Dry needling
Dry needling is an invasive technique where a fine needle or acupuncture needle is inserted into the skin and muscle. It is aimed at myofascial trigger points (MTrP) which are hyperirritable locations in skeletal muscle that are associated with a hypersensitive detectable nodule in a taut band. Dry needling is a method physical therapists use (where allowed by state law) to treat pain and movement impairments.
What is dry needling therapy?
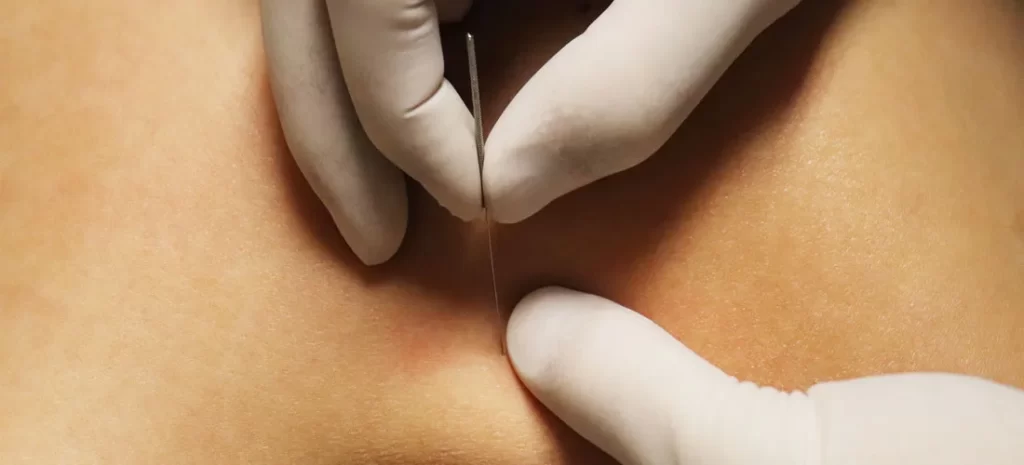
Dry needling is a therapy performed by skilled, trained physical therapists, certified in the procedure. It is a skilled intervention using a thin filiform needle to penetrate the skin and stimulate underlying myofascial trigger points and muscular and connective tissues for the management of neuromusculoskeletal pain and movement impairments. The physical therapist inserts a “dry” needle, one without medication or injection, into regions of the muscle. Trigger point dry needling can also be carried out at the superficial or deep tissue level.
Dry needling (DN) is a procedure utilized in the management of various neuromusculoskeletal pain syndromes by inserting fine monofilament needles through the skin. The needle can be inserted to treat various tissues such as muscles, subcutaneous fascia, tendons, ligaments, scar tissue, periosteum, teno-osseous junction, peripheral nerves, and also neurovascular bundles. The commonly used Dry needling therapy applies to needle the myofascial trigger points (MTrPs). Good quality investigations on myofascial trigger point needling and intramuscular electrical stimulation are needed to evaluate their effects in patients with knee osteoarthritis. Dry needling has been discovered to be effective in various myofascial pain syndromes and musculoskeletal conditions. However, there is a need to consider the effects of dry needling techniques in patients with knee osteoarthritis.
Pathophysiology of myofascial trigger points (MTrPs)
Trigger points are thought to be due to an excessive release of acetylcholine from specified motor endplates. They can also be divided into Active and Latent myofascial trigger points.
- Active trigger points may spontaneously trigger local or referred pain. They induce muscle weakness, restricted ROM, and autonomic phenomena.
- Latent trigger points do not provoke pain unless they are stimulated. They can also alter muscle activation patterns and contribute to a restricted range of motion.
- Thus both active and latent trigger points cause allodynia at the trigger point site and hyperalgesia away from the trigger point following applied pressure.
- The formation of trigger points is induced by the creation of a taut band within the muscle. This band is caused by extreme acetylcholine release from the motor endplate combined with inhibition of acetylcholine esterase and upregulation of nicotinic acetylcholine receptors.
- Originally, taut bands are produced as a normal protective, physiological measure in the presence of actual or potential muscle damage. They are thought to appear in response to unaccustomed eccentric or concentric loading, sustained postures, and repetitive low-load stress. Although, when sustained they contribute to sustained pain.
- Pain provoked by trigger points is due to hypoxia and decreased blood flow within the trigger point. This conducts in a decreased pH which activates the muscle nociceptors to restore homeostasis. This generates peripheral sensitization.
- Trigger points are also concerned with central sensitization. The mechanism remains ambiguous but trigger points maintain nociceptive input into the dorsal horn and therefore contribute to central sensitization.
