Dorsalis Pedis Artery
Introduction
The dorsalis pedis artery (DPA) is a major blood vessel located on the dorsal aspect of the foot. It begins at the anterior aspect of the ankle joint as a continuation of the anterior tibial artery. The DPA follows the course of the extensor hallucis longus tendon and terminates at the proximal part of the first intermetatarsal space, where it divides into two smaller arteries – the dorsal metatarsal artery and the deep plantar artery.
The main function of the DPA is to supply blood to the dorsal surface of the foot and toes. Due to its superficial location, the DPA pulse can be easily palpated and is therefore useful in clinical assessment of the peripheral arterial system. The DPA also has an important role in plastic and reconstructive surgery as a pedicle flap for wound coverage.
Course
The proximal aspect of the first intermetatarsal space is reached by the dorsalis pedis artery, which starts just distal to the superior band of the inferior extensor retinaculum, at the midpoint of the medial and lateral malleoli. It follows an oblique path medially, passing along the dorsal surfaces of the talus, navicular, and intermediate cuneiform bones.
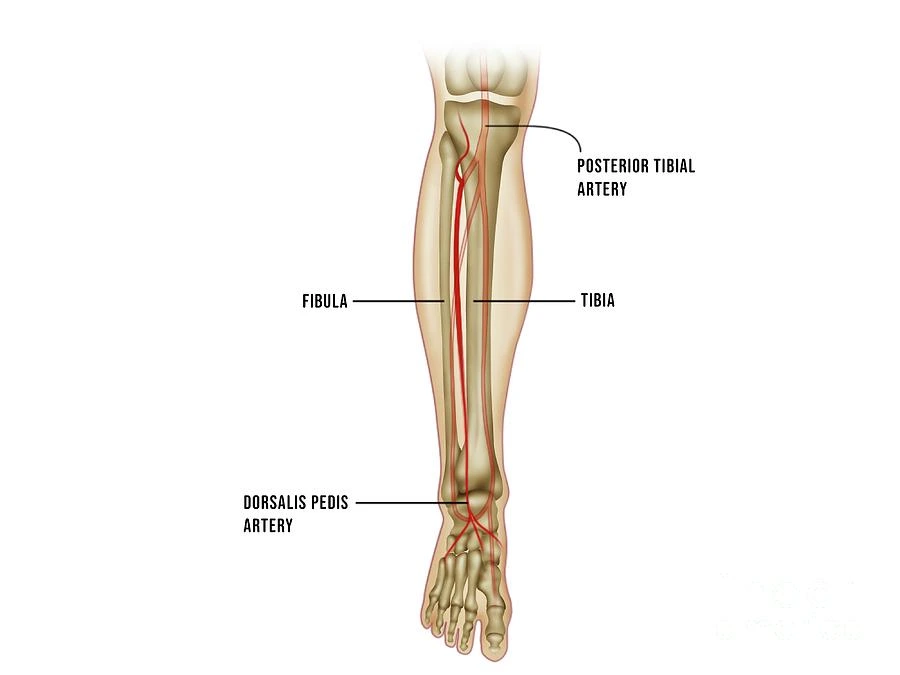
This is where the artery splits off to become the deep plantar artery. The deep plantar artery descends into the sole between the heads of the first dorsal interosseous muscle and anastomoses with the lateral plantar artery (originating from the posterior tibial artery) to form the deep plantar arch. The dorsalis pedis artery is paralleled along its course by the medial branch of the deep fibular (peroneal) nerve, which is located lateral to it.
Branches and Arterial Supply
The DPA gives rise to medial and lateral malleolar branches as well as four main arteries (2):
- Lateral tarsal artery: supplies blood to the tarsal joints and skin overlying the lateral aspect of the foot.
- Medial tarsal artery: supplies blood to the skin and subcutaneous tissue over the medial dorsal surface of the foot.
- Arcuate artery: interconnects the lateral tarsal and dorsal metatarsal arteries, supplying blood to the distal tarsals and metatarsals.
- Dorsal metatarsal arteries: a group of three slender vessels arising distal to the arcuate artery to supply the dorsal aspect of the toes.
Function of DPA
The foot receives an oxygenated blood supply from the dorsalis pedis artery. Healthy and mobile feet depend on adequate blood flow, which can be compromised by reduced blood flow and lead to problems like pain, ulceration, inadequate wound healing, or even limb loss.
