Crush Injury
Explanation of a crush injury
An object can injure someone by compressing their body, which is known as a crush injury. In everyday civilian life, this kind of damage is uncommon, yet it happens frequently after a natural disaster. Other factors include terrorist attacks, industrial accidents, car accidents, building collapses, heavy machinery mishaps, and traffic collisions.
Terminology definitions
The spectrum of all kind of crush injuries with other injuries consists of:
Crush injury
- Injury resulting from the direct physical crushing of the muscles by something heavy is known as a “crush injury.”
- The physical damage caused by prolonged compression of the torso, a limb or limbs, or other body components is known as a crush injury. The major immediate outcome of the trauma or ischemia brought on by compression may be to blame for the resulting trauma to the soft tissues, muscles, and nerves.
- After the release of the compressive force, severe crush injuries may result in edema in the affected regions, as well as probable muscular necrosis and neurological dysfunction, in addition to any potential direct muscle or organ injury. Additionally, a secondary injury from subsequent compartment syndrome may be the cause of this soft tissue damage.
- Patients who have been immobilized for an extended duration while inebriated or under anesthesia are examples of nontraumatic occurrences of crush damage.
One extremity may cross another, generating local pressure, or the afflicted muscle compartment may be the one that is resting on a hard surface. Crush syndrome may result from gluteal compartment syndrome, which has been observed in postoperative, drunk, and comatose patients who have been immobilized for a long time. This is especially true because presentation or detection is usually delayed. There are also more factors that might lead to nontraumatic crush syndrome, such as ischemic, metabolic, toxicologic, and oncologic causes of rhabdomyolysis.
Crush syndrome
- The term “crush syndrome” refers to the systemic symptoms that follow a crush injury and can cause organ damage (most commonly acute kidney injury [AKI], but multisystem organ injury can also happen), organ failure, or even death. Crush syndrome symptoms include rhabdomyolysis, which is a major cause of AKI and one of the systemic effects of muscular damage.
- Other circumstances when the tissues are compressed can also result in crush syndrome. For instance, burns, electrical injuries, and extended immobilization are all risk factors for crush syndrome. The second most common cause of mortality during earthquakes is crush syndrome, behind direct damage.
- An injury to the skeletal muscles that is severe enough to compromise cellular integrity and induce the discharge of its contents into the bloodstream is known as rhabdomyolysis and is associated with several metabolic abnormalities.
Compression syndrome
- An indirect muscular injury caused by the gradual, simple compression of a set of muscles that results in ischemic damage and permits the blood to get contaminated by crushed chemicals.
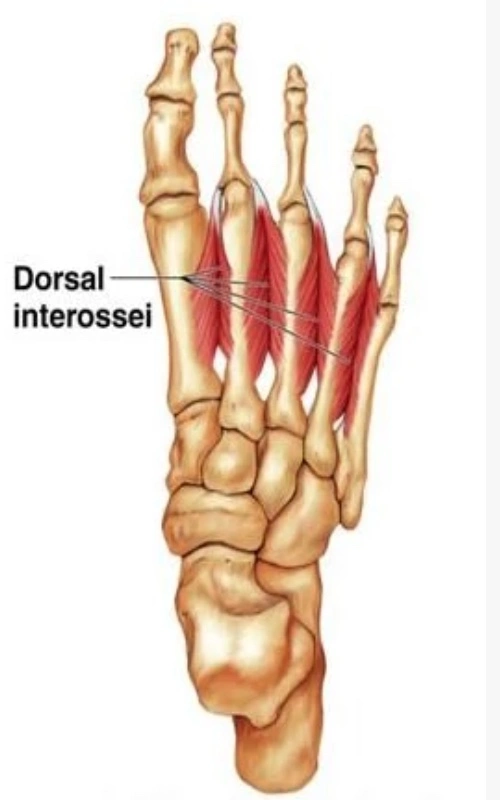
Compartment syndrome
- A localized, fast rise in muscular tension invariably results in metabolic abnormalities similar to rhabdomyolysis.