Mechanisms of Action
Dry needling has been shown to immediately increase pressure pain threshold and range of motion, decrease muscle tone and reduce pain in patients with musculoskeletal conditions. Its suggested mechanisms of action possess:
- Local Twitch Response: Dry needling can also elicit a ‘local twitch response’ which is an involuntary spinal reflex resulting in a localized contraction of the affected muscles that are being dry-needled. Local twitch reactions can lead to alteration in the length and tension of muscle fibers and stimulate mechanoreceptors like A Beta fibers.
- Effects on Blood Flow: Sustained contraction of tight muscle bands within trigger points might cause local ischemia and hypoxia. Dry needling causes vasodilation within the tiny blood vessels leading to increased muscle blood flow and oxygenation.
- Neurophysiological effects: Dry needling may also produce local and central nervous responses to restore hemostasis at the site of the trigger point which results in a reduction in both central and peripheral sensitization to pain.
- Remote Effects: Dry needling of distal MTrP has been found to keep an analgesic effect on proximal MTrP. The publications have conflicting evidence regard to the contralateral effect.
- Placebo Effect
Principles of dry needling therapy
The principles of dry needling (DN) application enclose patient education and support, procedural education, and practical application, such as proper positioning and palpation.
Procedural-education
DN requires during the procedure:
- The patient is asked and motivated to provide feedback and communicate with the clinician during therapy.
- The patient is asked to stay still during the process.
- In the case of trigger points (TrPts) – DN, the patient should be made aware of the local twitch response (LTR) which may be perceived as similar to an electric shock or other sensation. The patient should be made aware that the reproduction of the LTR is the aim of TrPts-Dry needling.
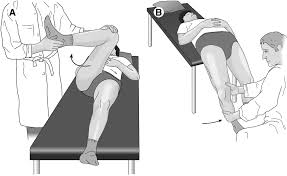
Positioning
Positions may have supine, prone, side-lying, or a combination of these positions. The patient must be comfortable and relaxed. Pillows or rolls etc can also be used for positioning.
Palpation
- Skilled palpation is the key part of identifying TrPts and for the application of safe Dry needling. The therapist should have excellent knowledge of practical anatomy including muscle attachments, bony landmarks, muscle fiber directions, and muscle layers.
- The therapist must be careful about the anatomical networks that need to be avoided including neurovascular structures, lungs, nerves, blood vessels, bones, joints, internal organs, etc., and should at all times aim to evade needling into these structures.
- The TrPts are identified by skilled palpation and the muscle is positioned to permit optimal tension for palpation and treatment. Ensure that the patient and muscles are relaxed before starting the Dry needling procedure.
Deep VS Superficial Dry Needling
Superficial dry needling involves inserting the needle up to 10 mm into the subcutaneous tissue, its benefits include ease of administration, decreased risk of significant tissue trauma, reduced risk of nerve and visceral injury, and patient comfort. Deep dry needling involves the insertion of the needle beyond the subcutaneous tissue into the muscle to reach myofascial trigger points.
How Dry Needling Works?
Dry needling targets your trigger points, or knotted muscles, to prompt them to contract and then relax – because the muscle tightness is what is causing the pain. These trigger points can also develop in the muscle as a result of overuse, lack of use, or trauma to the tissue. Pressing down on a trigger point with your finger may be extremely uncomfortable because these are highly sensitive areas on the muscle tissues.
The treatment allows for to loosen of tight muscles, eases joint pain, and improves blood flow to the affected area. By inserting the hair-thin needle into the muscle membrane, your body will react to the stimulation with a twitch response, demonstrating a release of the trigger point. Inserting the needle is considered to interrupt pain signals. After the needle is removed, the procedure will be repeated at other trigger points as needed.
Dry needling is sometimes confounded with acupuncture, but there are several key differences. Acupuncture employs needles that remain in the skin for a short while, whereas dry needling usually concerns the needle being removed practically right away. Also, the procedure is a bit different, with acupuncture being associated with how energy flows via the body, whereas dry needling is meant to simply release pressure and pain in the muscles.
What are the proposed theories of how Dry needling works?
- Increased blood flow – Needling of the trapezius and Achilles tendon results in increased local blood flow to the needled area.
- Decreased banding – It is hypothesized that following Dry Needling there is reduced banding of the target tissue and restoration of sarcomere length and endomysium spacing.
- Decreased spontaneous electrical activity – Eliciting a local twitch response of a trigger point results in diminished electrical activity at that site. This change in electrical activity might reflect a normalization of the neuromuscular junction.