The dorsalis pedis artery supplies blood to two muscles located on the dorsal (top) of the foot: the extensor hallucis and the extensor digitorum brevis. Nerves in the foot are involved in vasoconstriction, a physiological process that regulates blood flow throughout the body.
A low or missing pulse may suggest vascular illness; in patients with type 2 diabetes, an absent dorsalis pedis pulse is predictive of significant vascular outcomes. Physicians palpate the dorsalis pedis artery while assessing a patient for peripheral artery disease.
Anatomical Variations
Multiple anatomical variations have been reported in the dorsal pedis artery (DPA) through cadaveric, angiographic, and clinical studies:
- High origin: In over 10% of cases, the DPA originates more proximally as a branch of the posterior tibial, popliteal, or femoral artery rather than the anterior tibial artery. This variant poses a higher risk of inadvertent injury during proximal limb surgery.
- Accessory DPA: Up to 5% of cases demonstrate duplication or accessory DPA that follows a course parallel to the normal DPA. This can confuse the interpretation of angiographic studies and also complicates flap dissection surgery.
- Low bifurcation: Normally, the DPA divides into the first dorsal metatarsal and deep plantar arteries near the first intermetatarsal space. In rare cases, the bifurcation is located more distally near the proximal phalanges. This has implications for the maximal viable length of the DPA flap.
- Aplasia: Complete absence of the DPA has been reported in less than 1% of cases. The arterial supply to the dorsum of the foot is maintained by the enlargement of lateral tarsal and medial arteries. Aplastic DPA can give a false impression of proximal vascular occlusion.
The prevalence of DPA variations differs amongst ethnic populations. Sound knowledge of common variants can guide clinical suspicion and prevent misinterpretation. Most variants are detected incidentally without symptoms. However, certain anomalies can result in a compromise of the vascular supply and require corrective procedures.
Clinical Relations
As the DPA is easily accessible, palpation of the DPA pulse is an integral part of physical examination for peripheral vascular disease. Diminution or absence of pulse signifies proximal arterial insufficiency or local segmental DPA occlusion. In diabetic patients, medial arterial calcification can cause a non-compressible DPA pulse.
The DPA flap is commonly used in lower limb reconstruction surgery due to good vascularity, pliability, and contour. It can be raised as proximally as the distal third of the leg. The flap pedicle needs to be carefully elevated off the extensor retinaculum while preserving the integrity of vascular connections. Venous congestion rather than arterial insufficiency is the predominant cause of flap failures.
Anomalies in DPA origin, course, and branching need to be clearly defined before flap dissections to avoid inadvertent pedicle transection. Lack of knowledge of common DPA variations contributes to flap complications even in experienced hands. Hence, preoperative imaging combined with vigilance during surgery is warranted.
Palpation Dorsalis Pedis Artery Pulse
To determine whether a patient has peripheral vascular disease, doctors frequently check the dorsalis pedis artery pulse, which is absent in 2-3% of young, healthy individuals. It can be palpated lateral to the extensor hallucis longus tendon (or medially to the extensor digitorum longus tendon) on the dorsal surface of the foot, distal to the dorsal most prominence of the navicular bone as a dependable landmark for palpation.
Clinical Significance
Anywhere in the body can experience an accumulation of plaque, or fatty deposits, in the arteries. When fatty deposits collect in the arteries, and blood vessel walls become harmed, they make the walls stickier. Then, materials that are floating through your blood—such as proteins, fats, and calcium—stick to the walls of the arteries, narrowing them. Lower limb arteries are especially vulnerable to atherosclerosis, which can result in reduced blood flow and damage to tissues and organs.
Type 2 diabetes is the most common cause of toe and foot amputations in the United States; peripheral arterial disease (PAD) is a type of atherosclerosis that affects the arteries in the extremities. When these arteries become blocked, the muscles in the lower legs and feet weaken and cramp. One of the most prevalent symptoms of PAD is pain or discomfort in the legs, feet, and toes. Other symptoms include infection, cold feet, skin discoloration, and non-healing foot sores.
A person’s risk factors for PAD include smoking, diabetes, high blood pressure, high cholesterol, kidney disease, obesity, and being over 50. The diagnosis of PAD is twice as common in Black Americans than in White or Asian Americans. Individuals who have PAD also frequently have atherosclerosis in other areas of their bodies.