Injury mechanism
Crush injuries sometimes result from being trapped beneath a car or from industrial, construction, or agricultural incidents. 3 to 20% of mass casualties in natural catastrophes such as severe earthquakes may include crush injuries from building collapse and entrapment. Both acute asphyxia and crush injuries can result from large-scale mob stampedes.
While occluding venous outflow, the compressive force directly damages surrounding tissue. Crush syndrome may develop from prolonged compression-associated cellular death, particularly myonecrosis. The term “smiling death” refers to the clinical deterioration that can happen within 20 minutes following extrication, including death. After being freed and saved, the sufferer smiles before abruptly going into cardiac fibrillation due to the outflow of potassium, phosphorus, and myoglobin from the sites of damage. Renal failure-related delayed consequences and mortality have been well-documented in patients rescued from quake-damaged buildings and during the 1941 London Blitz bombings.
Only industrial safety laws, building rules, and injury prevention initiatives may be able to avoid crush injuries in their first stages. With quick therapy at the scene of the injury and continued through field care, prehospital transport, and basic hospital care, secondary prevention of crush syndrome may be possible after a crush injury has occurred.
Pathophysiology
As a result of skeletal muscle damage, disintegration, and subsequent cell content release, crush syndrome develops throughout the body. The length, scope, and mass of the injured muscle, as well as the severity of the crush syndrome, are all factors. Both short-term, high-magnitude traumas (like being crushed by a skyscraper) and long-term, low-magnitude injuries (like a coma or drug-induced immobility) can cause it.
According to data, severe head injuries or asphyxia cause up to 80% of crush injury sufferers to pass away. 10% of the 20% who are hospitalized recover without incident. 10% of people develop crush syndrome. Our whole attention must be directed towards treating this 10%, which has severe and frequently occurring metabolic abnormalities.
Myoglobin is released from crushed and ruptured muscle cells, where it is changed to metmyoglobin and then acid haematin, which is then discharged into the bloodstream. Additionally, potassium, magnesium, phosphate, acids, and enzymes including lactate dehydrogenase (LDH) and creatine phosphokinase (CKMM) are found in muscles. Even though they are necessary for cell function, when released into the bloodstream in high quantities, they are poisonous.
The release of sodium, calcium, and fluids during regional ischemia, which is brought on by blockage of the micro- and macro-circulation to the muscles after crushing, increases muscle volume and tension. Exhaustion of CK and ATP. Muscle vaso-dilatation and hypotension exacerbation are both aided by the Nitric Oxide System being activated.
Because reperfusion to the ischemic injured muscles alters the sodium-potassium-ATPase system after tissue tension is relieved, casualties don’t start to degrade until they are freed from the debris of collapse or entrapment. Consequently, myoglobin breakdown products, lactic acid, uric acid, and muscle enzymes like creatinine phosphokinase and aldolase are released into the bloodstream together with ions like calcium, potassium, and phosphate.
Renal mechanism affection
Although myoglobin is removed by the glomerulus, it precipitates in the distal convoluted tubules and causes blockage once the renal threshold is reached. Edematous and enlarged kidneys are another common condition. The circulation of potassium that has been released changes the rhythm of the heart. Finally, due to lung edema, patients experience shock that affects respiratory gas exchange. It is an ideal environment for ARDS.
The occurrence, persistence, and seriousness of oliguria as well as kidney impairment are unrelated to the degree of muscle damage. Massively bloated, rigid, cold, insensitive, and necrotic describe the muscles.
After head and chest traumas, crush injuries are uncommon since the extended pressure required to create this condition frequently ends in fatalities. Since most of these individuals are aware when they are saved, chest injuries are usually not too serious. However, research indicates that up to 10% of crush injuries are related to chest trauma.
Clinical characteristics
Casualties are common during rescue operations, but shock immediately sets in. It is common to observe petechiae, blisters, muscular bruises, and superficial wounds.
Myalgia, paralysis of the muscles, and sensory impairment are frequent. The sequence of events includes fever, cardiac arrhythmia, pneumonia, ‘tea or cola’ coloured urine, oliguria, and renal failure. In patients who need delayed rescue, nausea, vomiting, agitation, and delirium are common.
