Pronator Teres Syndrome (PTS)
What is Pronator Teres Syndrome?
Pronator teres syndrome is a condition that affects the median nerve as it passes through the pronator teres muscle in the forearm. The pronator teres muscle is responsible for pronation, the rotational movement of the forearm that turns the palm downward.
In pronator teres syndrome, the median nerve becomes compressed or irritated within the pronator teres muscle, leading to a variety of symptoms. The exact cause of this compression is often unknown, but it can be associated with repetitive forearm motions or activities that involve the repeated use of the forearm muscles. In complete the pronator teres syndrome, the involved muscles such as the PT (pronator teres), FCR (flexor carpi radialis), PL (palmaris longus), FDS (flexor digitorum superficialis), along with muscles innervated by the anterior interosseous nerve.
Pronator teres syndrome (PTS) is a rare disease caused by compression of the median nerve (MN) by the pronator teres (PT) muscle or other adjacent anatomical structures in the upper forearm. The classical presentation of Pronator teres syndrome is that of forearm pain with sensory changes in the median nerve territory.
Pronator Teres Syndrome (PTS) is a compression neuropathy of a median nerve at an elbow. It is not as normal as compression at the wrist which is Carpal Tunnel Syndrome (CTS). Pronator Teres Syndrome and Carpal Tunnel Syndrome present similarly, however, Pronator Teres Syndrome could be distinguished by a lack of sensation in the distribution of the palmar cutaneous branch of the median nerve (PCBMN) and the absence of common Carpal Tunnel Syndrome test findings. The palmar cutaneous branch of the median nerve branches off of the median nerve proximally to the carpal tunnel. Because of its site of origin, this nerve could be affected by median nerve entrapment of the forearm (such as in Pronator Teres Syndrome), but will not be affected by entrapment in the carpal tunnel. It shall also be noted that Anterior Interosseous Nerve Syndrome (AIN Syndrome) is another condition. and it could happen with anatomical compression at the level of the elbow, equal to Pronator Teres Syndrome. Though, Anterior Interosseous Nerve Syndrome presents strictly as a motor palsy of some or all of the muscles innervated by the median nerve in the forearm, including flexor digitorum profundus of the index fingers and middle fingers, flexor pollicis longus, and pronator quadratus.
The Pronator teres syndrome should also be determined from CTS ( carpal tunnel syndrome ). and median nerve entrapment at the level of the wrist, which is the most common median nerve entrapment syndrome, as well as from the Anterior Interosseous Nerve syndrome, brachial plexus injury, or cervical radiculopathy. The Pronator teres syndrome has a sensory loss in the entire median nerve distribution versus carpal tunnel syndrome, where sensation is spared over a thenar eminence because the palmar cutaneous branch leaves the median nerve.
In addition, pronation is spared in carpal tunnel syndrome, and nocturnal paresthesia symptoms are typically not present in pronator teres syndrome. NCS and amplitude of the median nerve might reduce in a forearm, but the distal motor and sensory latencies are normal in pronator teres syndrome except when there is associated carpal tunnel syndrome. Because of overlapping symptoms, carpal tunnel syndrome is a rare time diagnosed, and more proximal pronator teres syndrome is missed when both are present in the same limb. Thus in patients with carpal tunnel syndrome, pronator teres syndrome should be ruled out, particularly when the patient is a candidate for surgery.
To distinguish Anterior Interosseous Nerve from pronator teres syndrome, the pronation should be demonstrated with the elbow flex or bent (pronator quadratus function) to evade the contribution of the PT, which is the primary muscle to pronation with the arm extension. Also, there is no sensory loss in Anterior Interosseous Nerve syndrome (as it carries only deep sensory fibers to a wrist). and in a few cases, pronator teres syndrome might have only mild paresthesias in an MN distribution. In both cases, The FPL and FDP to digits two and three might be affected; but in Anterior Interosseous Nerve, the pronator quadratus (PQ) does not weaken the PT as Anterior Interosseous Nerve leaves the median nerve distal to the PT muscle. Clinically, in both cases, the individual presents with an unable to flexion the distal phalanx of the thumb, index fingers, and middle fingers and that with weakness of pronation movement.
In the case of brachial plexus injury or cervical radiculopathy, the examination might reveal a weakness in another muscle outside the median nerve territory. The neck pain that radiates to the arm is a common complaint, suggesting cervical radiculopathy. One group of authors describes a neuralgic amyotrophy as a potential competing condition with pronator teres syndrome due to equivalent symptoms, but it usually involves multiple nerves, and pain is more typically localized in the shoulder rather than in the forearm. Neuralgic amyotrophy is an idiopathic condition that usually enhances spontaneously in 6 to 12 months.
Pronator Teres muscle anatomy
The pronator teres muscle is a long, round muscle that is situated on the anterior aspect of the forearm. This muscle has two various points of origin: the humeral head and the ulnar head. A humeral head is larger and more superficial. The ulnar head is deeper and the joints it is at an acute angle, forming a one-muscle belly. The ulnar head is a few times more tendinous, a few times more muscular, and at times not present. The median nerve typically passes in between the two heads of the pronator teres (83% of the arms). where it is at risk for compression. The pronator teres from the medial border of the Cubital Fossa.
