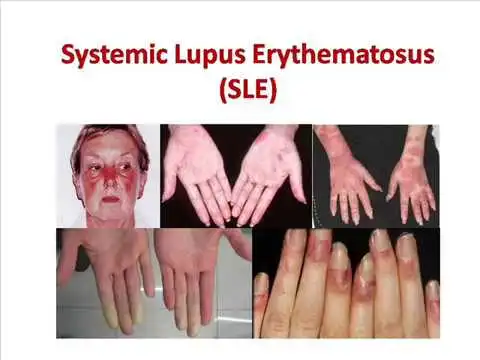
Systemic Lupus Erythematosus
What is Systemic Lupus Erythematosus?
Systemic lupus erythematosus (SLE), is the most familiar type of lupus condition. SLE is an autoimmune condition in which the immune system attacks its tissues, generating widespread inflammation and tissue injury in the involved organs. It can involve the joints, brain, skin, kidneys, lungs, and blood vessels. There is no treatment for lupus, but medical interventions and lifestyle modifications can assist to prevent it.
The immune system generally fights off harmful infections and bacteria to maintain the body healthy. An autoimmune condition happens when the immune system strikes the body because it confuses it for something unfamiliar. There are numerous autoimmune conditions, involving systemic lupus erythematosus (SLE).
The word lupus has been used to specify the number of immune conditions that have identical clinical manifestations and laboratory elements, but SLE is the most familiar type of lupus. The patient is frequently referring to SLE when they tell lupus.
Systemic lupus erythematosus – (SLE) is a chronic condition that can have stages of worsening symptoms that alternate with a duration of mild symptoms. Most patients with Systemic lupus erythematosus – SLE can live a routine life with therapy.
According to the Lupus Foundation of America, at least 1.5 million people are living with interpreted lupus. The foundation thinks that the number of patients who have the disease is much higher and that many patients go undiagnosed.
Epidemiology
There is a strong female preference in grown-ups, with females involved 9-13 times more than men. In kids, this balance is reversed, and men are involved two to three times more frequently.
Can involve any age group – the peak age at the start about the 2nd to 4th decades, with 65% of a person showing between the ages of 16 and 65 years (ie. during childbearing years).
The condition is more familiar in childbearing age in females yet it has been well documented in pediatric and senior people. SLE is more extreme in kids while in the aged, it manages to be a more insidious beginning and has more pulmonary involvement and serositis and less Raynaud’s, nephritis, malar rash, and neuropsychiatric difficulties
Analyses have shown that although rare, lupus in males grows to be more extreme.
Prevalence differs according to nationality with ratios as increased as 1:500 to 1:1000 in Afro-Caribbeans and indigenous Australians, down to 1:2000 in Caucasians.
Symptoms of SLE
The symptoms of lupus differ from patient to patient and can vary from mild to severe. You may have only a few symptoms involving only one region of your body, or you could have many symptoms throughout your body. Symptoms may arrive and go, and you may create new symptoms over time. Some symptoms occur when the condition generates inflammation in organs, like the joints, kidneys, skin, brain, lining of the heart and lungs, and blood cells. Symptoms of lupus can contain:
Arthritis generates painful and swollen joints and morning immobility.
Fevers.
Fatigue or feeling tired frequently.
A rash that occurs on the face across the nose and cheeks; this is known as a malar or butterfly rash
Round scaly rashes can occur anywhere on the body.
Sensitivity to the sun may generate a rash.
Hair loss.
Sores, which are generally painless, in the nose and mouth (most frequently on the top of the mouth).
Modification of color in the fingers and toes blue-purplish, white, or red from cold and tension (Raynaud phenomenon).
Swollen glands.
Swelling in the legs or near the eyes.
Pain when breathing deeply or lying down, from inflammation of the lining near the lungs or heart.
Headaches, depression, dizziness, confusion, or seizures.
Abdominal pain.
Lupus generates inflammation throughout the body, which can generate issues in organs, involving:
Kidney injury can lead to modifications in kidney function, involving kidney failure. This is known as lupus nephritis.
Seizures and memory issues due to modifications in the brain and central nervous system.
Heart issues:
Heart valve injury due to inflammation that conducts to scarring.
Inflammation of the lining near the heart muscle is known as pericarditis.
Inflammation of the heart muscle is also known as myocarditis
Inflammation of blood vessels, known as vasculitis.
Blood clots due to high levels of specific autoantibodies are referred to as antiphospholipid antibodies.
