Volkmann’s Contracture
What is Volkmann’s Contracture?
The Volkmann contracture is a deformity of a hand, fingers, and wrist caused by injury to the muscles of the forearm. This condition is also named Volkmann ischemic contracture.
Volkmann contracture, also called Volkmann ischemic contracture, is a claw-like deformity of the hand named after the 19th-century German doctor Richard von Volkmann. The name Volkmann ischemic contracture is self-explanatory. Ischemic refers to the possible causes, and contracture indicates shortening. Volkmann contracture condition is a permanent flexion deformity at the wrist and the fingers that outcomes in a claw such as a presentation of the hand. This presentation is because of the permanent shortening of the flexor group of the muscles in the forearm and hence might outcome in pain on passive flexion of the wrist and fingers. The upper limb could be divided into three sections: the arm, the forearm, and the hand. There are lesions classified into 3 levels of severity of VC (Volkmann’s contracture): mild: contracture of the fingers with no or limited loss of sensitivity; moderate: all fingers are flexed, the wrist is stuck in flexion position, and their is loss of sensitivity in hand and the presence of trophic lesions such as blisters
The principal bone of the arm, the humerus, attaches the ulna bone and radius bone (bones of the forearm) with the scapula. The forearm extends from the elbow to the wrist and has two groups of muscles, the flexor group of the muscles anteriorly, and the extensor group of the muscles posteriorly. Those muscles are responsible for the movements at the wrist joint, metacarpophalangeal joints, and interphalangeal joints. Those muscles are supplied by a branch of a brachial artery. The brachial artery courses down the humerus run via the elbow, and then divides into the two terminal arteries, the radial artery, and the ulnar artery. Out of these 2 terminal branches. the ulnar artery is responsible for the blood supply of the flexor group of the muscles. Volkmann contracture (or Volkmann ischemic contracture) is a permanent shortening (contracture) of forearm muscles, generally outcoming from an injury, that gives rise to a clawlike deformity of the hand, fingers, and wrist. It is more typical in children. A similar condition can happen in the foot. Congenital Volkmann ischemic contracture is a very rare condition in which a neonate presents skin, muscular, and nerve lesions because of raised intracompartment pressure and subsequent ischemia, probably due to extrinsic intrauterine compression.
The bones are an important factor in this contracture. We can see that the humerus of the upper arm is usually involved in Volkmann’s contracture. A fracture of the supracondylar space leads to a deficit in the circulation of the arteria brachialis. That is caused by the blocking of circulation and a deficit in blood supply to the muscles and the nerves malfunction. There is a contracture of the muscles, generally, the flexors of the wrist. Yet there is also a contracture that happens in the extensors of the wrist, but this is less common. The flexor group of muscles in the anterior forearm might be divided into a superficial group of the muscle and a deep group of the muscle. Muscles that are commonly involved are The superficial flexors group consisting of:
- Superficial flexors:
- Musculus pronator teres (median nerve innervation)
- Musculus flexor carpi radialis (median nerve innervation)
- Musculus flexor carpi ulnaris (ulnar nerve innervation)
- Musculus flexor digitorum superficial (median nerve innervation)
- Musculus palmaris longus (median nerve innervation)
The deep group consists of:
- Deep flexors:
- Flexor pollicis longus (median nerve innervation)
- Pronator quadratus (median nerve innervation)
- Flexor digitorum profundus (median nerve innervation)
These all muscles are innervated by a median nerve. Exceptions are the flexor carpi ulnaris muscle (that is innervated by the ulnar nerve) and flexor digitorum profundus sharing a dual nerve supply from both the ulnar nerve and the median nerve. Both superficial and deep groups are involved in the development of Volkmann ischemic contracture.
Alternative Names
- Ischemic contracture – Volkmann
- Compartment syndrome – Volkmann ischemic contracture
What are the causes of Volkmann’s Contracture?