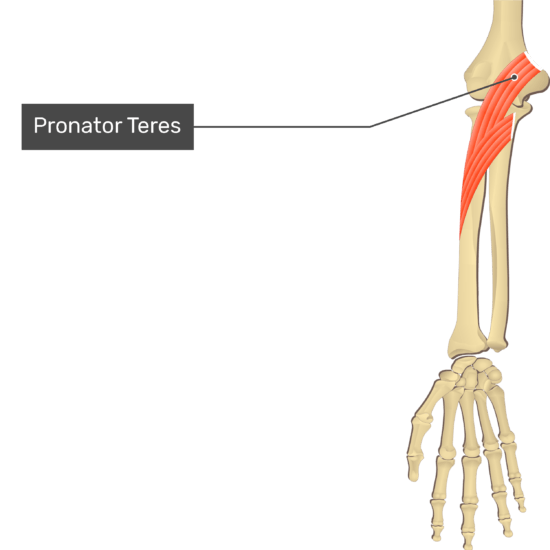
Origin
- Origination of the head of the Humeral: Instantly over the humeral medial epicondyle, common flexor tendon, and deep antebrachial fascia.
- Origin of Ulnar Head: Medial side of the coronoid process of an ulna bone.
Insertion
- Middle of the lateral surface of a radius.
Nerve
- The median nerve, C6, and C7.
Artery
- Ulnar artery, anterior recurrent ulnar artery.
Function
- The Pronator teres muscle pronates the forearm and assists in elbow flexion. It acts synergistically with a pronator quadratus. If a flexed elbow, then the muscle fibers are shortened and less able to produce force.
- Synergist: Pronator Quadratus
- Antagonist: Supinator, Biceps Brachii
Anatomy of the Median nerve:
- The median nerve arises from the C6, C7, C8, and T1 of the spinal cord. It originates from the brachial plexus. Then runs down into the arm from the, then enters into the cubital fossa, and passes between the two heads of the pronator teres muscle into the forearm. Then it runs in between a flexor digitorum superficialis muscle and flexor digitorum profundus muscles and enters the hand via a carpal tunnel. It provides most of the flexor muscles in the forearm and the hand. It supplies the sensation of the palm, the thumb, the index finger, the middle finger, and half the ring finger. In the proximal part of the forearm, it gives rise to the anterior interosseous nerve which provides a flexor of the thumb (FPL), the flexor digitorum profundus muscle of the index phalanx, the pronator quadratus muscle and terminates in a sensory branch to the wrist bone. Compression of a median nerve in a proximal part outcome in the weakness of these three muscles and can lead to pain in the wrist.
Nerve Entrapment
- Path of the median nerve through pronator teres. The median nerve generally runs between the two heads of the pronator teres, making it a possible site of nerve entrapment. There would likely be pain and paresthesia in the distribution of the median nerve. This entrapment can present similarly to the carpal tunnel because the median nerve is affected. If pronator syndrome is present, the individual should have a negative Phalen’s Test, a negative Tinel’s Test at the wrist (and a positive Tinel sign at a pronator teres), and likely pain with resisted pronation. The Pronator Teres Syndrome Test would such as be positive. In extra, there might be a history of repetitive pronation/supination such as with an individual who plays racquet sports.
Pathology
- The median nerve could be involved at many locations around the elbow five:
- The distal humerus: avian spur and ligament of Struthers
- Proximal elbow: thickened biceps aponeurosis
- Elbow joint: between the humeral head and ulnar head of the pronator teres muscle ( most common reason)
- The proximal forearm: thickened proximal border of the flexor digitorum superficialis muscle
- Gantzer’s muscle
How does the Pronator Teres Syndrome Occur?
Pronator teres muscle entrapment of the median nerve results in pronator syndrome. It is associated with prolonged or/and repetitious forearm motions, i.e., gripping movement with the palm down. This kind of problem is more likely to affect mechanics, carpenters, assembly line workers, tennis players, rowers, and weight lifters. The condition is usually associated with excessively developed forearm muscles. and is more typical in the dominant arm. The typical age of beginning is in the fifth decade. and the condition is four times more typical in women than in men. Such as other neuropathies, patients with diabetes, alcoholism, or hypothyroidism are predisposed to this condition.
Pronator syndrome might develop due to:
- Age and Gender – Males and Females could both develop Pronator Syndrome, but it is most usually a problem for women over 40.
- Medical Reasons – Individuals who suffer from this type of disease like diabetes and hypothyroidism are at raised risk for developing pronator Teres syndrome.
- Professions – such as carpenters, mechanics, and others who rotate their forearms as part of their job are at raised risk.
- Sports Activities – such as racquet sports (tennis), rowing, and lifting weights could contribute to the development of this syndrome.
- Other – This syndrome could develop due to bony abnormalities, trauma, and tumors.
It typically happens after prolonged or/and repetitive movement of forearm pronation movement(turning the palm to face downwards), accompanied by forced flexion of the fingers. In simple terms, forceful grasping with a hand and twisting at a wrist. These kinds of activities are typical in manual occupations such as carpentry and mechanics. In a few sports activities, racket sports, rowing, and weightlifting are the most typical culprits. The cause of this reasons compression is due to the increase in the bulk of muscle of the pronator teres muscle. This type of syndrome (PTS) might also ensue as an upshot of trauma to the forearm, bony abnormalities, tumors, or/and restrictive bands of fibrous tissue and scar tissue. Interestingly, it is four times more typical in females than males.