Investigations
Crush syndrome is often assumed to exist when serum creatinine kinase (CKMM) levels are more than 1000 IU/l and there are accompanying clinical symptoms. The typical range is 25–175 U/l, which typically increases 2–12 hours after a crush, peaks in 1–3 days, and then starts to fall after 3–5 days.
Highly sensitive tests include those that measure serum myoglobin and its breakdown products; those that measure serum lactic acid, AST, ALT, and LDH show a steady rise; those that measure serum uric acid may notice a moderate rise; those that measure serum urea and creatinine may notice a steep rise, particularly after a protracted crush; and those that measure serum potassium may indicate the need for dialysis. These are just a few of the other investigations that may be helpful.
There may be hypocalcemia and hyperglycemia brought on by stress. The presence of myoglobin products in urine may be detected by RE. ECG, haemogram, and blood gas analyses are also beneficial. Since it is well acknowledged that intracompartmental pressures more than 30 mm Hg indicate the necessity for a fasciotomy, intracompartmental pressure monitoring is helpful. To check for limb ischemia, Doppler investigations are performed, and the body weight is noted.
Complications
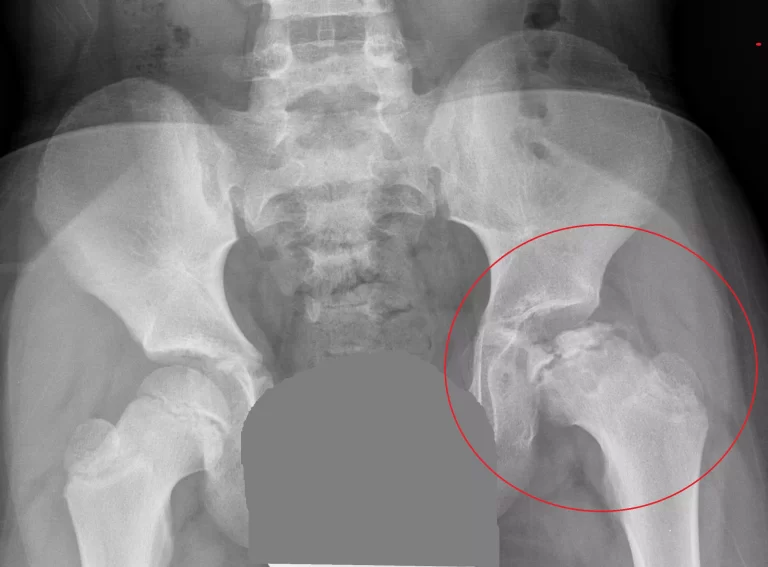
Hypovolemic shock
Severe hypovolemia can result directly from the loss of plasma volume via damaged capillary walls and cell membranes. Myocardial depression caused by the release of intracellular electrolytes might result in shock. Blood loss from pelvic or long bone fractures may also co-exist due to the mechanism of injury.
A considerable amount of potassium, a cation that is primarily intracellular and can cause cardiac arrest, can be released when cell membranes are disrupted. Hyperkalemia and electrolyte imbalance can also follow. The breakdown of clotting mechanisms and shock may intensify as a result of the sequestration of plasma calcium into wounded tissue, which can result in relative hypocalcemia. Hypoperfusion due to shock and reperfusion damage can also cause metabolic acidosis.
A common side effect of crush injury is compartment syndrome, which is brought on by bleeding, edematous tissue damage, and fluid redistribution into the intracellular compartment. Systemic crush syndrome and irreversible muscle cell loss may be caused by compartment syndrome that has already developed.
Traumatic asphyxia
A severe chest crush injury from a stampede or heavy item can cause traumatic asphyxia. This can cause a capillary rupture in the head and neck due to the substantial rise in thoracic pressure and pressure within the superior vena cava; this increased pressure in addition to efforts at inspiration against a closed glottis can cause this. The typical symptoms include petechial eruptions on the face, neck, and torso above the area where the item was crushing the sufferer, cervicofacial cyanosis, edema, and subconjunctival haemorrhage.