- Biochemical changes – Following Dry needling of an active trigger point, elevated levels of hydrogen ions, neurotransmitters (bradykinin, 5HT, NE, CGRP, and substance P), cytokines, and chemokines (TNF-α, IL-1b, IL-6, and IL-8) are decreased locally and remotely.
- Pain gate – It is hypothesized that sensorial and proprioceptive stimuli from needling can also drive the gate control mechanisms of pain reduction.
What types of needles or supplies are required to perform Trigger Point Dry needling?
Required supplies include:
- Sterile, single-use solid filiform needles of inconsistent lengths and diameters; as the length increases so should the diameter for improved needle control. Lengths range from 30 to 120 mm in length and 0.20 to 0.50 in diameter.
- Isopropyl alcohol, alcohol swab, or antiviral or antibacterial to clean the skin of the patient
- Firm-fitting treatment gloves
- Sharps container for disposal of used needles
- Recommended but not needed: electrical stimulation unit that may also be modified for motor or sensory TENS and applied through the needles
How does Dry needling differ from wet needling?
Dry needling and wet needling vary primarily in the type of needle used and also the purpose of the insertion of the needle. Dry needling used a solid filament needle to stimulate neuromuscular tissue, and wet needling utilizes a hollow hypodermic needle to inject pain relievers, corticosteroids, or Botox into neuromuscular tissue. Needles utilized for Dry needling are generally much smaller than hypodermic needles and are referred to in terms of diameter and length rather than “gauge.” They are solid instead than hollow and have a rounded rather than the beveled, cutting-edge tip of a hypodermic needle and so are normally more comfortable and carry less risk of introducing infection.
Types of Dry Needling You Need to Know
Trigger Point dry needling
Trigger point dry needling is just what it states; when your patient’s pain originates from an active trigger point, you may also use a needle to directly address that single spot until it terminates (Gattie et al, 2017). If your patient’s pain generator is an enthusiastic trigger point, trigger point dry needling would be a very effective way of dry needling.
- Risk: Medium – If a trigger point is not the pain generator, this type of dry needling will not be adequate, and you will need to choose another method.
- Needle Length: Depends on the depth of muscle that is being treated, the size of the patient, and any anatomical risk elements in the area being treated. Could go anywhere from 25 mm to 125 mm.
- Example Use Case: If a patient’s myofascial pain in his or her neck is caused by a trigger point in the upper trapezius, trigger point dry needling can also relieve these painful symptoms.
Superficial dry needling
Superficial dry needling (Baldry 2002; Griswold, 2019) is commonly utilized by many hands-on healthcare professionals. The needle is only inserted a few millimeters into the skin, achieving the epidermal layer but avoiding the muscle or bone. This method of needling targets the sensorimotor system: the needle adjusts the sensory input, therefore changing the motor output. Pain could also be significantly altered.
- Risk: Low – Because the needle is not piercing many layers of the body, there is a significantly lower opportunity to cause injury to vital organs or neurovascular networks.
- Needle Length: Generally, a short needle, only a few millimeters in length is needed. Ranges are normally from 3mm to 10mm.
- Example Use Case: In precarious areas like the thoracic spine, for
- example, clinicians run the risk of a high risk of puncturing a lung if the needle is inserted too deeply. Superficial dry needling is a great way to transform or alter this patient’s pain perception while avoiding the potential of injury.
Deep dry needling
Deep dry needling (Ceccherelli et al 2002; Boluk 2016; Fernández-Carnero et al 2017) is a higher-skilled way of needling that targets the muscle directly. In some areas of the body, manually manipulating a special muscle can be challenging depending on the location of the target muscle and the tissues that are surrounding the marked muscle. Deep dry needling permits clinicians to get into the target muscle to create a change in pain perception, impact scar tissue or relax or decrease tightness.
- Risk: High – Just like exercise therapy, laser, ultrasound, and other interventions, deep dry needling can be dangerous if you are not incredibly knowledgeable about human anatomy. Only attempt this type of needling if you are experienced and have great respect and understanding of the surrounding anatomy.
- Needle Length: 15mm to 125mm (depending on the target structure)
- Example Use Case: If a patient’s piriformis muscle is extremely tight and causing sciatic nerve pain, deep dry needling can be used to get past the glute muscles and tissue and decrease piriformis tightness, therefore decreasing sciatic pain.
Periosteal Pecking dry needling
Periosteal pecking involves using a dry needle to even peck at the bone in an attempt to help with healing (Dunning et al, 2018). This triggers neuroendocrine responses which, when done intracapsular, can help those dealing with painful osteoarthritis symptoms. Hyaluronic acid presentation, anti-inflammatory processes, and proliferation in endogenous opioid levels are other reasons why we think periosteal pecking is effective, specifically in knee osteoarthritis.