Pronator syndrome could happen in both males and females, but it is most common in women over the age of forty years. The condition is caused by compression of the median nerve, generally by swollen and inflamed structures around an elbow. certain underlying some condition like hypothyroidism and diabetes are considered risk factors for this type of syndrome. This type of (Pronator Teres syndrome) syndrome is more dominant in those who people routinely take part in movements that need repetitive pronation movement(turning a palm to face the floor) while flexing the fingers, such as when catching an object. A few typical job roles that are particularly prone to developing this type of syndrome include carpenters and mechanics. Sports such as weight lifting, rowing, and those use rackets are also susceptible to the condition. In extra, pronator teres syndrome could be led to other factors like trauma in the forearm, tumors, and bony abnormalities
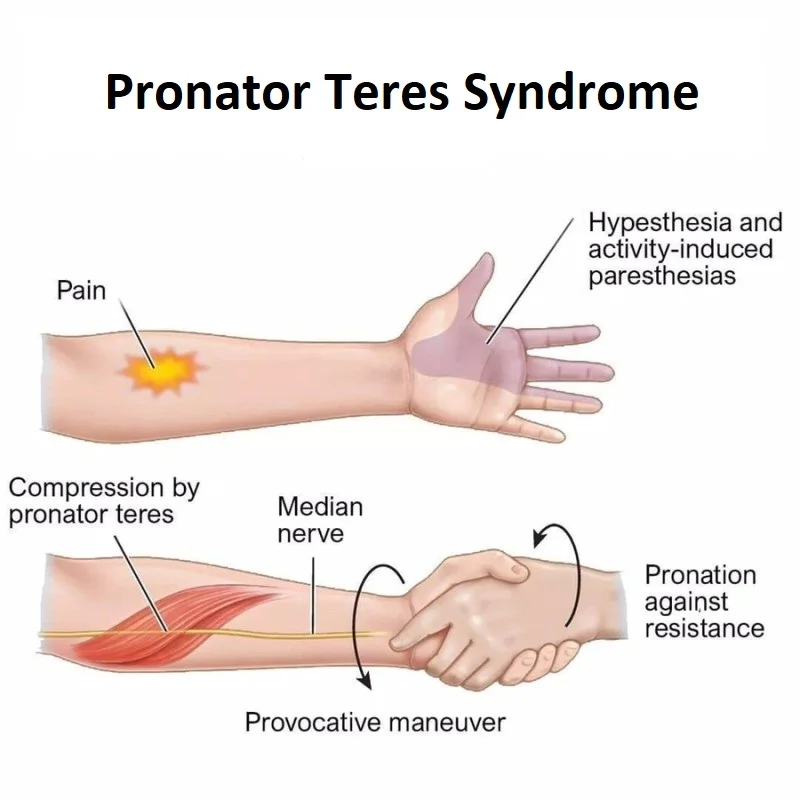
What are the symptoms of Pronator Teres Syndrome?
The symptoms of Pronator Syndrome (PTS) are equivalent to, but distinct from Carpal Tunnel Syndrome (CTS). A key difference is that Carpal Tunnel Syndrome symptoms worsen at night, while Pronator Teres syndrome symptoms do not.
- Aching in the forearm
- Weakness in the Muscle in the forearm, wrist, and/or fingers
- Numbness in the forearm, palm, and/or fingers
- Pain in the forearm, palm, and/or fingers
- Pain that raises with activity, but enhances with rest
- Tenderness when pressing on a pronator teres muscle
- Tingling sensation in the forearm, palm, and phalanx
This type of syndrome typically presents as an aching uncomfortable in the forearm with related paresthesias into the thumb, the pointer, and the index phalanx. The symptoms of this syndrome could mimic those of carpal tunnel syndrome with a few important points of differentiation. Both conditions might be exacerbated by repetitive activity. that people do not complain of night pain, which distinguishes this condition from carpal tunnel. Patients might note tenderness over a pronator’s teres muscle. Medial elbow tenderness is common. this syndrome might be related to weakness of the muscles in the forearm region innervated by a median nerve. Weakness is variable and is typically related to the sensation of grip clumsiness or/and a weakened pincher grip. The symptoms include aching pain in the forearm, weakness in the thumb and an index finger, tingling in the thumb and index finger, and numbness in the hand. Treatment such as includes rest, splinting, hand therapy, and surgery. Full recovery might take as long as six months, longer if there has been severe nerve damage.
- paresthesias in the thumb, index finger, middle finger, and radial half of the ring finger as seen in carpal tunnel syndrome
- in pronator syndrome, paresthesias usually made worse with repetitive pronosupination
- should have features differentiating from carpal tunnel syndrome (CTS)
- aching pain over the proximal volar forearm
- the sensory disturbances above the distribution of branch of the palmar cutaneous of the median nerve (palm of hand)
- arises 4 cm to 5 cm the proximal to the carpal tunnel
- lack of night symptoms
Prognosis
Pronator teres syndrome only needs pronator teres muscle release has a good recovery in a few cases, and patients back to light duty in approximately three weeks and routine duty in six weeks. Occupation therapy fastens recovery and is especially important for patients who underwent tendon transfers or have residual weakness. In these cases, patients might return to light-duty work in around six weeks to eight weeks and regular duty in ten weeks to twelve weeks.