Volkmann contracture happens when there is a lack of blood flow (called ischemia) to the forearm. This happens when there is raised pressure due to swelling, a condition called compartment syndrome. Damage to the arm, involving a crush injury or fracture, could lead to swelling that presses on the blood vessels and diminishes blood flow to the arm. A prolonged diminish in the blood flow damages the nerves and the muscles, reasoning in them becoming stiff (scarred) and shortened. When the muscle shortens, it drags on the joint at the end of a muscle just as it would if it were normally contracted. But due to it being stiff, the joint remains bent and stuck. This condition is called a contracture. In this contracture, the forearm muscles are severely injured. This leads to contracture deformities of the hand, the wrist, and the finger.
There are three levels of severity in this contracture:
Mild —
- Muscles: that localized contracture, and only involving parts of the flexor digitorum profundus muscle
- Clinical Presentation: flexion contracture in 2 and 3 fingers, generally including the long finger and ring finger.
- Sensory Effects: none – min sensory loss
- Therapeutic Volkmann’s contracture management: PROM stretching, progressive splinting, AROM exercises
- It normally presents as flexion of a limited number of fingers, 2 or 3, generally involving the middle and ring fingers
Moderate —
- Muscles: flexor digitorum profundus muscle and flexor pollicis longus muscle, might also include a few of the superficial muscles such as flexor carpi radialis, flexor carpi ulnaris, and flexor digitorum superficialis.
- Clinical Presentation: presents as claw hand with flexion at all digits and palmar flexion of the wrist
- Sensory Effects: moderate sensory deficits in median n. and ulnar n. (more in median n.)
- No treatment requires surgery
- all fingers are bent (flexed). and the thumb is stuck in the palm; the wrist might be stuck in a flexed position, and there is usually a loss of some feeling in the hand. Superficial muscles like flexor digitorum superficialis muscle, flexor carpi ulnaris muscle, and flexor carpi radialis muscle might also be affected. Fibrosis of the mentioned muscles leads to a usual claw hand image, which presents as flexion of all 5 digits as well as the wrist. Sensory impairment in areas of the median nerve and the ulnar nerve is also typical.
Severe —
- Muscles: contractures in most extensor muscles and all flexor muscles of a forearm
- The clinical presentation: severe contracture deformities, and intrinsic muscle dysfunction
- Sensory Effects: pronounced sensor deficits from median n. and ulnar n.
- No treatment requires surgery
- all forearm muscles both flexion movement and extension movement of the wrist joint and fingers joints are involved; this is a hardly disabling condition. There is minimal movement of the wrist and fingers. This type of contracture develops in severe cases. and presents as the involvement of both extensors and flexors. This outcome is hardly distorted contractures with pronounced sensory deficits. Long-standing moderate this type of contracture has the potential of yet developing into extreme VIC.
This contracture is classically associated with a supracondylar humerus fracture. Although, any fracture of the arm or elbow may outcome in this deformity. The key precipitating affair in supracondylar humerus fractures is ischemia of the forearm because of acute compartment syndrome. compartment syndrome is a condition in which there is a raises in the intra-fascial pressure of any closed compartment in a body. This might happen reason of two basic reasons: a reduction in compartment size or an increase in the volume of the compartment described as intrinsic or extrinsic compartment syndrome. Therefore, it could be simply claimed that any cause of compartment syndrome might result in VIC (Volkmann ischemic contracture). Causes of compartment syndrome include and Conditions that can cause raised pressure in the forearm include:
- Tight bandages and dressings
- Animal bites
- Burns
- Intensive and excessive exercises— this would not cause severe contractures
- Muscle hypertrophy
- Neoplasms
- Bleeding into a closed compartment (injury to a vessel, congenital disorder, or acquired disorder)
- Injections in the forearm
- Surgery on the forearm
- A forearm or elbow fracture
- Bleeding disorders
- Injury of the blood vessels in a forearm area
Volkmann ischemic contracture is also described as the sequela of an acute arterial insufficiency of the limbs. Emboli lodging in the arterial vasculature could also outcome in ischemia of the muscles outcoming in limb contractures.