- Risk: High – Inserting a needle into the joint capsule maintains risk. Surgical implants and infection risk elements need to be considered for each patient.
- Needle Length: Deep adequately to get close to or down to the bone. Length will vary based on the size of the patient and the area being needled.
- Example Use Case: If a patient with knee osteoarthritis is experiencing pain, use periosteal pecking, with or without electrical stimulation, in and around the knee joint to alter pain perception in the area and help stimulate chemical reactions that can also help kickstart the healing process.
Electrical Stimulation dry needling
Electrical dry needling (EDN) is a process in which two needles are inserted as electrodes for passing an electric current. One of the main advantages of using Electrical dry needling in clinical practice or acupuncture research is its capacity to set stimulation frequency and intensity objectively and quantifiable. In clinical practice, both low- and high-frequency electrostimulation is used often for diverse conditions. Low-frequency stimulation is specifically recommended for muscular atrophy, whereas high-frequency stimulation is recommended for spinal spasticity. On animals, for example, Electrical dry needling with 2 Hz stimulation seems to induce acupuncture analgesia by the release of endomorphin, β-endorphin, and enkephalin binding to μ and δ opioid receptors. Electrical dry needling with 100 Hz stimulation, however, enhances the release of dynorphin binding to the opioid receptor in the spinal cord dorsal horn to produce an acupuncture analgesic effect.
Most studies demonstrated a wide neuromatrix response that involved the limbic system and limbic-related brain structures consisting of the amygdala, hippocampus, hypothalamus, cingulate, prefrontal, and insular cortices, basal ganglia, and cerebellum. In humans, infact, effects demonstrated a greater effect on the limbic and limbic-related brain structures with real Electrical dry needling than with nonspecific or placebo stimulation. usually, the hemodynamic response produced a signal increase in notable limbic-related regions such as the insula, thalamus, cerebellum, and the anterior middle cingulate cortex. Interestingly, yet, the subgenual anterior cingulate showed a signal decrease.
Clinical Relevance
- The inclusion of electrical dry needling into a manual therapy and exercise schedule was more effective for improving pain, function, and related disability than the application of manual therapy and exercise alone in people with painful knee osteoarthritis.
- The inclusion of electrical dry needling into a program of manual therapy, exercise, and ultrasound was more adequate for improving pain, function, and related disability than the application of manual therapy, exercise, and ultrasound alone in people with patello-femoral pain at mid-term (3 months).
- Electrical dry needling and the upper cervical and upper thoracic HVLA thrust spinal manipulation were shown to be more effective than non-thrust mobilization and exercise in patients with chronic headaches, and the effects were maintained at 3 months.
- Electrical dry needling combined with cervicothoracic manipulation c resulted in greater reductions in pain, disability, and medication intake than nonthrust peripheral joint or soft tissue mobilization, exercise, and interferential current in patients with subacromial pain syndrome. The effects were maintained at 3 months.
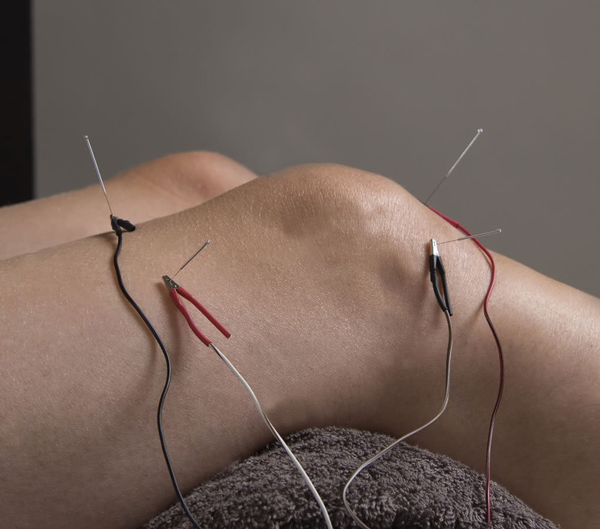
Adding electrical stimulation to the needles is a technical form of dry needling. The proliferation of electrical stimulation triggers a neuroendocrine reaction that is different than needles alone (Butts and Dunning 2016, Perreault et al 2018). This state of dry needling taps into different pain modulation centers and pathways in the central nervous system, making it a practicable choice for chronic pain patients and patients with osteoarthritis.
