Evidence-Based Practice (EBP)
What is Evidence-Based Practice?
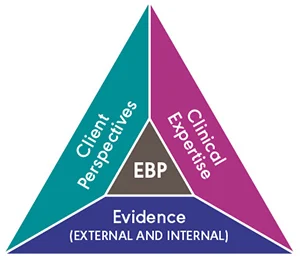
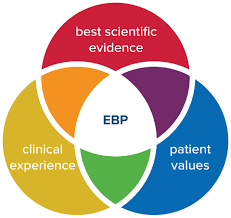
Evidence-based practice is the integration of great research evidence with the best available scientific research, clinical experiments, and patient values. which applied by healthcare workers will ultimately lead to improved patient health.
These 3 variations of evidence clinical expertise, scientific research, and patient values and circumstances form the basis on which you can decide which is the best physical therapy treatment plan for any given diagnosis. If you are an evidence-based therapist, your decisions will be on these three types of evidence. The goal of this therapist is to make sure that the patient’s condition is treated by the greatest available research to give more benefits that patients receive from the therapist. Evidence Base Practice gives a structured method for thinking about and collecting the different types of evidence preferred to make clinical decisions.
Evidence thought can be coming from these three different sources:
- Scientific research
- Clinical expertise
- Patient values and circumstances
Scientific research:
This evidence is practical evidence needed through systematic testing of a theory. When describing research evidence to a patient, it was difficult to speak in simple language and follow up with questions to make sure the patient corporate. Therapists have the main responsibility to identify, evaluate, and summarize research evidence concerning a patient’s care.
Clinical expertise:
It refers to implicit and explicit knowledge about physiotherapy diagnosis, management, prevention, and prognosis gained from cumulative years of curing patients with disease and injury and working on it and refining that care. This refers to the clinician’s cumulated education, clinical skills, and experience.
Patient Values and Circumstances:
The patient caregivers create the most vital pillar of evidence in the decision-making process. Evidence taken from the patient can be divided into two parts: values and circumstances. Patient values add the beliefs, preferences, expectations, and cultural identity that the patient brings to the therapy atmosphere. Fundamentally, values are the main principles that guide a person’s life and life choices.
It is the integration of these three components that define a clinical decision evidence-based. This consolidation can be effectively achieved by carrying out the 5 following sequences of evidence-based practice.
Evidence-based practice (EBP) is a problem-solving approach to giving health care that united the great evidence from researchers and patient care data with clinician expertise and patient preferences and values. When treatment given by the health care worker is a supportive organizational culture, the highest quality of care is. then best patient outcomes can be achieved.
The main aim of this series is to give healthcare professionals to knowledge and skills they need to apply Evidence Base Practice constantly. These articles will appear every month to allow you time to incorporate information when you work toward applying Evidence Base Practice in your clinical setup.
Many Research shows that evidence-based practice gives higher quality care, improved patient outcomes, decreased costs, and greater health care satisfaction than traditional approaches to care. Despite these favorable findings, many professionals remain inconsistent in their implementation of evidence-based care. Moreover, some doctors, whose education predates the inclusion of Evidence Base Practise in their curriculum, still lack the computer and Internet search skills necessary to apply these practices.
Why is Evidence-Based Practice Important?
Evidence-Based Practice is important because it prefers to give the most effective care that is available, and plan to improve patient health. Patients will expect to get the most effective treatment based on the best available research. Evidence-Based Practice encourages an attitude of inquiry in health professionals and starts us thinking about it: Why am I performing this in this way? Is there any evidence that can guide me to perform this more easily and helpful? As a healthcare professional, part of providing a professional service is more important. this is our practice and this is informed by the best available evidence. Evidence-Based Practice also plays an important role in ensuring that limited health resources are used wisely and that relevant evidence is considered when decisions are made about replacing health services.
What happened before Evidence-Based Practice?
Before Evidence-Based Practice health care professionals relied on the advice of more experienced teammates, most of taken the face value, their intuition, and on what they were taught as students. Experience is subject to flaws of bias and what we learn as students can quickly become outdated. Relying on older, more knowledgeable colleagues as the sole information source can provide dated, biased and incorrect information.
This is not to say that clinical experience is not important – it is part of the definition of EBP. However, rather than relying on clinical experience alone for decision-making, health professionals need to use clinical experience together with other types of evidence-based information.
Is not all Published Research of Good Quality?
