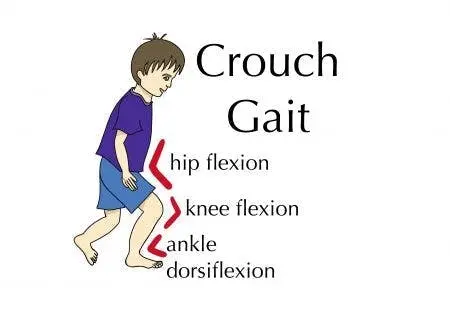
Crouch Gait
Introduction
Excessive dorsiflexion or calcaneus at the ankle combined with excessive flexion at the knee and hip is known as crouch gait. The majority of children with spastic quadriplegia and children with more severe diplegia exhibit this pattern as part of the normal course of gait problem.
Unfortunately, in younger children with spastic diplegia, solitary extension of the heel cord is the most typical cause of crouch gait. Hip and knee flexion will rise quickly after the heel cord has been extended if the spasticity/contracture of the hamstrings and iliopsoas has not been identified and appropriately addressed. An ugly, energy-draining gait pattern is the end outcome, which is followed by anterior joint pain and patellar pathology in youth.
It is typically necessary to extend the hamstrings and iliopsoas, use a ground response AFO, and stabilize the foot in order to adequately repair bone issues such as medial femoral torsion and lateral tibial torsion while managing the crouch gait.
The musculoskeletal disease is typically too far along by the time it is recognized to react to intramuscular BTX-A.
Long-term usage of a ground reaction (Saltiel) AFO for orthotic care is recommended until the plantar flexion knee extension couple’s integrity is demonstrably restored.
Crouch Gait Causes in People with Cerebral Palsy
An unusual walking pattern called crouch gait is characterized by:
- Ankle dorsiflexion, or twisting of the ankles both upward
- Bent knees (knee flexion)
- Bent hips (hip flexion)
The term “crouch gait” refers to the way this stance makes it look as though the person is walking somewhat crouched.
The main reason for crouch gait is spasticity, which is an involuntary muscular contraction. Ineffective communication between the brain and muscles leads to spasticity. The effect is that the muscles stay tightened for extended amounts of time.
Brain injury sustained during development is the cause of spastic cerebral palsy. The youngster may have stiffness in different parts of the body, depending on where the brain injury is. The cerebral palsy that results does not worsen with time, but the stiffness that follows can. The afflicted muscles stay tensed because the brain is unable to send a signal for them to relax.
As a result, children with stiffness in their legs may develop unnatural gait patterns like the crouch gait as they start to walk.
We’ll talk about the dangers of improperly handling crouch gait in the section that follows.
Risks Associated with Poorly Managed Crouch Gait
It takes more effort to walk with a crouch gait than to walk normally, which frequently results in weariness and joint pain.
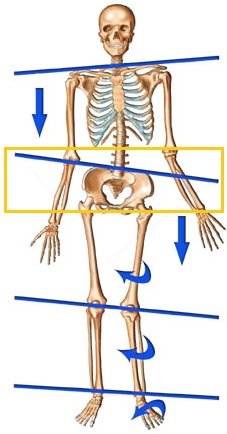
The body has to work harder to maintain equilibrium since the muscles, joints, and bones are put under more stress. Additionally, several muscles are continually underutilized as a result of the ankles, knees, and hips’ persistent contraction. In addition to increasing joint pressure, this muscle imbalance frequently causes persistent discomfort.
People may experience further issues if their leg spasticity is not well managed, such as:
- Uneven or distorted growth
- Weakening of the ankle plantar flexors, hip and knee extensors
- Sub-luxated or dislocated joints
- Inability to walk
- Compromised posture and stability
Now that you know why it’s important to regulate crouch gait, let’s talk about whether it can be fixed.
Treatment in summary for CP child and elderly
Non-operative
Physical therapy
Indications
- Has a significant impact on patients receiving both surgical and non-surgical treatment.
- Chemodenervation (botulinum neurotoxin A) may be utilized as a main therapeutic option or to temporize certain muscle groups in order to postpone surgical treatments.