- Risk: Moderate – Specific conditions are contraindicated to using electrical stimulation, such as patients with pacemakers. The associated risk of other systemic issues must be taken into account on a personal basis.
- Needle Length: Deep – There is not enough investment of the epidermis with superficial needling to attach electrical stimulation, so the needle should be in the muscle at least, or even down to the bone if utilizing the electrical stimulation to carry out periosteal pecking.
- Example Use Case: See Periosteal Pecking above.
Peripheral Neuromodulation
Peripheral neuromodulation is exceeding the extent of practice for most orthopedic healthcare professionals and should only be performed by an authorized acupuncturist or a western medical practitioner with internal medicine education (Longhurst and Tjen-A-Looi, 2013). This involved and dynamic shape of needling is used to influence organs, but the mechanism behind this concept can be activated any time you insert a needle. We do not get to decide what is being involved when a needle is inserted into a patient; the body will do with the stimulus what it will, meaning a systemic response is always a possibility when needling, precise if it is not the desired outcome.
It is no secret that organ pain can cause somatic pain – chest pain comes normally with a heart attack, and back pain is common with kidney stones. Although, this is not a one-way street. The connection also goes the opposite way, which means that it is likely to use a needle within the somatic system to address organ issues or systemic issues. When I insert a needle in someone, let’s say in an arm, I am not just needling the brachialis muscle (as an example). I am also needling the C5/C6 dermatome and concerning these spinal segments, which means anything else that’s innervated by C5/C6, including any organs or muscles, is also going to be affected.
- Risk: High – While you can use needles to affect certain changes, ultimately the nervous system chooses what’s going to be affected. This raises the risk for autonomic nervous system reactions, such as changes in blood pressure or heart rate.
- Needle Length: Variable, relying on the structure being targeted.
- Example Use Case: When acupuncturists are treating diseases like asthma, high blood pressure, or anxiety, peripheral neuromodulation concepts are used.
If I learned anything throughout my dry needling affairs, it is this: all needling procedures are not created equal for all patients. These small appliances make a mighty impact on the body’s muscular, skeletal, endocrine, and nervous systems and, when utilized properly, can yield incredible results in a short amount of time. Although, using needles effectively needs intimate knowledge of anatomy and physiology as well as hands-on experience. To help you use needling as an agent for positive patient results, I would like to introduce you to a handful of dry needling techniques and give you approaches on how to determine which kind is best for each unique patient.
How to Select the Best Dry Needling Method
Every evidence-based treatment intervention has a time and a place, and it is necessary to choose a tool based on the patient in front of you. Before I choose which kind of dry needling to utilize, I first think about my Pentamodal Method of Dry Needling and explore if dry needling is even the appropriate avenue of treatment. Use the three P’s to cover all of the elements that dictate if dry needling is right for your patient:
- Practitioner: Are you, the practitioner, prepared and experienced in dry needling? Are you convinced in your ability to use the tool to cause positive change?
- Patient: Is your patient satisfied with the idea of dry needling? Do they have any symptoms and/or conditions that would disqualify them from being needled safely? Do they have any contraindications or precautions that would control you from needling them, or give you pause on using dry needling as an intervention?
- Pathology: Is your patient showing a well-defined condition that can be impacted through a form of dry needling?
If the answer to any of these is “no,” consider choosing an alternative method of treatment or attending a CEU course to learn how to dry the needle safely and effectively. If the answer to those questions is “yes,” guide to the subsequent list of dry needling techniques to find which type has the best chance of delivering your (and your patient’s) desired results.
Describe a general protocol when performing Trigger point dry needling.
Examination and identification of neuromuscular impairments
- Absence of contraindications
- Approval of patient disclosure of potential adverse effects
- Adherence to clean needle procedure and universal precautions (ie, donning gloves, cleaning of the skin, and single-use filiform needles)
- Designation of the trigger point
- Direct needling of the trigger point to stimulate a twitch response (ie, various techniques exist [piston motion, etc.] and are at the discretion of the practitioner)
- Removal and proper dumping of the needle; check a patient for adverse effects
- Examination of the patient’s impairments to determine the effect of needling
Introduction of different necessary restorative interventions such as manual therapy, therapeutic, exercise, or modalities that would be indicated to further reduce the patient’s impairments and enhance function.
What Kind of Needles Are Used?
Dry needling involves a thin filiform needle. The needle pierces the skin and stimulates underlying myofascial trigger points and muscular and connective tissues. The needle permits a physical therapist to target tissues they are not able to reach with their hands. Physical therapists wear gloves and personal defensive equipment when dry needling. The employed sterile needles are disposed of in a medical sharps collector.
