft angle, increased cervicofemoral angle, vertical physis, shortened femoral neck decrease in femoral anteversion. HE angle (hilgenriener epiphyseal angle- angle subtended between a horizontal line connecting the triradiate cartilage and the epiphysisn normal angle is <30 degrees.
Treatment: HE angle of 45–60 degrees observation and periodic follow-up.
Indication for surgery: HE angle more than 60 degrees, progressive deformity, neck-shaft angle <90 degrees, development of Trendelenburg gait
Surgery: subtrochantric valgus osteotomy with adequate internal rotation of distal fragment to correct anteversion common complication is recurrence. If HE angle is reduced to 38 degrees less evidence of recurrence postoperative spica cast is used for a period of 6–8 weeks.
Coxa vara is also seen in Niemann–Pick disease.
Congenital coxa vara :
Presence at birth is extremely rare and associated with other congenital anomalies such as proximal femoral focal deficiency, fibular hemimelia, or anomalies in other parts of the body such as cleidocranial dyastosis. The femoral deformity is present in the subtrochantric area where the bone is bent. The cortices are thickened and may be associated with overlying skin dimples. External rotation of the femur with valgus deformity of the knee may be noted. This condition does not resolve and requires surgical management. Surgical management includes valgus osteotomy to improve hip biomechanics and length and rotational osteotomy to correct retroversion and length.
Treatment of Coxa Vara:
Non-operative Treatment :
Indications OF Treatment :
- Hilgenreiner-ephyseal angle (normal <25 degrees)
- <45 degrees – unlikely to progress
- 45-60 – may progress
- will require close follow-up if non-symptomatic.
Operative Treatment (Surgical) :
Corrective valgus derotation osteotomy (VDRO) :
Indications For surgery :
- Hilgenreiner’s physeal angle > 60°
- Hilgenreiner’s physeal angle between 45-60° if symptomatic (e.g. limp & progression of varus)
- progressive decrease in neck-shaft angle < 110 °
- aftercare
- hip-spica or abduction pillow x 4-6 weeks depending on fixation and healing.
Indications for surgical intervention are :
- Neck–shaft angle < 90 degrees
- Progressive deformity.
- Vertical physis and a significant limb length discrepancy
- HE angle> 60 degrees
Summary
Coxa vara is a hip deformity characterized by a decrease in the angle between the femoral neck and the shaft of the femur. It can be congenital or acquired. Symptoms may include a shortened leg, limping, hip or groin pain, limited range of motion, and gait abnormalities. Diagnosis involves a medical history review, physical examination, and imaging studies such as X-rays.
Treatment options include observation, bracing, or surgery depending on the severity and underlying cause. Rehabilitation and physical therapy may also be part of the treatment plan. It’s important to consult with a healthcare professional for an accurate diagnosis and appropriate management.
FAQ
What is coxa vara caused by?
Congenital or developmental conditions are the two most frequent causes of coxa vara. Other frequent reasons include osteomyelitis, post-Perthes deformity, metabolic bone illnesses (such as Paget’s disease of the bone), and post-traumatic (caused by incorrect healing of a fracture between the greater and lesser trochanters).
What are the characteristics of coxa vara?
The following radiographic signs of coxa vara can be seen: a decreased femoral shaft angle, a tiny, flat femoral head in retroversion or diminished anteversion, a shallow and oval acetabulum, coxa brevis, and an extremely vertically oriented physeal plate.
How do you treat coxa vara?
Depending on the patient’s symptoms, the severity of the varus deformity, and the rate of angle advancement, the corrective valgus derotation osteotomy procedure may be nonoperative or surgical.
What is the difference between coxa vara and genu varum?
Hip: coxa vara, which causes a limp because the angle between the femur’s head and shaft is decreased.
The tibia is rotated inward in proportion to the femur in genu varum, which results in a bowlegged malformation. Genu means knee in Latin.
Is coxa vara congenital?
Yes, it can be Congenital Coxa vara or it can be due Acquired Coxa vara.
What are the different types of coxa vara?
Varus abnormalities of the proximal femur known as acquired forms of coxa vara appear as a result of metabolic, neoplastic, or traumatic diseases. This category comprises premature closure, proximal physeal damage, fibrous dysplasia, and ricketic coxa vara.
Is there a special test for coxa vara?
X-Ray, MRI (magnetic resonance imaging), & CT Scan (computed tomography) can all show coxa vara.






2 Comments