Because hypoxia can be fatal if it lasts more than a few minutes, this injury usually appears only after a brief period of crushing pressure. Traumatic hypoxia has been reported in instances of stampedes during sporting, musical, religious, and political gatherings. Additionally, trampled victims frequently sustain fractures and musculoskeletal problems. Traumatic asphyxia can occur in conjunction with rib fractures, lung contusions, liver and spleen lacerations, and anoxic brain damage.
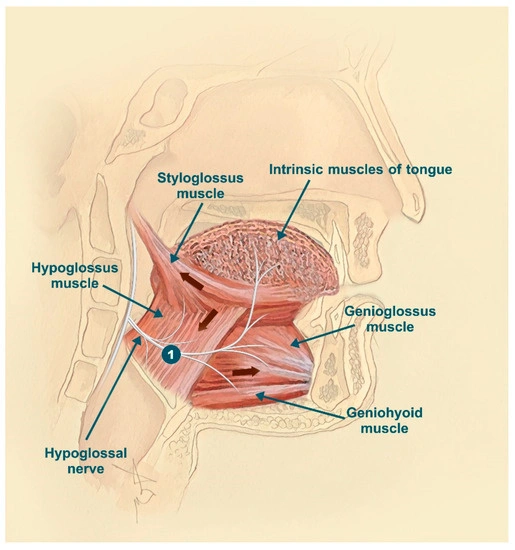
Extremity crush injury
Open fractures, mangled extremities with ischemia, blisters, purpura, and generalised edoema and erythema are all examples of clinical presentations of an extremity crush injury. It is important to be aware of the possibility for these individuals to develop acute compartment syndrome and rhabdomyolysis in addition to managing the usual orthopaedic and vascular complications related to this kind of injury.
These can happen as a consequence of a protracted hypoperfused condition that causes an ischemia-reperfusion damage that can cause swelling, acute compartment syndrome, and rhabdomyolysis, or they can happen as a result of direct trauma that causes tissue swelling due to crushing, or both of these things. Long-term compression can cause muscular necrosis and rhabdomyolysis by resulting in cell death. This has been linked to crush syndrome, compartment syndrome, and systemic signs of tissue injury. Long-term major artery compression can also cause intimal damage and thrombosis, which aggravates distal ischemia.
Organ injury
In addition to rib fractures, pelvic fractures, hemo-thoraxes, pneumo-thoraxes, and other blunt solid and hollow viscus injuries, blunt thoracic or abdominal traumas can also cause cardiac contusion, pulmonary contusion, and hollow or solid viscus injuries. Even spinal cord damage without a fracture has been linked to persistent compression. A concomitant penetrating injury from projectiles might exacerbate blunt injury from crush mechanisms.
Severe renal damage
A considerable percentage of acute kidney damage, believed to be up to 15%, is caused by the release of myoglobin by injured muscle, which results in rhabdomyolysis and shock. Acute renal damage causes a markedly greater death rate.
Renal replacement treatment and high-intensity intravenous fluid administration are no longer necessary if acute kidney damage has been confirmed. The typical indicators of volume overload, hyperkalemia, severe acidemia, and uremia are used to start hemodialysis. Hemodialysis may be necessary twice a day or more to treat hyperkalemia after a crush injury due to its potential for a very quick and severe start.
Management of severe crush injury in hospital
Initial trauma management
The Advanced Trauma Life Support programme describes the initial management of trauma patients in the emergency room.
Continue administering isotonic saline that was started in the field while closely watching urine output.
Ongoing trauma management – All the elements of care used for other trauma patients are included in the management of patients with crush injuries.
Clinical monitoring
Up to stabilization, many clinical examinations and laboratory tests should be done daily.
These include arterial blood gases with lactate and/or base deficiency, creatinine, and electrolytes (especially serum sodium, potassium, and bicarbonate). Upon admission, a urinary bladder catheter should be inserted to closely monitor urine output.
Patients who have a history of crush damage that is either overt or suggestive should have their blood pressure and electrolytes (especially potassium, calcium, and phosphate) as well as arterial blood gas measured. Rhabdomyolysis can be identified by urine myoglobin and creatine kinase tests.