Clinical Signs
Compression of the median nerve at the elbow could lead to pain and/or numbness in the distribution of the distal median nerve and weakness could develop in the FPL ( flexor pollicis longus ) muscles and FDP( flexor digitorum profundus ) muscles of an index finger and the pronator quadratus muscle. The physical determination of this would be tenderness over a PT( pronator teres ) muscle. and pain with resisted motion of forearm pronation. Weakness could be present with the thumb abduction as well as impairment to the pincer muscles. Sensation changes might also be experienced in the first 3 fingers and a palm.
Patients may present with these :
- volar pain of the proximal lower arm.
- paraesthesia of the volar surface of the forearm and the radial 3 digits and the radial aspect of the 4th digit.
- weakness, on the other hand, is variable, usually with unspecified grip clumsiness.
- the proximal volar surface of the forearm area is painful to palpation. and Tinel’s sign could be elicited on the palpation of the pronator teres muscle.
- simian hand deformity: not able to move the thumb away from the rest of the hand.
- the benediction sign: when endeavoring to form a fist, due to weakness in the flexion of radial-sided digits.
When Should People Consult a Doctor?
No one should live with pain. If individuals are experiencing symptoms of this Syndrome. and those who are interfering with their daily life, contact the GP. Pronator teres Syndrome could worsen if left unaddressed and could cause irreversible nerve damage. If it is diagnosed early, pronator teres syndrome could be treated with a range of non-surgical and surgical treatments. Most importantly, a medical professional can put the mind at ease and assist people to decide what to do next.
Differential diagnosis
Due to the same clinical presentation, a few authors combine pronator teres syndrome with the following proximal median nerve entrapment syndromes :
- Ligament of Struthers entrapment – median nerve compression by a ligament running from the medial epicondyle to a bony spur on a distal medial part of the humerus, which is present only in 1-2 % of the population. The pain in the forearm and paresthesias in the median-innervated digits are exacerbated by supination of the forearm and extension of the elbow (versus pronation in pronator teres syndrome). The radial pulse may also be reduced as the brachial artery runs next to the median nerve.
- The median nerve entrapment by hypertrophied bicipital aponeurosis (lacertus fibrosis) – This is fascia connecting the biceps to the ulna and overlies the median nerve in the proximal forearm. The pain in the forearm and paresthesias in the median-innervated digits are exacerbated by resisted flexion of the elbow with the forearm in supination.
- Median nerve compression by the sublime bridge of the flexor digitorum superficialis muscle – The pain in the forearm and paresthesias in the median-innervated digits is exacerbated by resisted flexion of the proximal interphalangeal joint of the middle finger while other fingers are held in the extension position.
The pronator teres syndrome should also be distinguished from carpal tunnel syndrome, median nerve entrapment at the wrist joint, which is the most common median nerve entrapment syndrome, as well as from the anterior interosseous nerve syndrome, the cervical radiculopathy, or the brachial plexus injury. The pronator teres syndrome has loss of sensation in the entire median nerve distribution versus CTS ( carpal tunnel syndrome ) where sensation is spared over the thenar eminence because the palmar cutaneous branch exits the median nerve the proximal to the carpal tunnel but the distal to the pronator teres muscle. In extra, pronation is spared in carpal tunnel syndrome, and nocturnal paresthesia symptoms are generally absent in pronator teres syndrome.
Nerve conduction study and amplitude of the median nerve might reduce in the forearm, but the distal motor and sensory latencies are normal in pronator teres syndrome except when there is associated carpal tunnel syndrome. due to coinciding symptoms, carpal tunnel syndrome is a few times diagnosed, and the proximal pronator teres syndrome is missed when both are present ( or current ) in the same limb. Thus in patients with carpal tunnel syndrome pronator teres syndrome should be ruled out particularly when the patient is a candidate for surgery. To distinguish the anterior interosseous nerve from pronator teres syndrome, the pronation should be demonstrated with the elbow flexed (pronator quadratus function) to evade the contribution of the pronator teres muscle, which is the primary muscle to pronate with the extension of the arm. Also, there is no sensory loss in anterior interosseous nerve syndrome (as it brings only deep sensory fibers to the wrist), and in a few cases, pronator teres syndrome might have only mild paresthesias (an abnormal sensation of the skin) in the median nerve distribution. In both cases, flexor pollicis longus and flexor digitorum profundus to digits 2 and 3 might be affected; but in the anterior interosseous nerve, the pronator quadratus does not weakness of the pronator teres muscle as the anterior interosseous nerve leaves median nerve distal to pronator teres muscle.
Clinically, in both cases, the patient presents with a not able to bend the distal phalanx of the thumb, index, and middle fingers and a weakness of pronation. In the case of brachial plexus injury or cervical radiculopathy, the examination might reveal a weakness in other muscles outside the median nerve territory. The Neck pain that radiates to the arm is the common complaint, suggesting cervical radiculopathy. One group of authors describes a neuralgic amyotrophy as a potential competing condition with pronator teres syndrome due to the same symptoms, but it generally involves multiple nerves, and pain is more commonly localized in the shoulder instead of in the forearm. Neuralgic amyotrophy is an idiopathic condition that generally improves spontaneously in 6 months to 12 months.
Pronator-teres syndrome must be differentially diagnosed from:
- other median nerve entrapment syndromes
- carpal tunnel syndrome
- anterior interosseous nerve syndrome (a.k.a. Kiloh-Nevin Syndrome)
- cervical radiculopathy
- thoracic outlet syndrome
- brachial plexus neuritis (Parsonage-Turner Syndrome)
- Pronator teres strain
What are the risk factors of Pronator Teres Syndrome?