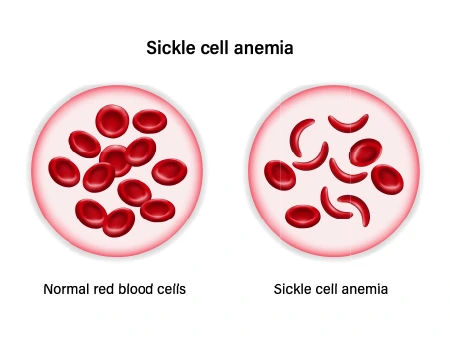
Low blood cell counts involve red blood cells, white blood cells, and platelets.
Inflammation of the tissue that covers the lungs, produces it painful to breathe. This is known as pleurisy.
Some patients with lupus may be more probable to develop further conditions, like cardiovascular conditions due to inflammation of the heart and blood vessel tissues generated by lupus, which can lead to:
Atherosclerosis occurs when fat and further materials connect to the blood vessel wall and build plaque. This can occur in blood vessels throughout the body.
Coronary artery condition occurs when plaque creates in the arteries that deliver blood to the heart. This can interrupt blood flow when a blood clot formations or a piece of plaque breaks off, generating a heart attack.
Causes of SLE
The actual cause of SLE isn’t known, but several aspects have been associated with the condition.
Genetics
The condition isn’t connected to a specific gene, but patients with lupus frequently have family fellows with different autoimmune diseases.
Environment
Environmental triggers can contain:
- ultraviolet rays
- specific medications
- viruses
- physical or emotional stress
- trauma
Sex and hormones
Systemic lupus erythematosus – SLE involves females more than males. The female also may feel more extreme symptoms during pregnancy and with their menstrual times. Both of these remarks have led some medical experts to think that the female hormone estrogen may play a function in generating SLE. Yet, more analysis is still required to confirm this theory.
Associated Co-morbidities
Contain:
- Fibromyalgia
- Atherosclerosis
- Lupus Nephritis- conducts to End Stage Renal Disease (ESRD)
- Anemia
- Some varieties of cancers (particularly non-Hodgkin’s lymphoma and lung cancer)
- Infections
- Hypertension
- Dyslipidemia
- Diabetes Mellitus
- Osteoporosis
- Avascular Necrosis
How is SLE diagnosed?
Your doctor or physician will do a physical examination to study for typical signs and symptoms of lupus, involving:
sun sensitivity rashes, like a butterfly or malar rash
mucous membrane ulcers, which may happen in the mouth or nose
arthritis, which is swelling or tenderness of the little joints of the hands, knees, feet, and wrists
hair loss
hair thinning
symptoms of cardiac or lung involvement, like rubs, murmurs, or uneven heartbeats
No single examination is diagnostic for SLE, but screenings that can assist your doctor to arrive at an informed diagnosis contain:
blood examinations, like antibody examinations and a complete blood count
a urinalysis
a chest X-ray
Your doctor or physician might guide you to a rheumatologist, which is a doctor or physician who specializes in managing joint and soft tissue diseases and autoimmune conditions.
Treatment for Systemic Lupus Erythematosus
The purpose of treatment in SLE is to control organ injury and conduct remission. The selection of treatment is dictated by the organ system/systems affected and the severity of involvement and varies from minimal therapy (NSAIDs, antimalarials) to intensive therapy (cytotoxic medicines, corticosteroids).
Person education, physical and lifestyle criteria, and emotional assets play a major role in the control of SLE.
A person with SLE should be sufficiently educated on the condition pathology, potential organ involvement involving brochures, and the significance of drug and monitoring compliance.
Stress decrease methods, exercises, adequate sleep hygiene, and use of emotional assets shall be promoted.
Smoking can aggravate SLE symptoms – educated regarding the significance of smoking cessation.
Dietary suggestions – Avoid alfalfa sprouts and echinacea and contain a diet wealthy in vitamin D.
Photoprotection is vital, and all people with SLE shall avoid direct sun disclosure by timing their activities properly, light-weight loose-fitting dark clothing wrapping the maximum part of the body, and using broad-spectrum (UV-A and UV-B) sunscreens with sun protector factor (SPF) of 30 or more
Maintenance therapy
The chronic condition should be managed with a lower dose of corticosteroids (eg, oral prednisone = 7.5 mg once a day or its equivalent) and further medications that prevent inflammation (eg, antimalarials, immunosuppressants [mycophenolate mofetil or azathioprine]) to sustain remission. Therapy should be directed by clinical characteristics mainly, although anti-dsDNA antibody titers or serum supplement levels may be observed, especially if they have correlated with condition activity in the past. Yet, anti-dsDNA antibody titers or serum additional levels may not parallel nonrenal illness flares. Further pertinent blood and urine examinations may be used to evaluate precise organ involvement.