Mangled extremities
Some extremity crush injuries are so serious that the survivability of the afflicted limb is in doubt. Amputation rates range from 3 to 59 percent, depending on extrication times, injuries sustained, and available resources.
According to recommendations, amputation should only be performed in situations when a limb cannot be saved or when damage to the limb is the cause of sepsis, systemic inflammation, or excessive bleeding. The choice of whether to save a limb is a clinical one; rating systems like the mangled extremity severity score (MESS) have not been demonstrated to be predictive and perform worse than the expertise of skilled surgeons. Amputation may be more likely to be required in a mass casualty scenario where the resources, such as blood transfusion, required to try limb salvage may not be sufficient.
Acute extremities compartment syndrome has a recognized cause: a severe crush injury. The risk of crush syndrome and limb loss is lower with early compartment syndrome diagnosis, examination, and treatment. In the vast majority of scenarios, fasciotomy to completely decompress all affected compartments is the only effective therapy for established extremities compartment syndrome.
Fasciotomy delays result in higher morbidity, which might lead to the necessity for amputation. Separate reviews are given of the clinical characteristics of acute extremity compartment syndrome and fasciotomy, including the distinction between the upper and lower limbs.
The use of preventive fasciotomy in cases of severe crush injuries is debatable. In a level 1 trauma centre, where the author has worked, we don’t do preventive fasciotomies for severe crush injuries. Only when established acute compartment syndrome is clinically evident at the time of admission or when measured compartment pressures show a difference between the diastolic blood pressure and the compartment pressure (delta pressure) of 30 mmHg or less, do we normally conduct fasciotomies.
Support from the psychosocial community
Psychological trauma is a part of crush damage. Healthcare professionals, unharmed victims, family members, and other carers may also feel shocked, sadness, and subsequently depression and post-traumatic stress disorder. Disaster survivors, first responders, and medical professionals all run the risk of committing suicide. Plans for providing emotional, psychological, psychiatric, and social assistance to everyone in need should be part of disaster response preparation.
Treatment
Early fluid resuscitation lessens the possibility of renal failure, lessens the severity of hyperkalemia, and can enhance recovery from isolated crush injuries.
We are concerned with rescue, resuscitation, identification of the syndrome, treatment, and rehabilitation in the case of crush injuries. Rescue operations need to be well-coordinated, and patients should be sent to dialysis clinics for greater levels of treatment.
Some professionals advise using potassium binders such oral polystyrene sulfonate before transit in addition to the standard military care procedures to prevent kidney injury. A prediction algorithm for calculating the risk of crush syndrome has been attempted by Noriaki et al.
The optimal place to start resuscitation is at the scene of the accident. A victim may lose litres of extracellular fluid into the wounded extremities while they are often in shock. In combat, a clear history is not always accessible, and the condition might sneak up on people who first seem well. The paramedical staff should be trained to recognise this disease and to aggressively use fluid therapy to treat it.
Radiologists, trauma surgeons, doctors, and biochemists work closely together to identify crush syndrome and treat it. Rehabilitation should be a long-term process that includes both physical and mental health care.
Large-volume crystalloid fluid resuscitation lessens the severity of and lowers the risk of acute renal impairment in victims with isolated crush injuries who are hemodynamically stable.
Monitoring and fluid replacement
Despite being an essential component of therapy, there is no established method. Fluid resuscitation must begin quickly, ideally within the first six hours, and ideally before the person is extricated. The amount of fluids injected varies significantly. More than 25 litres of saline have reportedly been given in a single day.
Of course, everyone agrees that saline should be administered as the fluid. Bicarbonate, lactate, or even oral citrate are necessary to combat metabolic acidosis. According to Gunal et al., 50 mmol of bicarbonate should be added to each lit of isotonic saline. The CVP, BP, lung condition and urine output are all closely monitored.
To lessen the sudden rise in blood potassium levels, an insulin glucose drip has been used. Blood transfusions are frequently required for patients with crush syndrome, and it is important to properly handle the logistical issues of collection, storage, and transportation.
