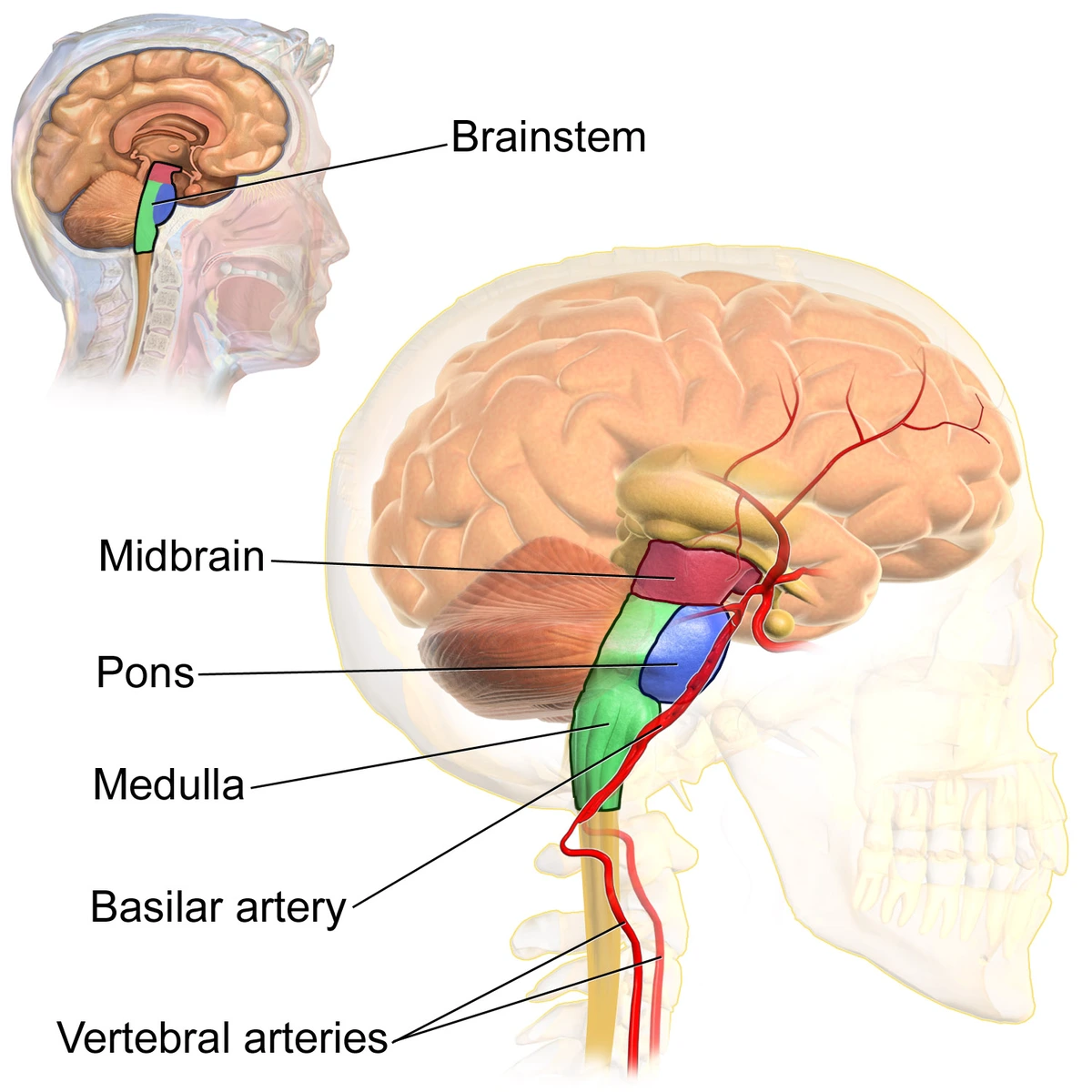
Basilar Artery Thrombosis
What is Basilar Artery Thrombosis?
Basilar artery thrombosis is a devastating stroke condition with a high morbidity and mortality rate. Its initial presentation is frequently nonspecific and may include dizziness or blurred vision.
Bilateral vertebral artery joint at the junction of the pons-medulla formed the Basilar artery. It delivers oxygen-rich blood to the brain’s brainstem, cerebellum, occipital, thalamus, and medial temporal lobes.
Epidemiology
Risk factors are equal to the known general risk factors for stroke. The most familiar is hypertension which is seen in as many as 70% of patients. Further risk factors contain coronary artery condition, diabetes mellitus, cigarette smoking, peripheral vascular condition, and hyperlipidemia.