What is the Pathophysiology of Volkmann Contracture?
Volkmann contracture develops when there is maintained ischemic damage to the muscles. Decreased blood flow to the forearm, causing ischemia, may be due to increased compartmental pressures or acute arterial emboli. Intracompartmental pressures of greater than 30 mmHg (normal: less than 10 mmHg) significantly impair arterial circulation and are indicative of compartment syndrome. Contractures ultimately develop because of prolonged myonecrosis, which stimulates fibroblastic proliferation, shortening of the cicatrix, and myotendinous adhesions, resulting in a fibrotic pull on the wrists and fingers.
What is the Epidemiology of Volkmann Contracture?
Volkmann’s ischemic contracture is a relatively rare condition. It most typically presents after pediatric upper limb trauma. In one study, the incidence of this contracture was 0.105% of all orthopedic cases, with the majority of cases being men in their second and third decades of life. Another study reviewed a child admitted to the hospital with an upper extremity long bone fracture over the age of thirteen years. Thirty-three of these patients had a fracture of the supracondylar, out of which 3 developed Volkmann ischemic contracture. The subgroup analysis later showed those ipsilateral displaced extension type supracondylar fractures of the humerus or displaced fractures of the forearm had a prevalence of 33% for this contracture. This highlights the importance of maintaining a vigilant eye for signs and symptoms of compartment syndrome in patients with supracondylar humerus fractures, particularly those displaced.
What are the Signs of Volkmann’s Contracture?
There are 5 signs that an individual would have with Volkmann’s contracture. These signs show throughout various severities of the condition; although, the earlier signs could assist individuals identify as a clinician that the client’s symptoms might point to Volkmann’s contracture. The five signs have been referred to as the five Ps. These include:
- Pain
- Pallor
- Pulselessness
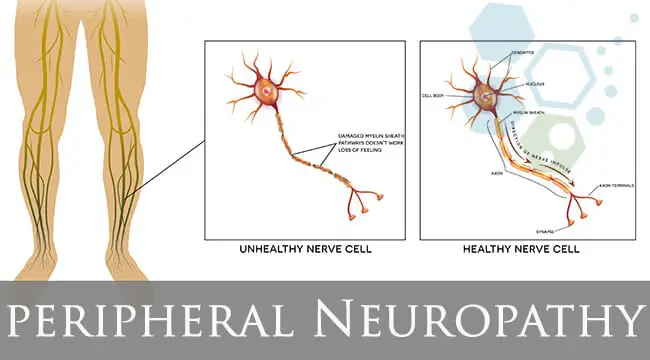
- Paresthesia
- Paralysis
What are the Symptoms of Volkmann’s Contracture?
Symptoms of Volkmann contracture affect the forearm, the wrist, and the hand. Symptoms might include:
- Diminished sensation
- Paleness of the skin
- Weakness in the Muscle and loss (atrophy)
- Deformity of the wrist, the hand, and the fingers causes the hand to have a claw-like appearance
What are Diagnostic Procedures?