However, Not all research is of sufficient quality to give clinical decision-making. Therefore you have to critically approve evidence before using it to inform your clinical decision-making. The 3 major aspects of evidence that you need to critically appraise are:
- Validity – can you believe it?
- Impact – These results are clinically important?
- Applicability – can you apply it to your clinical setups?
How do you apply Evidence Bases Practice in clinical practice?
Researching all available evidence on a subject would be a nearly not possible task. Many Evidence-Based practice processes have been found to help healthcare professionals to implement Evidence Base Practice in the clinic or hospital.
The most common process follows these six steps for EBP:
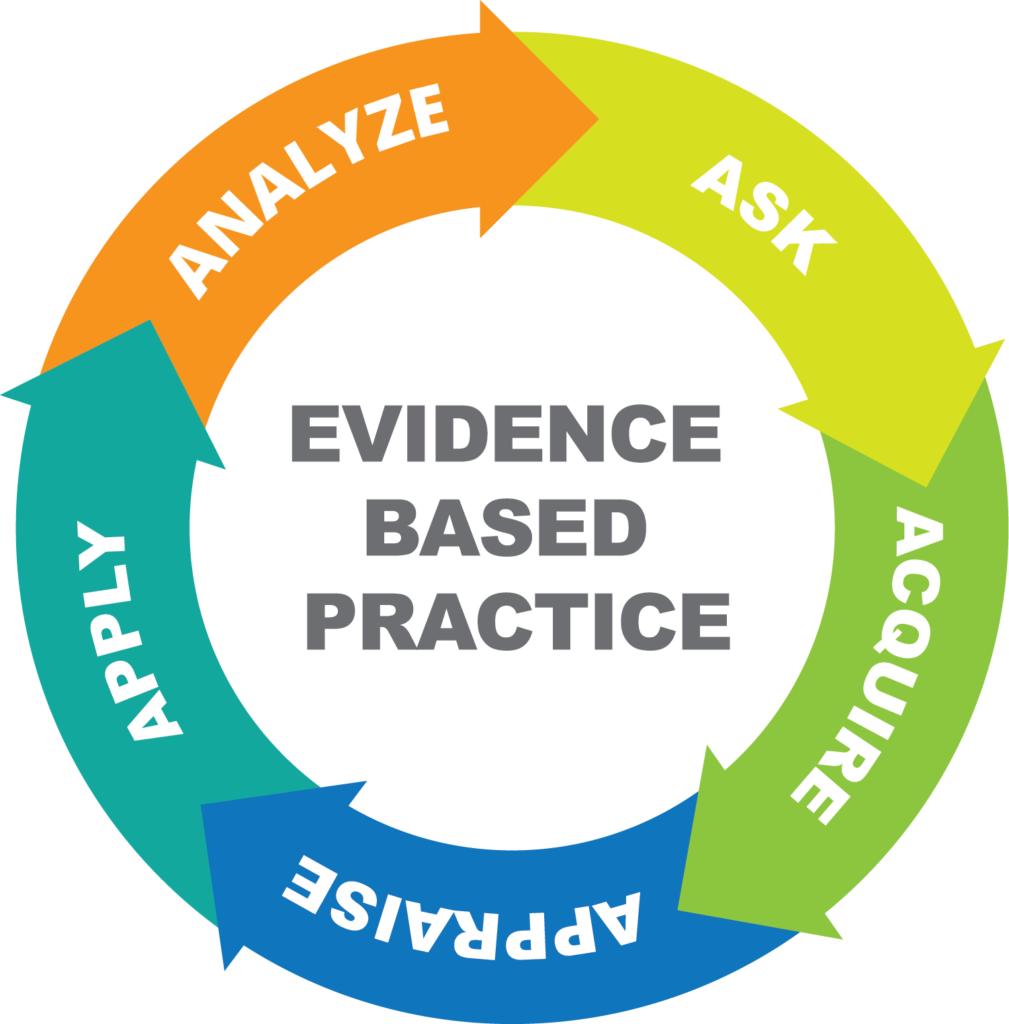
- Ask a question:
There has something in your clinical setup that you are wondering about? Perhaps you wonder if new research is more helpful than the one currently used. Ask yourself: What works great and what can be improved in the treatment? And, more importantly, Why it? Investigate the activity and workflow that impact, or are impacted by, the noticed practice gap. This formal will be used called a Pico. - Acquire:
the present evidence. You will do this by presenting a literature search. You will search with guided clinical questions. - Appraise:
the literature or in other words, sort, read, and critique peer-reviewed literature. - Apply:
What you find in clinical decision-making. Integrate the research with clinical expertise and patient preferences and values. Then make evidence-based recommendations for regular practice. - Evaluate:
your observational results. document your approach and review data. Be sure to add any revisions or changes in your practice. Keep a note of the outcomes of your intervention. Evaluate and summarize the outcome. - Disseminate:
the information. Announce the main results of your research with your colleagues. Sharing new ideas will help to promote best clinical practices and prevent duplicate practices. There have many added resources that support or oppose your practice.