The frequency, incidence, and majority are not well-known in medical publications. 20% of cerebral blood flow goes via the posterior circulation (vertebrobasilar system), it is analytical to understand why posterior circulation occlusions account for one-fifth of all strokes. Fortunately, basilar artery occlusions are thought to account for about only 1% of all strokes. Basilar artery occlusion has been noted in 2 out of 1000 post-mortem issues. Basilar artery thrombosis may define as many as 27% of ischemic strokes happening in the posterior circulation. A raised prevalence exists in men, with a 2:1 ratio. Occlusion due to an atherosclerotic condition is most prevalent in the person of advanced age, generally in the sixth and seventh decades of life. Distal basilar artery occlusion is generally secondary to embolism and is most dominant in the fourth decade of life.
Symptoms of Basilar Artery Thrombosis
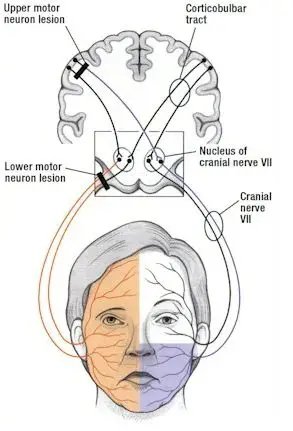
Most generally, persons experiencing basilar artery occlusion show acute neurologic signs involving:
- motor deficits
- hemiparesis or quadriparesisand facial palsies
- dizziness
- headache
- speech abnormalities
- particularly dysarthria
- a problem in articulating words
A person may also complain of:
- nausea
- vomiting
- changes in vision
An altered level of consciousness is generally present.
Basilar artery thrombosis may show in three general constellations:
Rapid beginning of advanced motor and bulbar symptoms with a reduced level of consciousness.
Insidious or stuttering symptoms over a rare day as a mixture of the above that end with incapacitating motor and bulbar symptoms, a reduced level of consciousness, or both. Prodromal symptoms may contain:
- headache
- neck pain
- loss of vision
- binocular diplopia
- dysarthria
- dizziness
- hemiparesis
- paresthesias
- ataxia tonic-clonic type motions
Herald hemiparesis is the phrase to define the momentary, unilateral weakness that may precede later permanent symptoms.
An abnormal level of consciousness and focal motor weakness are the hallmark symptoms displayed in the majority of people. Pupillary anomalies, oculomotor signs, and pseudobulbar representations (dysphonia, facial palsy, dysphagia, dysarthria, ) are noticed in more than 40% of people. Varying degrees of hemiparesis or quadriparesis is a region of the clinical image. As basilar artery thrombosis shows in different methods, it is essential to have high clinical suspicion to see it.
Cause of Basilar Artery Thrombosis
The cause can happen from:
- thromboembolism
- atherosclerotic disease
- vascular dissection
The mechanism varies depending on the involved segment. The atherosclerotic condition more generally involves the mid-portion of the basilar artery, observed by the vertebrobasilar junction. Lodging of an embolic source is much more regular in the distal third of the basilar artery, particularly at the top of the basilar artery and the vertebrobasilar junction. Arterial dissection is more familiar in the extracranial vertebral artery and has been associated with neck damage and cervical chiropractic adjustments. Intracranial dissections are extremely infrequent.
Differential Diagnosis
When regarding the diagnosis, it is essential to consider further etiologies that may generate equal overlapping symptoms. These contain:
- meningitisbasilar migraine
- cerebellar hemorrhage with brainstem compression
- cerebellar infarct
- hemorrhage with edema
space-occupying lesions in the posterior fossa involving metastatic condition, and supratentorial mass lesions with herniation, mass effect, and brainstem compression. Regard Todd’s paralysis, hypoglycemia, and conversion condition as likely mimics.
Diagnosis
The primary purposes of the evaluation are to verify the site of the vascular lesion and decide whether acute intervention is suggested to achieve recanalization in a time-sensitive way.
Laboratory analyses have restricted utility but may contain:
- complete blood count (CBC)
- electrolytes
- blood urea nitrogen (BUN)
- creatinine international normalized ratio (INR)
- prothrombin time (PT)
- activated partial thromboplastin time (aPTT)
Younger persons or patients without proof of atherosclerosis should be analyzed for the presence of procoagulant states. These contain:
- protein C
- protein S antithrombin III deficiencies
- lupus anticoagulant
- anticardiolipin antibodies
- homocysteine levels
An electrocardiogram enables screening for arrhythmias that may be representative of a thrombotic etiology.