Risk factors of pronator teres syndrome:
- Hypothyroidism.
- Diabetes.
- Alcoholism.
- Any type of trauma at an elbow.
How is the Pronator Teres Syndrome Diagnosed?
In addition to a careful history, the physical exam usually points to the diagnosis of pronator syndrome. Many examination tests performed by the clinician during the physical exam would clarify the exact cause of pronator syndrome. For example, if symptoms are reproduced when the elbow is flexed to 120 degrees against resistance, this is strongly correlated with median nerve compression by a structure called the ligament of Struthers. Same, the clinician may attempt to compress the medial nerve at the elbow by pressing on it. If numbness and tingling are reproduced within 30 seconds, it is strongly suggestive of pronator teres syndrome.
An X-ray of the elbow would be taken to rule out any bony abnormality which might be leading to symptoms. Sometimes, Magnetic resonance imaging would be needed to obtain more detail about the soft tissues affecting the median nerve. The nerve conduction studies and electromyography are performed to ensure a diagnosis.
Nerve conduction studies must be done in pronator teres syndrome to rule out other neuropathies, but they seldom show abnormalities 1. Sensory and motor amplitudes are decreased more than conduction velocities, mostly in patients with severe and axonal symptoms. Electromyography (EMG) abnormalities happen in flexor pollicis longus and flexor digitorum profundus to digits 2 and 3, less often in the flexor digitorum superficialis and abductor pollicis brevis, and only rarely in pronator teres because compression at the site most usually happens distal to its innervation. Suppose any of the median muscles are not normal. In that case, other muscles innervated by the same myotomes as the proximal median muscles but supplied by a different nerve should be tested to exclude more proximal lesions within a brachial plexus or cervical roots. a few authors report not normal electrodiagnostic findings in 10% of pronator teres syndrome only.
Pronator teres syndrome among other entrapments within the upper limb also could be diagnosed by ultrasound and magnetic resonance imaging, but ultrasound is advantageous due to its dynamic character and lower cost. Several studies with an ultrasound evaluation of the median nerve between the humeral and ulnar heads of pronator teres concluded that the cross-sectional area of MN positively correlates with severity, duration of the symptoms, and nerve conduction failure.
Pronator Teres Syndrome Test
The Pronator teres syndrome test is an elbow examination used to test for median nerve compression at the pronator teres muscle.
Procedure:
The patient was seated with the elbow fixed at 90 degrees of flexion. The examiner then places one hand on the patient’s elbow for stabilization and the other hand grasping the patient’s hand in a handshake position. The individual maintains this position as the practitioner attempts to supinate the patient’s forearm (forcing the client to contract the pronator muscles). While maintaining the resistance against pronation, the healthcare provider extends the individual’s elbow. If an individual’s pain or/and not comfort is reproduced, there is a good chance of median nerve compression by a pronator teres muscle. The patient should keep the elbow relaxed during the test because holding the elbow firmly in flexion would not allow elbow extension.
Purpose
The purpose of this test is to assist differentiate the difference between these two types of syndromes ( like Pronator Teres Syndrome and Carpal Tunnel Syndrome.)
Physical exam
- provocative tests are specific for various sites of entrapment
- positive Tinel sign in the proximal anterior forearm but no Tinel sign at the wrist nor provocative symptoms with wrist flexion as would be seen in Carpal Tunnel Syndrome
- the resisted elbow flexion movement with forearm supination movement (compression at bicipital aponeurosis)
- the resisted forearm pronation movement with the elbow extension position(compression at two heads of pronator teres)
- the resisted contraction of flexor digitorum superficialis to the middle finger (compression at flexor digitorum superficialis fibrous arch)
- possible coexisting medial epicondylitis
Imaging
- Radiographs
- recommended views
- elbow films are mandatory
- findings
- may see the supracondylar process
Radiographic features
these are the two imaging modalities. such as Ultrasound and Magnetic resonance imaging. which best lends itself to investigating entrapment syndromes. Next to directly visualizing direct causes [e.g. the primary nerve or/and sheath tumors, ganglion cysts, osseous spurs, and anatomical alternatives or variants (e.g. Gantzer’s muscle), recognizing pathological muscle signal patterns on Magnetic resonance imaging can inversely point to the affected nerve.
Magnetic resonance imaging
In Pronator teres syndrome, the pronator teres (PT), flexor carpi radialis (FCR), palmaris longus (PL), and flexor digitorum superficialis (FDS) will reveal hyperintense signal changes secondary to denervation edema, which could happen 24-48 hours after an inciting event; electromyography, the most sensitive neurophysiological study for inferring denervation syndromes, requires 7 days -14 days to show pattern changes.
Studies
- EMG and NCV
- may be useful if positive but are usually inconclusive
- and may exclude other sites of nerve compression or determine the double-crush syndrome
Differential diagnosis:
- Anterior interosseous nerve entrapment.
- Carpal tunnel syndrome.
- Pronator teres strain.
- Cervical Radiculopathy.
- Thoracic Outlet Syndrome.
- Brachial Plexus Neuritis.
Is pronator teres syndrome the same as carpal tunnel syndrome?
Not really. Although the symptoms might be similar, the causes are very different and require. different treatment approaches. Compression of the median nerve leads to carpal tunnel syndrome by inflamed tendons where the wrist meets the hand; pronator teres syndrome is compression of the median nerve near an elbow joint due to tight muscles, adhesions, and/or the presence of scar tissue it compresses the nerve.