We have to apply EBP in daily participating in project-based work, integrating EBP into our daily life. then this will help us achieve the best possible patient benefits. This required asking proper questions about our practice.
This is important to note that our evidence practice will be applied individually at the bedside, working combining as a team is more likely to result in lasting improvement.
The Problem with EBP:
The evidence-based “quality mark” has been misappropriated by missed interests The volume of evidence, especially clinical guidelines, has become not manageable Statistically significant importance can be marginal in clinical set-ups Inflexible rules and technology-driven prompts may induce care that is management driven rather than patient-centered Evidence-based rules mostly map poorly to complex multi morbidity
Implementation Strategies for Evidence-Based Practice
The Implementation Strategies for Evidence-Based Practice guide is set to help healthcare professionals who are responsible for EBP choose implementation tactics that would make it easier for clinicians and practice teams to help in clinical practice recommendations into standard procedures. Strategies are selected and positioned to enhance the movement through four phases of implementation: creating awareness and interest, commitment and building knowledge, adoption and promoting action, and pursuing integration and sustainability.
- Before you start EBP –a few important considerations must be
- Do you have more than just evidence?
- Patient Feedback
- The patient design explores the thumb
Research findings, in the absence of other considerations, should be used independently to justify a change in practice. These factors may be considered during research:
Patient values and preferences
- Experience of the health care provider
- Patient assessment and laboratory findings
- For Evidence-Based Practice strategies to result in the best patient benefits, all of these things must be considered.
For more helpful tips to get started, read and ask these four questions before starting any improvement.
To execute Evidence-Based Practice, we also need some consideration from the administration and institutional resources if the implementation of the project work. For illustrate, suppose there is a strong body of evidence showing a decreased incidence of depression in pregnant female who receives cognitive therapy sessions when they are hospitalized for long periods. While this may be a great idea, budget constraints may prevent hiring a therapist to apply this therapy.
While you are thinking about the resources, think about your helpers, or human resources.
- Who in your organization can help you with the research?
- Are there any content experts or key stakeholders that you can involve early on?
- can you have an assessment to access the data and a plan for measuring the research progress?
Just like the research process, we must evaluate and monitor any changes in results after implementing an Evidence-Based practice project so that positive effects are carried out and negative effects are sorted out. An intervention may be highly effective in a rigorously controlled trial, but that does not always indicate it will work the same way in your clinical setting or for your patients.
Conclusion
The goal of conducting Evidence-Based Practice is to work on current knowledge and connect it with patient preferences and clinical expertise to give and improve standard care processes and, ultimately, patient health.
FAQ
Which are good Evidence-based practice questions?
How can you brief the problem or a group of patients similar to research? What is the main investigation, prognostic factor or exposure am I considering? Is there any alternative to compare with this same intervention? how to accomplish, measure, improve, or affect?
Which are the requirements for Evidence-based practice?
Which are the requirements for Evidence-based practice?
There have three elements to apply to evidence base practice
Best Available research.
Clinical Knowledge and Skills to apply it.
Patient’s convenience and Needs.
What are the five A’s for Evidence-based practice?
This process involves 5 distinct steps which we name the five ‘A’s: Ask, Audit, Access, Appraise, and Apply.
What is the main purpose of evidence-based practice?
Evidence Base practice is a practice used to review, analyze, and translate the latest scientific research. The aim of this is to quickly incorporate the best available technique, along with clinical experience and patient preference, into clinical setup, so the therapist can make informed patient-care decisions.
Which barriers are implemented in evidence-based practice?
conducting a study on primary care and identifying the main barriers to Evidence Base Practise, namely organizational issues regarding price, changes in work, time limitations, patient compliance, and lack of motivation to apply EBP.
Which four pillars are used in evidence-based practice?
These four pillars are used in EBP clinical expertise, research evidence, the patient’s values and circumstances, and the practice context.