Computed tomography (CT) scanning is generally the first imaging analysis conducted. CT may be useful for identifying larger regions of ischemic abuse and can emphasize hemorrhagic pathology. A hyperdense basilar artery may be current on the CT scan. Yet, CT scanning has a low sensitivity for early ischemia and is less useful at assessing the cerebellum, brainstem, and posterior circulation. Finally, one requires a high index of suspicion in the right clinical context to diagnose an easily missed condition. Additional evaluation with CT angiography may be viewed, and a filling fault reported within the basilar artery.
Catheter angiography is yet a measure for diagnosis, yet, with the availability of noninvasive imaging modalities like magnetic resonance imaging (MRI) and angiography (MRA), the function of angiography has altered. MRI/MRA is more susceptible than CT scanning for determining early ischemia and vascular occlusion. MRI is the most useful imaging modality for any posterior fossa lesion involving acute ischemic infarction.
Diffusion-weighted imaging (DWI) series can show an acute brainstem or cerebellar infarct within seconds of the arterial occlusion. MR angiogram can display the area of vascular occlusion non-invasively. The fact of microhemorrhages in GRE-T2* or SWI imaging can assist to show underlying hypertensive etiology.
Treatment of Basilar Artery Thrombosis
Acute occlusion of the basilar artery is mostly life-threatening. All persons should be permitted to a stroke unit when available. Recanalization of the basilar artery is key to the victorious therapy of basilar artery thrombosis and to enhancing prognosis. This can be performed by:
- systemic thrombolysis (IVT)
- intra-arterial thrombolysis (IAT)
- mechanical endovascular thrombectomy
Recanalization happens in more than half of basilar artery occlusion persons managed with IAT or IVT. Therapy is time-sensitive, the earlier the intervention, the better the functional outcomes. There is no good large-scale study to specify the therapy window for basilar thrombosis. It is much longer than the received window of 6 to 8 hours suggested for large vessel occlusion in anterior circulation infarct. The generally accepted time window is at least 12 hours and potentially up to 24 hours.
In some circumstances, if the person is having symptoms and minimal stroke on the MRI brain it is likely to think for mechanical endovascular thrombectomy for up to 2-3 days. Subsequent treatment for secondary prevention concentrates on managing the underlying reasons and altering risk factors.
Complications
Overall results can be predicted to be poor in a person with basilar artery thrombosis. Advances in pharmacologic and mechanical thrombosis and endovascular treatment may decrease mortality and disability rates. Catheter-directed thrombolysis and IV heparin also bring a risk of bleeding. There are many complications that affect a person’s life. Difficulties can contain the following:
- aspiration
- aspiration pneumonia
- thromboembolic condition (deep vein thrombosis and pulmonary embolism)
- myocardial infarction
- recurrent stroke
A person with progressive functional debility secondary to stroke is increasingly prone to pressure ulcers, contractures, and sepsis. Many persons who survive basilar artery thrombosis need ongoing physical and occupational therapy to recover and maintain functionality.
Prognosis
The person mortality rate is more significant than 85%, although it falls to as low as 40% in persons with recanalization. One can predict good functional results in as few as 24 to 35% of persons managed with intravenous or intra-arterial thrombolysis. For symptomatic persons who survive, the hazard of recurrent stroke is 10 to 15%. The most significant prognostic factors are the extent and time of thrombosis. Thus, a high index of suspicion of the diagnosis observed by expedited recanalization will provide the person with the best hope of an enhanced result.
FAQ
Can you recover from a basilar artery stroke?
A person can feel near-complete healing if therapy is provided promptly. Yet, the time from the beginning of symptoms to diagnosis in the emergency department is frequently very delayed in basilar artery occlusion, with one analysis informing an average total delay of 16 hours and eight minutes.
What is the survival rate of a basilar artery stroke?
Basilar artery occlusion has a dismal natural approach and the mortality rate is 85% to 95% even with anticoagulant and fibrinolytic treatment if the artery is not recanalized.
What region of the brain does the basilar artery supply?
The basilar artery is the major artery that delivers blood to the back part of your brain. It brings oxygen-rich blood to your brainstem, cerebellum, and occipital lobes. Several diseases, like blood clots or aneurysms, can interrupt blood flow in your brain.
Can the basilar artery be stented?
Conclusions Elective stenting of the basilar artery is possible, with minimal risk to the person. Its effect on long-term stroke prevention and its durability is unknown and will need different analyses.
Can you live with a blocked basilar artery?
A person with an acute basilar artery occlusion (BAO) has a high chance of long-lasting disability and death.