How many needles do you use?
It depends on how numerous spots need needling and the patient. The first time or two, I likely would not needle them head to toe. I would pick a few of the worst spots. But I have a patient who has chronic neck and shoulder pain. With someone like her, I presumably would use at least a dozen needles.
How long does a dry needling session last?
Usually, about 20 minutes if that is the only remedy, or it can be part of a longer physical therapy session. For instance, if a patient has a stiff shoulder after I needled their shoulder, I will also do some range of motion exercises to assist their shoulder. If their range is pretty good, I can try some light strengthening.
How long do the results last?
Most patients experience an instantaneous improvement in functionality and mobility after a dry needling treatment and will feel less pain within the first 24 hours. After undergoing 2 or 3 sessions one time per week you will generally feel the lasting positive effects of dry needle therapy. The moderate dry-needling patient will undergo 2 or 3 sessions once a week. For additional intense issues or rare disorders, 5 to 6 sessions, sometimes 2 per week, may be advised. A dry needling session prevails for about 20 to 30 minutes. However, your physical therapist might compile the session with traditional physical therapy like targeted stretching or range of motion exercises to increase the effects of dry needling.
How many sessions do you need?
That changes depending on the problem and how long you have had it. I have had people that have one or two sessions and that’s all they require to feel good. But I also have patients who have chronic problems, and dry needling is a method to manage a chronic problem. I have some patients who come in once a month. They just get needled wherever they require it, and that’s how they assist to manage their pain.
Aftercare for dry needling
The following is recommended for Dry needling aftercare:
- The muscle and treatment area needed should be compressed instantly following needle withdrawal for hemostasis for up to 30 seconds or until any bleeding has stopped. A cotton swab may also be used and should be discarded as appropriate.
- The patient should be educated on aftercare which may also contain limbering exercises, gentle stretching, the use of hot packs or cold packs, activity modifications, and motor retraining, as deemed necessary.
What Pain Can Dry Needling Help to Relieve?
Dry needling could also help provide pain relief from many ailments, including the following common conditions:
Arthritis
- Arthritis is joint inflammation. There are dozens of types of arthritis, and the most ordinary type is osteoarthritis – whose symptoms may also include joint pain, stiffness, and swelling. People who tend to get osteoarthritis are those who are implicated in a sport and those who are getting older, as this is the wear and tear type of arthritis.
- Osteoarthritis emerges from the wearing down of the protective cartilage that cushions the ends of your bones in a joint. Dry needling is a convincing treatment for reducing pain from osteoarthritis because it increases blood circulation around the joint, thereby delivering natural relief.
Fibromyalgia
- Fibromyalgia is featured by chronic pain, stiffness, and tenderness of your musculoskeletal system. It also ensues with other conditions such as rheumatoid arthritis, lupus, and other rheumatic conditions.
- Dry needling conducts for patients who have fibromyalgia by targeting trigger points that cause pain. For patients who have no specific trigger points, therapists focus on the area where the patient experiences symptoms. Through dry needling, the affected area is not only comfortable, but it also enriches blood circulation.
Rotator Cuff Tears and Shoulder Pain
- A torn rotator cuff can also be caused by an acute injury or by a repetitive stress injury, which tends to occur due to several small tears in the shoulder’s rotator cuff. The rotator cuff allows shoulder movement and stability; when it is injured, it can cause pain and the incapacity to move the shoulder very easily.
- When feasting rotator cuff tears, dry needling is often accompanied by strengthening exercises. After treatment, you can also expect to regain the range of motion in your shoulder.
Indication of dry needling therapy
- Dry needling can also be indicated for myofascial pain with the presence of trigger points. Dry needling has also been shown to be advantageous for the treatment of strains, osteoarthritis, and tendinopathies.
- Contraindications
- Patient unwilling – fear, patient belief,
- Not able to give consent – communication, cognitive, age-related factors,
- Medical emergency or acute medical condition,
- Over a site or limb with lymphedema, this can also increase the risk of infection or cellulitis and the difficulty of fighting the infection if one should occur,
- Irregular bleeding tendency, Compromised immune system, Pregnancy, Children, Vascular disease, Diabetes.
Contraindications of dry needling therapy
Dry needling therapy should be avoided in patients under the following circumstances:
Absolute contraindications
- In a patient with needle phobia.
- Patient unwilling – fear, patient belief.
- Incompetent to give consent – communication, cognitive, age-related factors.
- Medical emergency or acute medical condition.
- Over an area or limb with lymphedema may increase the risk of infection or cellulitis and the problem of fighting the infection if one should occur.