Pressure monitoring Intracompartmental pressure (ICP) could be measured by several means including:
- Wick catheter
- Simple needle manometry
- Infusion techniques
- Pressure transducers
- Side-ported needles
- Critical pressure for diagnosing compartment syndrome is unclear Various authors consider surgical intervention if:
- Absolute Intracompartmental pressure greater than 30 mmHg
- Difference between diastolic pressure and Intracompartmental pressure greater than 30 mmHg
- The difference between mean arterial pressure and ICP greater than 40 mmHg
Exams and Tests
The healthcare provider would perform a physical exam, focusing on the affected arm. If a provider suspects Volkmann contracture, detailed questions would be asked about past injuries or the conditions that affected the arm. Tests that might be done include:
- X-ray of the arm
- Tests of the muscles and the nerves to check their function
Outcome Measures
- Functional Outcome Measures
- Active range of motion (ROM) of the elbow & wrist
- Active range of motion and passive range of motion of the digits
- The shoulder and elbow strength using the sphygmomanometer
- Hand strength was measured using a dynamometer
- Pad to pad pinch. key grip and tripod grip strength measured utilizing a Preston pinch gauge
- Sensation measured using:
- Von Frey Test
- Moving two-point discrimination test
- Functional hand sensation – Moberg pickup test
- Fine Motor Function
- McCarron Assessment of Neuromuscular Development (MAND)
- Activities of Daily Living
- Jebson Hand Function Test
Differential Diagnosis
Volkmann contracture needs to be differentiated from:
- Dupuytren contracture
- Pseudo Volkmann contracture
Pseudo-Volkmann contracture is defined as the inability to fully extension of fingers, because of mechanical entrapment, in patients with forearm fractures. That is important to note that signs and symptoms of ischemia are not present in pseudo-Volkmann contracture. This is a relatively rare condition that might be seen in the pediatric age group due to the tethering of flexor digitorum profundus to a fractured ulna. Dupuytren’s contracture is a progressive condition characterized by permanent flexion of one or multiple fingers. The exact etiology is not fully known; although, risk factors include chronic liver disease, alcoholism, smoking, and prior trauma. Dupuytren’s contracture starts as thickening nodules in the palm, afterward progressing to restriction of finger motion. A few pieces of literature do not limit the term ‘Volkmann contracture’ to just the presentation in the hand. though, most literature exclusively mentions Volkmann contracture as the ischemic fibrosis of the anterior muscles of the forearm. For this writing, we would stay limited to its presentation in the hand.
Evaluation
Volkmann contracture generally presents as a classical image, making the diagnosis easy and justifiable with the assistance of the history and the physical examination. more cases do not even require lab investigations for reaching the diagnosis. though, if required, acute compartment syndrome might be investigated with creatine phosphokinase (CPK), blood urea nitrogen (BUN), creatinine, serum electrolytes, serum calcium, urinalysis, and urine myoglobin. Abnormalities in any of the above investigations could suggest compartment syndrome. Coagulation studies might also be warranted if a bleeding disorder is considered a potential lead to compartment syndrome. A complete blood picture will also assist rule out anemia, which can potentiate anoxia in the osteofascial compartment.
Measuring an intracompartmental pressure of the osteofascial compartment. it is the standard of diagnosis when the history and physical examination is nonconclusive. It might also assist confirm the findings of clinical assessment. although, care must be taken not to exclude the compartment syndrome based on the single normal reading. There are several methods of measuring intra-compartmental pressures; among them. the Stryker tonometer gives relatively accurate readings. A compartmental pressure of greater than 30 mmHg to 40 mmHg is considered abnormal. and warrants prompt fasciotomy, and delays of even some hours might prove detrimental to the prognosis. Near-infrared Spectroscopy (NIRS) could also aid the assessment of an acute compartment syndrome and management of an acute compartment syndrome. The wide use of Near-infrared Spectroscopy is limited because of its cost and limited availability of sensors, despite proving to be a reliable noninvasive investigation for the Volkmann ischemic contracture.
Imaging studies such as x-rays, magnetic resonance imaging scans (MRIs), and computed tomography (CT) scans might prove to be supportive in the diagnosis of Volkmann ischemic contracture but are not considered first-line investigations. X-rays might especially assist identify displaced supracondylar fractures of the humerus. computed tomography scans and magnetic resonance imaging scans might also have a role in narrowing down the differential diagnosis of compartment syndrome unrelated to fractures of the upper limb. An ultrasound might also assist exclude the differential diagnosis of acute compartment syndrome.
What is the Treatment of Volkmann Contracture?