The main difference between their etiologies lies in the area of compression: pronator teres could be caused by compression of the MN as it passes through the anatomical structures of the forearm; carpal tunnel syndrome is caused by compression at the carpal tunnel.
PTS is distinct from carpal tunnel syndrome in that it develops when the median nerve is compressed in the upper forearm region as opposed to the wrist and hand. When the median nerve is affected or involved in the upper forearm, it becomes entrapped around the elbow and the upper forearm, leading to a range of symptoms.
How is the Pronator Syndrome Treated?
What can the athlete do?
- Rest from activities that might be contributing to the condition.
- Apply ice to ease pain and swelling. Cold therapy or ice could be applied for 10 to 15 minutes every hour initially reducing to 3 or 4 times a day as needed.
What can a sports injury professional do?
A doctor might prescribe painkillers or anti-inflammatory medications such as ibuprofen. They might use electrotherapy treatments such as ultrasound or laser. Sports massage might be useful to reduce muscular tension. A nerve block or corticosteroid injection might be used if symptoms do not improve.
- A doctor might prescribe painkillers or anti-inflammatory medications such as ibuprofen.
- They might use electrotherapy treatments such as ultrasound or laser.
- Sports massage might be useful to reduce muscular tension.
- A nerve block or corticosteroid injection might be used if symptoms do not improve.
- Surgery is very sometimes used to release tight or abnormal structures.
- Pronator muscle stretches might be helpful.
- Acupuncture might be effective in releasing muscular tension.
To make a diagnosis, one of our reconstructive hand surgeons would perform a physical examination. and take imaging tests to thoroughly evaluate what might be leading to their symptoms. this syndrome is most generally determined based on the physical examination, but imaging tests, like an X-ray, Magnetic resonance imaging, or nerve conduction studies might assist a doctor in better understanding the structure of the area and if another problem might be contributing. For mild cases to moderate cases of this syndrome, the surgeons would first recommend conservative treatments to attempt resolution of the condition. These non-surgical methods might include one or more of the following:
- Rest from the activity leads to symptoms
- Splinting to prevent the forearm from rotating
- Anti-inflammatory pain medications
- Hand therapy
The progress would be monitored over three to six months; most of the time the symptoms would resolve. If these methods are not enough to enhance the condition—or initial symptoms include problems moving the arm or hand—surgery might be recommended to ease the pressure on the median nerve. This typically entails a minimally invasive procedure developed to decompress the nerve at the elbow to restore optimal function. The most beneficial treatment option for the condition would be determined once the surgeon has had the opportunity to assess the symptoms as well as the results of the imaging tests.
Conservative management might be effective in 50–70% of cases with extremity rest and non-steroidal anti-inflammatory drugs. Corticosteroids have also been used. The surgical decompression is indicated in space-occupying lesions and failure of conservative management over twelve weeks, with success rates of up to 90%.
An effective conservative treatment strategy includes rest, modalities, muscle active release, and nerve gliding exercises. Perhaps the more important aspect of management is the avoidance of repetitious forceful gripping. Ice packs or ice massage directly around the pronator teres muscle might provide benefits. The use of ultrasound and electrical stimulation has shown advantages for the management of other nerve pathologies. and their use might be advantageous in the management of pronator teres syndrome. One study demonstrated that in 50% of pronator teres syndrome, some people reported resolution of symptoms within four months of initiating care. the surgical decompression of the median nerve is a consideration when non-surgical treatment fails.
Nonoperative
The vast majority of individuals with pronator syndrome respond well to conservative treatment. Three months to six months of rest from the offending activity, splinting, and use of non-steroidal anti-inflammatory drugs to diminish inflammation under the watchful eye of a hand specialist may be all that is required for symptoms to resolve. Treatment is conservative, including rest, ice, and anti-inflammatory drugs or medications. Stretching and strengthening exercises assist to diminish the load through the tendon. Cortisone injections could be used for refractory pain.
- rest, splinting, and NSAIDS for 3-6 months
- indications
- mild to moderate symptoms
- technique
- a splint should avoid forearm rotation
Operative
If motor deficits such as weakness or paralysis are noted on a physical examination, or if the patient does not respond to conservative methods, surgery might be required to treat pronator syndrome. Surgery is aimed at decompressing the nerve at the actual place of the entrapment. Postoperatively, a long arm splint is placed. Eight days to ten days thereafter, the splint is removed, sutures are removed, and the patient is transitioned to a removable splint. The splint is worn at night. and during every day as endured for a minimum of two weeks. Physical therapy is prescribed and generally lasts two months.
- surgical decompression of the median nerve
- indications
- only when nonoperative management fails for 3 months to 6 months
- technique
- decompression of the median nerve at all five possible areas of compression
- outcomes
- of surgical decompression is variable
- 80% of patients have relief of symptoms
Physiotherapy treatment for pronator teres syndrome:
- Take a rest in between the activity.
- Apply an Ice massage over the pain area.
- Stretching of the pronator teres muscle.
- Stretching of flexor muscles of the wrist.
- Nerve flossing exercise for the median nerve.
- Strengthening exercise of the supination muscles.
- Massage technique.
- Kinesio taping technique.
- Dry needling technique.
- Myofascial release of pronator teres.
- Electrical modalities like TENS, and the US, diminish the pain and spasm, and tingling sensation.
- Wearing splint.
- Patient education and advice on Modified activity/sport.