Diuresis
The importance of preserving healthy kidney function as the cornerstone of our care of crush injuries must be emphasized. The urine output in patients with established crush syndrome should be at least 300 ml/hour, or at least 12 lit of fluid per day, as fluid sequestration inside injured muscles may reach 4 lit. This is largely accomplished by mannitol diuresis. However,
However, Mannitol is recommended in a compartment syndrome context, although according to Holt et al, it is not preferable to IV fluids alone.
In individuals with CK >5000 U/1, Brown demonstrated that bicarbonate and mannitol do not prevent renal failure. Except when necessary to provide a brief burst of renal function, loop diuretics should be avoided. One Japanese research attempted to use dopamine as the main treatment with mixed results, though this has the extra benefit of maintaining stable blood pressure.
Dialysis
It now clearly maintains a position in the treatment of crush syndrome. In the Armenian earthquake, where 23% of the victims needed dialysis, the Russians were incredibly successful. Therefore, it is crucial to have a nephrologist or at the very least a doctor on the team.
Anuria, fluid overload, serum creatinine levels, BUN, and bicarbonate levels are some of the key indicators for dialysis.
Potassium levels over 7 meq/1 are independent and significant dialysis predictors. For up to 15 days, dialysis may be required at least twice or perhaps three times every day. Patients who are at high risk for hyperkalemia may need preventative dialysis.
Hyperbaric oxygen
At high pressures, the plasma’s physically dissolved oxygen levels rise, tissue viability is improved, some vasoconstriction takes place, and as a result, the amount of fluid that leaves vascular compartments reduces, lowering tissue edema.
It immediately promotes fibroblast growth, which aids in wound healing. And conclusion, it can lessen the formation of anaerobic bacteria in necrosed muscles. The typical dosage is 2.5 atmospheres administered twice a day for a week at a time for roughly an hour and a half.
Numerous non-nephrotoxic, broad-spectrum antibiotics may be required.
- Surgery: Laparotomy and thoracotomy may be required. Debridement of all necrosed muscles is necessary, and this is followed by delayed primary or secondary suturing. Fasciotomy is necessary when there are indications that compartmental pressure may be increasing. Fasciotomies performed after 8–10 hours of crush have required amputations, hence early fasciotomies are preferable.
- According to Kantarci et al., a patient who requires a fasciotomy almost certainly needs renal replacement therapy. Fixing fractures is necessary, and conservative amputations may be necessary in both emergency and non-emergency situations. Tetanus vaccination is recommended. Reliable rehabilitation therapists are needed for late consequences of muscular contracture.
Summary
Hospital treatment for crush injuries resembles rhabdomyolysis in many ways. The surgical approach is similar to that taken in any incidence of trauma. Numerous limbs and lives will be saved by highly active fluid replacement, diuresis, fasciotomies, and monitoring of enzymes and electrolytes.
FAQs
What are the 5 P’s of a crush injury?
The five ‘p’s’ of pain, pallor, paraesthesia, pulselessness, and paralysis are commonly used to diagnose CS.
What is the first aid for a crushing injury?
Make an ambulance call. All crushing pressures should be removed from the victim as soon as it is safe to do so and is physically possible. A victim of a crush injury might not express any discomfort, and there might be no apparent signs of harm. Maintain the victim’s warmth and attend to any bleeding.
What can cause a crush injury?
When the body or part of it is pinned, wedged, or jammed under or between things, a crush injury happens. Depending on the intensity of the pressure, the skin, muscles, nerves, or bones may be damaged. If sufficient force is used, traumatic amputation happens.
What are the different types of crushing injuries?
Compartment syndrome (increased pressure in an arm or a leg that results in significant injury to muscles, nerves, blood vessels, and tissue) Bone fracture (fracture) (Open wound) Laceration nerve damage.
What is another name for a crush injury?
After a skeletal muscle is crushed, a condition known as crush syndrome, which is additionally referred to as traumatic rhabdomyolysis or Bywaters syndrome, emerges. It is followed by severe shock and renal failure.
What is the difference between crush injury and compartment syndrome?
Continual, sustained pressure on major muscles, such as those in the arms or legs, causes muscular breakdown, resulting in a crush injury. Any situation where a structure, such a nerve or a tendon, has been compressed into a space is known as compartment syndrome.





3 Comments