- Hamstring spasticity in an ambulatory patient without a permanent deformity
Orthosis
- Solid ankle foot orthosis (AFO)
- Indications
- Equinus malformations that may bend
- The subtalar neutral posture can be maintained as the ankle is passively corrected to neutral.
Posterior leaf-spring (or hinged) orthoses
- Indications
- Used in the presence of excessive ankle plantar flexion in the swing phase
Operative
- single-event, multi-level surgery (SEMLS)
Overview
- The SEMLS technique, which aims to correct all primary (spasticity) and secondary (i.e., contractures) abnormalities at several levels during a single surgery, has emerged as the gold standard for CP gait surgery.
- To prevent an iatrogenic deterioration of gait, it is imperative to correct various distortions simultaneously.
- Methods carried out in the event of increasing femoral anteversion-related SEMLS lever arm dysfunction: turn outside the body Hip flexion contracture caused by proximal femur osteotomy and knee contractures caused by intramuscular psoas lengthening
- Lengthening of the medial hamstrings (lateral may result in excessive weakness) minor fixed contracture is present
- Directed expansion
- For stiff knee gait equinus, distal femur extension osteotomy rectus transfer: gastrocnemius retraction or tendo-achilles lengthening flatfoot repair rehabilitation
With the exception of a year for recuperation, AFOs and vigorous physical therapy for retraining and strengthening after releases are crucial parts of the SEMLS strategy.
Techniques
- External rotation proximal femur osteotomy
- Indications
- Femoral anteversion/hip internal rotation deviation
- Rectus Transfer
- Indications
- Stiff knee gait
- Technique
- Transferring it posterior to the center of rotation of the knee will result in a knee flexion vector with rectus activation.
Hamstring extension in the medial
- Indications
- Typically younger individuals with less than 5 degrees of knee flexion deformity method for minor knee dysfunction
- Technique
- The best outcome is fractional lengthening at the myotendinous junction.
- Complications
- Recurrence of hamstring contractures is common, particularly with jump gait
Guided surgery for growth
- Indications
- knee flexion abnormalities ranging from 10 to 25 degrees in patients who still have at least two years of growth left in them Superior femur extension osteotomy +/- shortening or advancement of the patellar tendon
- Indications
- For abnormalities of knee flexion ranging from 10 to 30 degrees, with substantial quadriceps lag near or at skeletal maturity
The gastrocnemius retracts
- Indications
Silfverskiöld test positive
- Technique
- Identification and protection of the sural nerve (superficial to fascia) by use of a horizontal or vertical incision made at the level of the stomach myotendinous junction
- cut all deeper bands that restrict the release of contracture (tiny raphes may be present in the tendon) and precisely split the tendon alone, protecting the muscle fibers that haven’t yet joined the tendon.
- 10 degrees of dorsiflexion is the target range for therapy.
Extension of the Tendo-Achilles
- Indications
- Ankle rigid abnormalities cannot be passively corrected to a neutral position.
- True equines
- Silfverskiöld negative
- Contraindications
- Spastic diplegia
- This causes the calcaneus to become excessively weak and the crouch gait to develop.
- Techniques
- To prevent over-lengthening, execute a Z-lengthening or many hemi-lengthenings.
How to deal with crouch gait in people who have Cerebral Palsy
People with cerebral palsy must address spasticity, the underlying cause of crouch gait, in order to improve it.
Generally speaking, it will be simpler to repair an aberrant gait pattern the earlier it is discovered.
We’ll discuss a number of therapies that might be used to address crouch gait below.
Orthotic Devices
Even if it means your child walks more slowly or diligently while learning to improve crouch gait, it’s important to correct improper form and placement.
In addition to gently stretching spastic muscles, orthotic devices like braces and splints offer structural support to encourage appropriate musculoskeletal alignment. and stop further contractions.
In an ideal scenario, people are able to progressively wean off of the usage of their orthotic devices until they are no longer required as their brains and bodies adjust to walking using the corrected gait pattern.