Resting:
It is essential to prevent overusing the affected arm for the repetitive activity of grasping and forearm rotation movement. Hence, an elbow orthosis is useful to rest the elbow in a bending position, and the forearm in a neutral position. patient wear it the whole day for at least two to four weeks. For heavy computer users, therapists should advise using an ergonomic split keyboard and vertical mouse, which assist to decrease full pronation of the forearm when typing and mousing.
Therapeutic exercises:
Median Nerve Flossing Exercise:
- Sit on the table and reach the affected arm out to the side, and bring it with the shoulder, the hand facing the floor.
- Flex a hand and pull the fingers up toward the ceiling.
- Bend an arm and bring the hand toward a shoulder.
- Repeat it 5 times.
Pronators Stretching:
- Pronator Teres Stretch. Stretching the pronator teres muscle in the forearm would assist lengthen this muscle. and prevent muscle tightness associated with pronator teres syndrome.
- Standing with the back facing the door.
- Raise the arm backward (shoulder extension) as much as possible, and keep the elbow straight.
- Grasping the doorframe with the thumb pointing down.
- Rotate the arm externally.
Myofascial Release:
- First Maintain the elbow bend, palm facing up. Put the thumb over the affected forearm, near an elbow
- Rotate the palm facing downward, so that palpate the pronator teres muscle be
- After the palpation of the tender point, press for five seconds without triggering any symptoms such as tingling or numbness sensation.
- Rotate the forearm repeatedly. (turning the palm up and down) this movement repeats ten times while the thumb is still on the belly point.
Standing palm press (Flexor muscles stretching and Extensors muscles stretching):
- The forearm muscles and hand muscles would be stretched along with the nerves in the arm.
- Stand the affected side of the body facing the wall side. the feet should be slightly apart.
- Press that hand into the wall, while maintaining the torso upright position and the arm should be straight.
- Fingers should be pointed up.
- Pull the shoulder or body back and hold the stretch for five deep breaths.
- Change the finger’s position to be pointed downward without hunching the shoulder and another position will be similar.
- Maintain the stretch for five deep breaths.
Standing curl Exercise:
- First, stabilize the pelvis and torso and it assists to work all the muscles in the shoulders and arms.
- Rotating movements of the arms enhance muscle strength and movement in the forearm.
- Stand with legs shoulder-width apart, maintain the dumbbell in one hand which hands facing toward the legs.
- Flex the arms to the shoulders. and turn the hands that face the shoulders.
- Rotate the arms and the hands so that the knuckles are facing toward the body. then back to the beginning position.
- Repeat this movement ten times.
Massage Techniques:
- In complete the pronator teres syndrome, the involved muscles such as the PT (pronator teres), FCR (flexor carpi radialis), PL (palmaris longus), FDS (flexor digitorum superficialis), along with muscles innervated by the anterior interosseous nerve. To massage the Pronator Teres muscle, people will require a ball and a table. Place the ball over the muscle in the forearm. then place the hand over a table. Apply pressure on that hand with the other arm and hold, keeping the wrist relaxed.
- Massage techniques can assist to reduce tension in the pronator teres muscle so which reduces compression on the median nerve. Called “releasing” the pronator teres.
- These techniques performed by a trained professional could lengthen the muscle.
- The practitioner executes contact inhibition and drained the tension in which areas or sites are tight.
- This technique assists to work stubborn tension out of the muscle and relieves compression of the underlying nerve.
Kinesio Taping:
- Attach the tape over the outside of the mid-forearm, and then pull it diagonally to the inside of the forearm.
- Apply the Kinesio tape over a pinky side of a wrist and stretch it towards an inside of an elbow.
- This tape is applied for two or three days and then it removes.
Dry needling:
- The dry needling technique is used to decrease pain, decrease activation of resting muscle and decrease muscular tension.
- This technique used various size needles and applies them to the pain area.
Patient Education:
During conservative treatment, patients should be advised to minimize their related activities that involve frequent forearm pronation movement.
These activities include:
- Hammering.
- Ladling food.
- washing dishes.
- Playing table-tennis.
- Pouring drinks, activity performed by waitresses.
- Carry the books frequently performed by librarians.
- Twisting the clothes.
What is the Pronator Teres Syndrome Prognosis?
Pronator teres syndrome only needs pronator teres muscle release has a good recovery in most cases, and patients return to light duty in approximately three weeks and regular duty in six weeks. Occupational therapy fastens recovery and is especially important for patients who underwent tendon transfers or have a residual weakness. In these cases, patients might return to light duty work in approximately six weeks to eight weeks and regular duty in ten weeks to twelve weeks.
What is the complication of pronator teres syndrome?
After surgical treatment complication is very rare. In one research study, 72 patients were treated with the pronator teres syndrome, and no complications were recorded during an operation. And after the postoperative treatment satisfaction rate is 59 percent. Theory basis complications of surgery include:
- Any Infection.
- Any type of hematoma formation.
- Nerve injury.
- Scar tissue formation.
DISCLAIMER:
This article is intended or purposeful for your general informational purposes only and does not address particular circumstances. it is not a substitute for professional advice(or guidance) or help( or assistance) and should not be relied on to make decisions of any kind. A few or any actions you take upon the information presented in this article are strictly at your own risk and responsibility.
FAQs
Which of following the signs and symptoms are typical for the pronator teres syndrome?
Signs & Symptoms.Aching pain in the forearm. Tingling in the thumb and index finger. Numbness in the hand. and the thumb and index finger in the weakness.