The first step in some suspected cases of compartment syndrome or/and earlier Volkmann contracture is the removal of all external dressings, splints, or casts. This meager but meaningful step might halt the development of Volkmann contracture if extrinsic compartment syndrome is the prime offender. that is shown that casts might confine compartment expansion by up to 40% and should always be removed, a step that relieves pressure elevation by about 40% to 60%. This also opens up the field of view to perform required investigations and physical examinations.
However elevation of the limb diminishes swelling, it is not recommended beyond the level of the heart as it can also reduce limb perfusion, thus raising the risk of ischemia. Allowing relative hypertension and correcting anemia could also slow down the progression of acute compartment syndrome. An analgesic might be prescribed according to the intensity of the pain. Although, care must be taken not to get complacent due to the relief of the symptoms. The primary emergency management for an acute compartment syndrome reasoning to Volkmann contracture is emergency fasciotomy. That is commonly agreed those intracompartmental pressures above 30 mmHg – 40 mmHg necessitate this.
Decompression could be achieved by the volar approach or dorsal approach. and both of which release compartmental pressure. The median nerve requires decompression throughout its course, particularly in the high-risk areas (deep to lacertus fibrosus, in the carpal tunnel, and between the heads of pronator teres). Physicians must also be wary of myoglobinuria which is an outcome of prolonged ischemia. Reperfusion syndrome could cause significant systemic abnormalities leading to multiorgan failure. Adequate hydration, monitoring of arterial blood gases, renal function tests, and management of electrolyte disturbances are needed.
If Volkmann contracture has already developed, the management approach depends on the degree of the contracture. Mild Volkmann contracture might be treated with physiotherapy, dynamic splinting tendon lengthening, and slide procedures. These are associated with relatively favorable results. Moderate contractures might need tendon slide, neurolysis, and extensor transfer operations. the severe contractures involving both extensor groups and flexor groups necessitate extensive and radical debridement of the scar tissue. After debridement, tendon transfer procedures might be used to regain the motion of the digits. The Brachioradialis muscle is typically used to regain the movement of the thumb by transferring the tendon to the flexor pollicis longus muscle. The extensor carpi radialis longus muscle is transferred to the flexor digitorum profundus muscle to regain flexion of the finger. Free muscle transplantation may also be required if the belly of the muscle is necrosed. A necrotic muscle could be identified by its color, contractility, consistency, and capacity to bleed.
The first goal is to control the injury that could lead to contracture. This could be treated to diminish and fix any fracture and correct any circulation problem. The compartments might require to be released to evade any extreme swelling that could lead to an injury of the muscles and contractures.
The second goal of treatment is to assist individuals to regain some or full use of the arm and hand. the management depends on the severity of the contracture:
- For mild contracture. muscle stretching exercises and splinting of the affected fingers might be done. Surgery might be required to make the tendons longer.
- For moderate contracture. the surgery is done to repair the muscles, the tendons, and the nerves. If required, the arm bones are shortened.
- For severe contracture. the surgery is done to remove the muscles, the tendons, or/and the nerves that are thickened, scarred, or/and dead. These are replaced by the muscles, the tendons, or/and the nerves transferred from other body regions. Tendons that are still working might require to be made longer.
Medical Management
Prevention is the best management in this condition. Although, there are times when surgical intervention would be indicated. The majority of VC (Volkmann’s contractures) are caused by a supracondylar fracture, and all steps must be taken to improve the healing of a fracture. When there is an intra-compartment pressure (ICP) of >30 mmHg, an urgent fasciotomy is recommended to avoid further complications, Raised ICP threatens the viability of the limb, and compartment syndrome (CS) represents a true medical emergency. Hence, the requirement for decompression by removal of all dressing down to the skin, followed by fasciotomy- Surgical opening of the fascia around the muscles to make more place for the structures inside. This is done to control the onset of Volkmann’s contractures. In moderate Volkmann’s contracture, tendon slide and neurolysis surgery should be accomplished (median and ulnar) along with extensor transfer procedures. Finally, in severe cases of Volkmann’s contracture, debridement of injured muscle might be performed with releases of scar tissue and salvaging procedures. Range of motion and function after an injury is improved through physical therapy and occupational therapy.