- Inappropriate for any other reason.
Relative Contraindications
- Abnormal bleeding tendency
- Compromised immune system
- Vascular disease
- Diabetes
- Pregnancy
- Children
- Frail patients
- Patients with epilepsy
- Psychological status
- Patient allergies
- Patient medication
- Unsuitable patient for any reason
What are the safeguards for Trigger point dry needling?
- Needle phobia or aversion
- Significant cognitive impairment
- Communication barrier
- History of traumatic or spontaneous pneumothorax
- Hyperalgesia or allodynia
- Local skin lesions or infections
- Compromised immune system
- Metal allergies
- Abnormal bleeding tendency
- Vascular disease
- Over any implant
- Area of laminectomy
What are dry needling side effects?
Dry needling is a therapeutic pain relief option but can threaten people, and really what are dry needling’s side effects, are there any? In treatment, a physical therapist carefully inserts very fine needles into your muscles in specific areas known as trigger points. Pain relief ensues as the result of the needle “releasing” the trigger point. We are proud to propose dry needling in Denver as one of our many treatment options.
Dry needling is supported by scientific studies and modern Western medicine. Many patients have come to love this treatment as it provides relief without the dangers and side effects commonly associated with prescription pain medication and surgery. Dry needling is very protective when performed by a highly qualified physical therapist, however, like any treatment, it does come with a risk for a few minor side effects. While most of the patients do not encounter any problems, here is a closer look at the potential dry-needling side effects.
LIST OF DRY NEEDLING SIDE EFFECTS
Many patients do not undergo any side effects following a dry needling session. When side effects do happen, they are most often mild. Dry needling side effects include:
TEMPORARY INCREASE IN PAIN
This usually appears within 24 to 48 hours following treatment and may resolve on its own or with mild activity or stretching of the area or light massage.
BRUISING OR BLEEDING
Bruising or bleeding can also occur at the insertion site. Bleeding or bruising at the insertion point is rare and only involves about 10% of patients. If you are on blood thinners or have blood vessel problems, you may also be more likely to experience this side effect.
FAINTING
Fainting is another distinctive risk that is most likely to affect healthy, athletic men, more aging or weaker individuals, middle-aged women with blood pressure under 120/70, and people who are thirsty, hungry, or eat immediately before their appointment.
FATIGUE AND TIREDNESS
Some individuals can experience general feelings of fatigue or weakness.
SKIN REACTIONS
Small red areas may develop on your skin as a histamine reaction to the needles. These spots usually go out on their own within a few minutes or a few hours.
PNEUMOTHORAX
Pneumothorax, or a collapsed lung, is an extremely rare side effect that can normally be detoured by only seeking dry needling services from someone with the proper training and certification, such as the physical therapists at Denver Physical Medicine and Rehab.
DRY NEEDLING SIDE EFFECTS IN DENVER
For the vast majority of patients, the advantages of dry needling outweigh the potential side effects by a large degree. If you are curious in learning more about dry needling and finding out whether this unusual dry needling therapy is the right solution to your chronic pain, schedule a consultation today!
Are There Any Adverse Effects?
Dry needling is considered to be a safe, mechanical process whereby the needle is manually manipulated without any medication. The little side effects which may occur include temporary soreness or discomfort. This is caused by the twitch reaction, which is reported to be minor as compared to the pain that was caused by the trigger point.
Not everyone is a prospect for dry needling. Pregnant women, individuals who have a fear of needles, and patients who have compromised immune systems or skin conditions must consider an alternative treatment for their myofascial pain. Any patient who is curious about dry needling therapy should consult their doctor first. Any side effects from the treatment must be reported to your physical therapist or your physician.
Evidence
The significance of this treatment depends greatly on the skill of the therapist to accurately palpate myofascial trigger points as well as kinaesthetic awareness of the anatomical structures.
- A Cochrane review (2005) of RCTs completed that trigger point dry needling may also be beneficial for low back pain when used in combination with other treatments. Although further higher-quality studies are needed to confirm this.
- A Crossover study (2016) on the Effect of Dry Needling on Spasticity, Shoulder Range of Motion, and Pressure Pain Sensitivity in Patients With Stroke concluded that dry needling reduced localized pressure sensitivity and increased shoulder range of motion in individuals who had experienced a stroke, with no significant effect on spasticity.
A systematic examination of 23 trials considering needling therapies for myofascial trigger point pain terminated that direct dry-needling (where MTrPs were directly targetted) was as beneficial as wet needling. There is no clear evidence that it is beneficial beyond a placebo. More analyses of higher quality with reproducible diagnostic criteria and a valid placebo are needed to draw firm conclusions on this.