Calcium, vitamin D, and bisphosphonate treatment should be evaluated in persons carrying corticosteroids long-term.
If a mixture of immunosuppressive treatment is used, persons should be offered prophylaxis for opportunistic infections, like Pneumocystis jirovecii, and vaccines against standard infections (eg, streptococcal influenza, pneumonia, COVID-19).
Physiotherapy treatment in Systemic Lupus Erythematosus
Exercise is useful for persons with SLE because it reduces their muscle weakness while simultaneously improving their muscle endurance. Physical therapists can play an essential role for a person with SLE during and between worsenings. The person’s requirements for physical therapy will differ significantly depending on the systems affected.
Education: Patients with skin lesions need to have proper education on the best method to care for their skin and to confirm they do not feel further skin breakdown.
Aerobic Exercise: One of the most familiar impairments that people with SLE feel is generalized fatigue that can restrict their movements throughout the day. Graded aerobic exercise schedules are more victorious than relaxation methods in reducing the fatigue levels of persons with SLE. Aerobic activity generates many with SLE to feel much sounder. The aerobic exercise schedule may consist of 30-50 minutes of aerobic exercise (walking/swimming/cycling) with a heart rate corresponding to 60% of the person’s peak oxygen consumption. Both aerobic activity and range of movement/muscle-strengthening activities can raise cardiovascular fitness, energy level, functional level, and muscle strength in a person with SLE (aerobic activity for 20-30 minutes at 70-80% of their highest heart rate,3 times a week for 50 minutes sessions).
Energy Conservation: Physical therapists can familiarize persons with proper energy conservation methods and the best ways to save joints that are susceptible to injury.
Further, physical therapists and persons with SLE should be mindful of signs and symptoms that indicate a progression of SLE involving those associated with kidney involvement, avascular necrosis, and neurological involvement.
Long-term complications of SLE
Over time, SLE can hurt or cause difficulties in systems throughout your body. Likely complications may contain:
- blood clots and vasculitis or inflammation of blood vessels
- inflammation of the heart, or pericarditis
- a heart attack
- a stroke
- memory changes
- behavioral changes
- seizures
- inflammation of lung tissue and the bordering of the lung, or pleuritis
- kidney inflammation
- decreased kidney function
- kidney failure
SLE can have severe negative consequences on your body during pregnancy. It can show pregnancy difficulties and even miscarriage. Speak with your doctor regarding ways to decrease the risk of difficulties.
Prognosis
Despite the advances in therapeutic choices for SLE and a better understanding of the conditioning process, SLE people suffer from considerable morbidity and maintain high mortality. Survival rates are 85 to 90% during the first ten years. Conducting reasons for mortality contain infections, cardiovascular conditions, and renal conditions. Early diagnosis with treatment to control organ damage, monitoring, and screening persons for cardiovascular conditions and infections with early intervention may enhance these results.
Poor prognostic elements in SLE contain African American ethnicity, renal condition (particularly diffuse proliferative glomerulonephritis), young age, male sex, more senior age at presentation, low socioeconomic status, hypertension, presence of antiphospholipid antibodies, antiphospholipid antibody syndrome, and high overall condition activity.
FAQ
Is lupus a very serious disease?
Lupus can affect many various regions of your body. It can generate aches and pains, as well as severe difficulties for your primary organs. Because lupus is an autoimmune condition, it generates your body to attack itself. This can guide to organ injury over time.
Can lupus go away?
Lupus is a chronic condition with no treatment. This indicates that you can control it with treatment, but it will not go out. Treatment can assist to enhance your symptoms, controlling flares, and controlling further health issues frequently caused by lupus. Your therapy will rely on your symptoms and requirements.
At what age does lupus start?
Symptoms and diagnosis happen most frequently between the ages of 15 and 44. Symptoms of lupus will happen before age 18 in only 15 percent of the patient who is later analyzed with the condition.
What happens if lupus is left untreated?
If gone untreated, it can place you at risk of creating life-threatening issues like a heart attack or stroke.
How can you avoid getting lupus?
Although lupus is not preventable, patients with lupus can carry actions to control their condition and control or minimize lupus flares: People with lupus need to take their drugs as referred by their healthcare providers or doctor.



3 Comments