How do you test for pronator teres syndrome?
Pronator Teres Syndrome Test. The healthcare provider stabilizes the elbow with one hand and asks the individual to pronate his hand against the practitioner’s resistance. The clinician extends the person’s elbow while maintaining this resistance. the reproduction of the symptoms suggests the including of the pronator teres muscle.
What nerve is damaged in pronator teres syndrome?
Pronator teres syndrome (PTS) is a rare disease caused by compression of the median nerve (MN) by the pronator teres (PT) muscle or other adjacent anatomical structures in the upper forearm. The classical presentation of Pronator teres syndrome is that of forearm pain with sensory changes in the median nerve territory.
How do you relieve pronator teres muscle pain?
Pronator Teres Stretch. Stretching the pronator teres muscle in the forearm would assist lengthen this muscle. and prevent muscle tightness associated with pronator teres syndrome. …
Flexor Stretch. …
Nerve Flossing. …
Standing Palm Press. …
Supinator Strength Training. …
Standing Curl and Press. …
Myofascial Release.
What medication is used for pronator teres syndrome?
A doctor might prescribe painkillers or anti-inflammatory medications such as ibuprofen. They might use electrotherapy treatments such as ultrasound or laser. Sports massage might be useful to reduce muscular tension. A nerve block or corticosteroid injection might be used if symptoms do not improve.
How to differentiate between PTS (pronator teres syndrome) and CTS (carpal tunnel syndrome)?
The main difference between their etiologies lies in the area of compression: pronator teres could be caused by compression of the MN as it passes through the anatomical structures of the forearm; carpal tunnel syndrome is caused by compression at the carpal tunnel. Pronator teres syndrome (PTS) changes from carpal tunnel syndrome as it happens when the median nerve is compressed in the area of the upper forearm part instead of in the wrist and the hand. When the median nerve is affected or involved in the upper forearm, it becomes entrapped around the elbow and the upper forearm, leading to a range of symptoms.
What muscles are affected in pronator teres syndrome?
In complete the pronator teres syndrome, the involved muscles such as the PT (pronator teres), FCR (flexor carpi radialis), PL (palmaris longus), FDS (flexor digitorum superficialis), along with muscles innervated by the anterior interosseous nerve.
How do people massage the pronator teres muscle?
In complete the pronator teres syndrome, the involved muscles such as the PT (pronator teres), FCR (flexor carpi radialis), PL (palmaris longus), FDS (flexor digitorum superficialis), along with muscles innervated by the anterior interosseous nerve. To massage the Pronator Teres muscle, people will require a ball and a table. Place the ball over the muscle in the forearm. then place the hand over a table. Apply pressure on that hand with the other arm and hold, keeping the wrist relaxed.
How long does it take to recover from a pronator teres tear?
The symptoms include aching pain in the forearm, weakness in the thumb and an index finger, tingling in the thumb and index finger, and numbness in the hand. Treatment such as includes rest, splinting, hand therapy, and surgery. Full recovery might take as long as six months, longer if there has been severe nerve damage.
Why does my pronator teres muscle hurt?
Entrapment of the median nerve (MN) between the two heads of a pronator teres muscle (PTM) can reason to pain and functional disability in the arm and hand and can lead to referred pain and neurological symptoms in a hand. This is called Pronator teres syndrome (PTS).
What nerve controls the pronator teres muscle?
The pronator teres (PT) muscle is a forearm flexor with a radial head and ulnar head. That is innervated by a median nerve (MN), which passes between these heads.
How do you treat a teres muscle injury?
Treatment is conservative, including rest, ice, and anti-inflammatory drugs or medications. Stretching and strengthening exercises assist to diminish the load through the tendon. Cortisone injections could be used for refractory pain.
Can you pull your pronator teres?
The pronator teres muscle strain is a few times sporting injuries reported thus far only in cricket and golf participants. The injury appears to happen when the sporting club or/and racket strikes the base during a forceful swing. and leads to the elbow experiencing an eccentric force during resisted elbow flexion and elbow pronation.
What is a common injury to the teres minor?
The teres minor muscle is the component of the rotator cuff least such as to tear. Injuries to the teres minor muscle commonly happen either in the setting of massive rotator cuff tears. or/and following posterior subluxation/dislocation.
What is the Pronator Teres Syndrome Prognosis?
Pronator teres syndrome only needs pronator teres muscle release has a good recovery in most cases, and patients return to light duty in approximately three weeks and regular duty in six weeks. Occupational therapy fastens recovery and is especially important for patients who underwent tendon transfers or have a residual weakness. In these cases, patients might return to light duty work in approximately six weeks to eight weeks and regular duty in ten weeks to twelve weeks.
When Should People Consult a Doctor in Pronator Teres Syndrome?
No one should live with pain. If individuals are experiencing symptoms of this Syndrome. and those who are interfering with their daily life, contact the GP. Pronator teres Syndrome could worsen if left unaddressed and could cause irreversible nerve damage. If it is diagnosed early, pronator teres syndrome could be treated with a range of non-surgical and surgical treatments. Most importantly, a medical professional can put the mind at ease and assist people to decide what to do next.
What are the risk factors of Pronator Teres Syndrome?
Risk factors of pronator teres syndrome:
Diabetes.
Hypothyroidism
Alcoholism.
Any type of trauma at an elbow.





4 Comments