A systematic study and meta-analysis with level 1a evidence suggest that:
- Very low-quality to moderate-quality evidence suggests that dry needling conducted by physical therapists is additionally more effective than no treatment, sham dry needling, and other treatments for reducing pain and enhancing pressure pain threshold in patients presenting with musculoskeletal pain in the immediate to 12-week follow-up period.
- Low-quality proof suggests superior results with dry needling for functional outcomes when reached to no treatment or sham needling.
- No discrepancy in functional outcomes exists when compared to other physical therapy treatments.
- Evidence of the long-term usefulness of dry needling is currently lacking.
Abstract
Dry needling is often a treatment technique in orthopedic manual physical therapy. Although different dry-needling approaches exist, the more common and nicely supported approach targets myofascial trigger points. This article seeks to place trigger point dry needling within the context of pain sciences. From a pain science viewpoint, trigger points are constant sources of peripheral nociceptive input instructing peripheral and central sensitization. Dry needling cannot only change some aspects of central sensitization, but it also reduces local and referred pain, improves the range of motion and muscle activation pattern, and varies the chemical environment of trigger points. Trigger point dry needling must be based on a thorough understanding of the scientific background of trigger points, the contrasts and similarities between active and latent trigger points, motor adaptation, and central sensitized application. Several development studies are formed, as well as comments on dry needling and acupuncture.
Trigger point dry needling is a treatment technique utilized by physical therapists around the world. In the United States, trigger point dry needling has been approved as within the extent of physical therapy practice in a growing number of states. There are several dry-needling techniques, based on various models, including the radiculopathy model and the trigger point model, which are discussed here in detail. Special attention is paid to the clinical proof for trigger point dry needling and the underlying mechanisms. Comparisons with injection therapy and acupuncture are noted. Trigger point dry needling is a rather new technique used in combination with other physical therapy interventions.
FAQ
What is the current evidence regarding the effectiveness of dry needling?
Considerable studies indicate support for dry needling in cases of myofascial pain syndromes, spasticity as a result of stroke, shoulder pain, lateral epicondylalgia, heel pain, temporomandibular dysfunction, and pain.
What are the current practice requirements for a physical therapist to perform dry needling?
Routine requirements vary from state to state. Currently, there are 6 states in which dry needling by a physical therapist is prohibited and 27 states in which the course act or the Physical Therapy Board precisely allows it. In the remainder of the states, there has not yet been a decision regarding physical therapists performing dry needling. Requisites for training or competency differ from state to state.
Does dry needling really work?
Dry needling can also help to reduce pain and soreness. A specially qualified physical therapist employs a thin needle to release muscle tightness, ease tendonitis and inflammation, and facilitate healing. “I engage it with about 30 percent of my patients at Spine Group Arizona,” Kylie said.
What is the distinction between acupuncture and dry needling?
Dry needling is focused on employing strong stimulation on the muscles to get them to remove. Acupuncture, on the other hand, does not use strong stimulation and it is established on channel theory and uses points to heal the body naturally.
How painful is dry needling?
Does dry needling hurt? The actual insertion of the needle does not damage it, these needles are very thin. Sometimes the muscle would twitch when you put it in, and it could also feel sore if that happens. You frequently will feel a little muscle ache or soreness for a day or two after that feels like you worked out that muscle.
Who can benefit from it?
If you have had a muscle injury, it can help. A few people come in to try it when nothing else seems to work, while others use it as part of a treatment plan that encloses other types of physical therapy, such as joint mobilizations (when your therapist moves your joints in specific directions with his or her hands), stretching or soft tissue work (massage).
Does dry needling help with torn ligaments?
No. It is more for muscle pain. It would not be beneficial for that type of injury or a further type of pain, like gallbladder pain.
What should you not do after dry needling?
Avoid ice unless you are icing a bruise, heat is more suitable for muscle soreness. Drink alcohol, but it is suggested that you do not do so excessively.
Why do I feel weird after dry needling?
It is expected to feel tired, nauseous, emotional, giggly or “loopy” and somewhat “out of it” after treatment. This is a normal response that may last up to an hour or two after treatment. Infrequently, there are times when treatment may also actually make your typical symptoms worse in the short term.
Does dry needling go to the bone?
The needle is only inserted a few millimeters into the skin, reaching the epidermal layer but detouring the muscle or bone. This method of needling targets the sensorimotor system: the needle modifies the sensory input, thus changing the motor output. Pain can be significantly altered as well.






7 Comments