(Suspected cases) in case any of these types of signs appear:
- Immediate removal or discontinuation of pressure-causing factors, eg. splint, POP cast, bandage.
- Limb elevation and passive as well as active vigorous movements of segments distal and proximal to the affected area.
- Heat is to be applied to the other limbs and trunk to promote general vasodilation.
- The contrast baths, steam packs, massage, and stimulation could be used to augment local circulation and nerve excitation provided the sensory status of the affected area or region is intact.
(Established cases) the prognosis depends upon a degree of permanent damage to the muscle and the nerves. The therapeutic approach depends upon the type of Volkmann’s ischemic contracture.
- Mild type:
- There is ischemia of the flexor digitorum profundus muscle.
- It could be managed by exercise and dynamic splinting to hold finger extension.
- Moderate type:
- It includes superficial as well as deep finger flexors and flexors of the wrist and thumb.
- If these muscles are still functional, a conservative approach of graded splinting and exercise is useful.
- Muscle lengthening operation might be necessary in non-responding cases.
- Severe type:
- Invariably requires surgery as a contracture progressed beyond the scope of conservative treatment.
- Though, the preoperative passive relaxed stretching. and dynamic splinting facilitates surgery.
The ultimate aim is to achieve maximum extension at the wrist, which is a functional requirement.
- splinting
- for raising the extensibility of the contracted soft tissues on the flexors aspect, effective adjuncts such as
- Massage,
- Ultrasonic and,
- axial traction could be used besides relaxed passive movements.
- If the swelling persists, strong voluntary movements with the limb in elevation should be given.
SURGICAL TREATMENT: following surgical procedure might be done in selected cases:
- Shortening of forearm bones:
- It is done to overcome contracture of the flexor group of the muscles.
- Muscle sliding operation:
- Also known as the Max Page operation,
- This allows correction of the flexion contractures at the wrist joint and finger joints.
- Excision of the dead muscles:
- The necrotic muscle mass is excised and replaced by a healthy or normal muscle obtained from the neighborhood or a distant site.
- Nerve grafting:
- If the median nerve is damaged beyond repair, nerve grafting might sometimes be helpful.
PHYSIOTHERAPEUTIC MANAGEMENT FOLLOWING SURGERY: In all four surgical procedures, the objective of physiotherapy is the re-education of the muscle action. Muscle power, joint range, and sensory status are assessed preoperatively.
Postoperative management following surgery;
- Provide a corrective splint, incorporated with immobilization.
- This is to maintain the corrected position of the contractures, and assists, in movements.
- The measures such as
- Diapulse
- Hand elevation
- Active resistive movements of the related joints are carried out to reduce inflammation and pain.
During mobilization: The basic therapeutic principles are
- Care of the anesthetic areas
- Re-education of the muscle action
- Sensory re-education
- To improve the functional efficiency
- Modification in the splint to further improve a function.
After the surgery, that is important to ensure that the mobility is recovered by:
- Passive stretching techniques
- Range of motion exercises to improve soft tissue elasticity.
Another part of the therapy program involves activating and strengthening the weak agonist to ensure equilibrium in agonist and antagonist pull during joint movement. Progressive Splinting, passive stretching, and tendon gliding, as well as massage, could be used in mild cases to moderate cases of Volkmann’s contracture. With the use of the electromyographic device, the patient could train the affected muscles with cooperativity. The patient is more alert and there is more interaction between the patient and the therapist.
Prognosis
How well an individual does depends on the severity and stage of the disease at the time treatment is started. The result is usually good for individuals with mild contracture. They may regain the normal function of their arm and hand. Individuals with moderate or severe contractures who require major surgery might not regain full function. The result of fasciotomy for an acute compartment syndrome causing the VC (Volkmann contracture) depends on the duration and intensity of compartment syndrome. Immediate fasciotomy, i.e., within 4 hours, leads to minimal sequelae.