The test called the ankle/brachial index (ABI), is a standard for detecting PAD and is used to diagnose the condition by taking a blood pressure reading in the lower legs and comparing it to the arm reading. A vascular ultrasound may be performed to assess blood circulation, and a pulse volume recording (PVR), which records blood volume changes in the legs, may also be performed. This test can assist in identifying the location of blockages.
Treatment of PAD
Treatment options for PAD include quitting smoking, altering one’s diet, exercising, taking care of one’s feet and skin, and walking regularly. Managing other health conditions that may be exacerbating the condition is also crucial. If PAD is left untreated, it can result in stroke, renal disease, and amputation.
Co-occurring diseases such as hypertension and hypercholesterolemia may also be treated with medicine; antiplatelet drugs may lower the risk of a heart attack or stroke; Pletal (cilostazol) may increase the distance that a person can walk. If medication and lifestyle changes prove insufficient, further measures such as endovascular intervention or surgical bypass may be necessary.
- Atherectomy: Atherectomy is a procedure that uses a catheter to remove plaque from the artery. It is typically carried out in association with angioplasty.
- Angioplasty: Percutaneous transluminal angioplasty is used to treat PAD. It involves placing a balloon inside the artery to inflate it and push the plaque up against the artery wall.
- Bypass surgery: Bypass surgery involves rerouting blood around a clogged artery by grafting a new pathway. It is performed under general anesthesia in the hospital by a vascular surgeon.
- Endarterectomy: Atherosclerosis endarterectomy is performed in the hospital under general or regional anesthetic by a vascular surgeon to remove plaque from an artery. A shunt is used to temporarily reroute blood flow to the brain during the procedure.
Summary
The dorsalis pedis artery (DPA) is a vital blood vessel of the lower limb located on the dorsal surface of the foot. It originates from the anterior tibial artery near the ankle joint. The main function of DPA is to supply oxygenated blood to the structures on the dorsum of the foot and toes.
As it runs a superficial course, the DPA pulse can be easily palpated. This makes it an important clinical test for assessing circulation to the limb. A diminished or absent DPA pulse signifies potential vascular insufficiency or obstruction. The DPA gives rise to several branches during its course – the medial/lateral malleolar, medial/lateral tarsal, arcuate, and dorsal metatarsal arteries. These supply blood to the overlying skin, joints, and tendons.
While typically constant in position, many anatomical variations have been described in DPA anatomy. These include high origin from popliteal or femoral arteries, duplication, accessory vessels, or complete agenesis. Sound knowledge of common variants can help avoid complications during reconstructive flap dissections.
Due to excellent vascularity and pliability, the DPA flap is commonly utilized for resurfacing wounds over the foot and ankle. Careful pedicle dissection while preserving venous drainage is vital for flap viability. Preoperative planning to rule out significant DPA anomalies can prevent undesirable outcomes.
FAQs
Where is the dorsalis pedis pulse palpated?
The dorsalis pedis pulse is palpated along the dorsal midline of the foot, lateral to the extensor hallucis longus tendon.
What is the significance of an absent dorsalis pedis pulse?
The absence of dorsalis pedis pulse signifies potential occlusion or severe stenosis of the proximal lower limb arteries like anterior tibial, popliteal, or femoral arteries.
What are the most common anatomical variations of the DPA?
The most common DPA variations are high origin from popliteal or femoral arteries, duplication, accessory vessel formation, and complete agenesis.
How can DPA anomalies affect surgical flaps?
Variant DPA anatomy like high origin or accessory vessels can increase the likelihood of inadvertent vascular injury during dissection of dorsal foot flaps.
What are the causes of DPA flap failure?
The most common causes of DPA flap failures are venous congestion due to inadequate drainage and pedicle compression or kinking after inset. Arterial insufficiency is relatively uncommon.
References
Valeii, K. (2023, October 24). Anatomy of the Dorsalis Pedis Artery. Verywell Health. https://www.verywellhealth.com/dorsalis-pedis-artery-5097663
Dorsalis Pedis Artery. (n.d.). Physiopedia. https://www.physio-pedia.com/Dorsalis_Pedis_Artery
MSc, E. O. M. (2023, November 3). Dorsalis pedis artery. Kenhub. https://www.kenhub.com/en/library/anatomy/dorsalis-pedis-artery





One Comment