Botox
A drug called Botox is injected into spastic muscles to temporarily relax them. It suppresses the excessive nerve messages that activate muscles.
Botox’s side effects provide people with a little window of time to practice walking correctly. Although its benefits do wear off over time, the advantages of regularly using the right form when walking can endure long after the drug has gone off.
Intrathecal Baclofen Pump
A steady dose of baclofen can enter the fluid around the spinal cord thanks to surgery to implant a baclofen pump beneath the skin of the abdomen.
Similar to Botox, Baclofen is a muscle relaxant that reduces excessive muscular tone. As opposed to taking the medication orally, you don’t require as high of a dosage because it is injected straight into the cerebrospinal fluid. Baclofen pumps may not be the best course of therapy for kids since they require frequent refills.
Selective Dorsal Rhizotomy
A surgical technique called selective dorsal rhizotomy involves chopping off hyperactive sensory nerve fibers on purpose. Reducing the amount of information that the brain receives from the muscles can greatly lessen spasticity.
Single-Event Multi-Level Surgery (SEMLS)
The most invasive spasticity operation is called SEMLS. From the hips to the feet, each muscle imbalance and bone abnormality is surgically addressed separately throughout the course of the process.
Tendon lengthening, muscle movement, and bone alteration are all possible SEMLs. Without directly affecting the central nervous system, spasticity can be greatly reduced by correcting the alignment of the musculoskeletal system.
Physical Therapy
Finally, and perhaps most significantly, addressing aberrant gait patterns like crouch gait requires extensive physical treatment.
Your child has to engage in rigorous physical training to improve their gait, regardless of whether they use a brace, Botox, or surgery to manage their spasticity.
To encourage neuroplasticity in the brain and replace the preexisting walking pattern, physical therapy activities need to be hard and repeated. It’s also crucial to keep up with home workouts to reinforce abilities acquired during therapy.
Summary
There isn’t a single orthosis or therapy that can be used to increase mobility and walking. AFOs may improve walking stability and comfort but may not stop abnormalities and contractures. In cases when there is contracture of the adductors of the legs, operations may be required to facilitate parent care or to enhance functionality (such as standing and walking).
Before making judgments on the use of orthoses and operation medicine, a thorough assessment is required. The efficacy of surgeries and AFOs is still mostly unknown.
FAQs
What is a crouch gait?
Review’s objective: Excessive ankle dorsiflexion, knee flexion, and hip flexion during the stance phase are characteristics of the crouch gait. Those with cerebral palsy frequently have this type of gait abnormality.
What are the characteristics of crouch gait?
One of the most prevalent gait abnormalities in individuals with cerebral palsy (CP) is the crouch gait pattern (CGP), which is characterized by greater knee flexion during the stance phase and commonly increased hip flexion and internal rotation. These kids’ ankle joints may exhibit various kinematic patterns.
What is a crouch gait in adults?
One of the most prevalent gait abnormalities, crouch gait (CG), is seen in individuals with cerebral palsy. Hip, knee, and ankle flexion that is excessive are primarily defining characteristics.
What muscles are weak in crouch gait?
It may be difficult for people with a crouch gait to adopt an upright gait pattern if their ankle plantar flexors and hip abductors are weak. These muscle groups may be essential goals for strength training regimens.
What is another name for crouch gait?
Pathological gait patterns are frequent and include the crouch gait (also known as the crouching or flexed knee gait). Although there are several classifications according to experts and research, crouching is typically identified by an excessively flexed knee during the stance phase of locomotion.
References
- Classification of Gait Patterns in Cerebral Palsy. Physiopedia. https://www.physio-pedia.com/Classification_of_Gait_Patterns_in_Cerebral_Palsy
- Cerebral Palsy – Gait Disorders – Pediatrics – Orthobullets. https://www.orthobullets.com/pediatrics/4128/cerebral-palsy–gait-disorders
- What Crouch Gait Appearances Like as well as How to Deal with Cerebral Palsy Flint Rehab. https://www.flintrehab.com/crouch-gait-cerebral-palsy/