The prognosis of developed Volkmann contracture differs greatly from case to case. That is, although, observed that nearly all patients suffering from a contracture during childhood end up with a relatively short limb. Functioning-free muscle transfer (FFMT) outcomes in substantial enhancement of hand function; in contrast, tendon lengthening leads to the recurrence of contractures in multiple cases. Typically speaking, tenolysis, neurolysis, and tendon transfer procedure. and the removal of necrotic muscle produces good hand function in those who have adequate muscle remaining.
Possible Complications
Untreated, Volkmann contracture outcomes in partial or complete loss of function of the arm and hand. Complications of the treatment for VC (Volkmann contracture) vary from procedure to procedure. Common complications of the fasciotomy wound include altered sensations (77%), dry and scaly skin (40%), pruritus (33%), and discolored wounds (30%). The unsightly appearance of the wounds also leads to significant distress to the patients, with 23% of patients altering their behavior to hide their scars. Over-tensioning and under-tensioning are potential complications for tendon transfer surgery. These might outcome even with the most skilled hands as the knot used might loosen or slip. Hematoma formation and wound dehiscence might lead to postoperative worry when flexor origin slide surgery is performed. Also, Functional free muscle transfer surgery is associated with complications. Flap loss, infection, scarring, and tendon adhesion formations are the most commonly occurring.
Postoperative and Rehabilitation Care
Incisions for an acute compartment syndrome are all left open. Negative pressure wound dressings might be applied if major arteries and nerves aren’t exposed. Dressings should be aseptically changed every 24 hours to 48 hours to prevent wound infection. Delayed primary wound closure could be used 7 to 10 days after the incision so that the swelling sufficiently subsides. Precise rehabilitation for Volkmann ischemic contracture differs from surgery to surgery. Immobilization in a cast or splint is recommended for 2 weeks to 4 weeks. Gradual use of the limb might be begun afterward by raising the level of activity with time.
When to Contact a Medical Professional?
Contact the provider right away if someone has had an injury to the elbow region or forearm region. and has developed swelling, numbness, and pain that maintains getting worse. Patients with Volkmann ischemic contracture require to be managed by an interprofessional team. Although, the primary management is to be done by a hand surgeon. The neurologist, the orthopedic surgeon, and the vascular surgeon these three are must all be consulted timely as well. Plastic surgeons could play an important role in reconstruction if needed. Physical therapists are also extremely significant in both the treatment and postoperative care of patients with Volkmann contracture. If reperfusion injury is also suspected. and medical specialists and nephrologists must be consulted to manage the systemic effects of muscle necrosis.
Conclusion
Pain is the first sign in Volkmann’s contracture. A patient would start to feel pain with palpation over the affected area of the forearm. If people have a patient who is starting to have flexor stiffness in 2-3 digits and they have pain when palpating the arm, this might be a sign that the patient is starting the early stages of Volkmann’s contracture. As the condition progresses the individual might show pallor where their skin looks bleached, as well as present pulselessness, where people are not able to feel a pulse in the distal forearm. If the patient is in the moderate and severe stages, this is when they would show the signs of paresthesia, decreased sensation, and observable muscle paralysis.
Hand therapists are one of a few professionals who see individuals regularly after injury. If compartment syndrome has gone unrecognized by physicians at early follow-ups, and mild Volkmann’s contracture begins to develop, a hand therapist might be the one most likely to catch it before it progresses into stages that need surgery. The clinician must know what Volkmann’s contracture is, as well as what the signs and symptoms are so they could catch it in time. If found in the early stages, Passive Range of Motion, progressive splinting, and gradual Active Range of Motion exercises are key. If not addressed until later stages, then referral back to the surgeon might be necessary for surgical intervention.
DISCLAIMER:
This article is intended or purposeful for your general informational purposes only and does not address particular circumstances. it is not a substitute for professional advice(or guidance) or help( or assistance) and should not be relied on to make decisions of any kind. A few or any actions you take upon the information presented in this article are strictly at your own risk and responsibility.
FAQs
What is Volkmann’s ischemic contracture muscle?
Volkmann contracture (or Volkmann ischemic contracture) is a permanent shortening (contracture) of forearm muscles, generally outcoming from an injury, that gives rise to a clawlike deformity of the hand, fingers, and wrist. It is more typical in children. A similar condition can happen in the foot.
What causes Volkmann’s contracture?
VC (Volkmann contracture) happens when there is a lack of blood flow (ischemia) to the forearm. This happens when there is raised pressure due to swelling, a condition called compartment syndrome.
What is the Volkmann triangle?
Volkmann triangle (1875)
[*Earle-Volkmann triangle] – the avulsed posterior edge of the distal tibia (posterolateral tibial lip), in cases of traumatic fracture-dislocation of the ankle.
What is the earliest indication of Volkmann’s ischemia?
The clinical presentation of VC (Volkmann contracture) includes what is typically referred to as the five Ps: pain, pallor, pulselessness, paresthesias, and paralysis. Of these, pain is the earliest sign. On the physical examination, pain accentuated by passive stretching seems to be the most reliable finding.
What is a Volkmann fracture?
Volkmann fractures are avulsion fractures of the posterior lip of the tibia at its articular surface through the essential external rotation or abduction force through the PITFL.
What is congenital Volkmann syndrome?
Congenital Volkmann ischemic contracture is a very rare condition in which a neonate presents skin, muscular, and nerve lesions because of raised intracompartment pressure and subsequent ischemia, probably due to extrinsic intrauterine compression.
What are the types of contractures?
Types of Contractures
Capsular Contracture: The response of the immune system to foreign materials in the human body.
Dupuytren’s Contracture: This condition in which one or more fingers become permanently bent in the flexed position. Muscle contracture: The muscle contracture is a tightening or shortening of muscles.
What are the 5 P’s of compartment syndrome?
Common Signs and Symptoms: The “5 P’s” are oftentimes associated with the compartment syndrome: pain, pallor (pale skin tone), paresthesia (numbness feeling), pulselessness (faint pulse), and paralysis (weakness with movements). Numbness, tingling, or pain might be present in the entire lower leg and foot.
What are the two types of compartment syndrome?
The symptoms can begin suddenly, such as after an injury or if a bandage or plaster cast is too tight. This is called acute compartment syndrome. The symptoms could also come on gradually after exercising and go away when you rest. This is called chronic compartment syndrome.
What is Volkmann Canal also called?
Volkmann’s canals, also named perforating holes or/and channels, are anatomic arrangements in cortical bones. Volkmann’s canals are inside osteons. and they interconnect the haversian canals with each other and the periosteum.
What is Volkmann’s canal also known as?
Volkmann’s canal: Also known as perforating holes, these are microscopic structures found in compact bone that carry small arteries throughout the bone.
What are the three levels of severity in Volkmann’s contracture?
These lesions are classified into 3 levels of severity of VC (Volkmann’s contracture): mild: contracture of the fingers with no or limited loss of sensitivity; moderate: all fingers are flexed, the wrist is stuck in flexion position, and there is loss of sensitivity in hand and the presence of trophic lesions such as blisters
What is the role of the Volkmann Canal?
function in the bone vascular system…of the cortex, is named Volkmann canals; Volkmann canals connect adjacent osteons and also connect the blood vessels of the Haversian canals with the periosteum, the tissue covering the bone’s outer surface.
What is the difference between spasticity and contracture?
Spasticity refers to the involuntary tightening or stiffening of muscles. The term contracture refers to the not normal positioning of the joint.




2 Comments