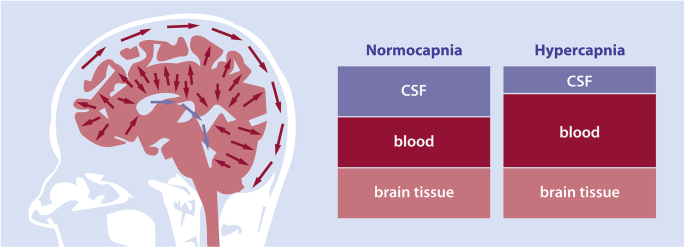
Hypercapnia
What is Hypercapnea?
Hypercapnia (from the Greek word hyper means too much and kapos means smoke), also called hypercarbia (CO2 retention) is a disease of abnormally increased levels of carbon dioxide (CO2) in the blood.
Carbon dioxide is a gaseous outcome of the body’s metabolism and is generally expelled via the lungs. Carbon dioxide may collect in any disease that generates hypoventilation, a decrease of alveolar ventilation (the clearance of air from the small sacs of the lung where gas is exchanged in a particular area) as well as resulting from inhalation of CO2. The incapability of the lungs to clear carbon dioxide, or inhalation of raised levels of CO2, conducts to respiratory acidosis. Ultimately, the body compensates for the increased acidity by retaining alkali in the kidneys, a process called metabolic compensation.
Acute hypercapnia is known as acute hypercapnic respiratory failure (AHRF) and is a medical emergency as it normally happens in the context of acute disease. Chronic hypercapnia, where metabolic compensation is generally present, may generate symptoms but is not normally an emergency. Depending on the scenario both conditions of hypercapnia may be managed with drugs, with mask-based non-invasive ventilation, or with mechanical ventilation.
Hypercapnia is a danger of underwater diving associated with breath-hold diving, especially on rebreathers, scuba diving, and deep diving where it is associated with raised breathing gas density due to the high ambient pressure
Epidemiology
Hypercapnia is a syndrome of disease instead than a single condition etiology. As such the same epidemiology is connected to the particular inducing pathology.
What are the symptoms of hypercapnia?
Symptoms of hypercapnia can occasionally be mild. Your body can fast properly these symptoms to breathe nicely and balance your CO2 levels.
Mild symptoms of hypercapnia contain:
- flushed skin
- drowsiness or incapability to focus
- mild headaches
- feeling disoriented or dizzy
- feeling short of breath
- being abnormally tired or exhausted
If these symptoms continue beyond a few days, notify your doctor. They can specify whether you’re experiencing hypercapnia or another underlying disease.
Severe symptoms
Severe hypercapnia can pose more of a danger. It can control you from breathing correctly. Unlike with mild hypercapnia, your body can’t fix extreme symptoms fast. It can be seriously harmful or fatal if your respiratory system closes down.
Visit your doctor right away if you have one or more of the subsequent symptoms, particularly if you’ve been analyzed with chronic obstructive pulmonary disease (COPD):
- unexplained feelings of confusion
- abnormal feelings of paranoia or depression
- abnormal muscle twitching
- irregular heartbeat
- hyperventilation
- seizures
- panic attack
- passing out
What else can cause hypercapnia?
Hypercapnia can have many different causes besides COPD, also. For instance:
Sleep apnea controls you from breathing correctly while you sleep. This can maintain you from bringing oxygen into your blood.
Being overweight or obese can also maintain you from getting sufficient air due to the pressure placed on your lungs by your weight.
Activities that may restrict you from breathing in the fresh air, like scuba diving or being on a ventilator during anesthesia, can also generate hypercapnia.
Physical diseases or events that generate your body to create more CO2, like having a fever or eating a lot of carbs, can both raise the quantity of CO2 in your bloodstream.
Gas exchange issues
Some underlying diseases can generate dead space in your body. This suggests that not all of the air you breathe in brings a role in your breathing process. When this occurs, it’s generally because a portion of your respiratory system isn’t working correctly. In many patients, this includes your lungs not doing their role in gas exchange.
Gas exchange is the method by which oxygen enters your blood and CO2 leaves your body. Issues can be generated by diseases such as pulmonary embolus and emphysema.
Nerve and muscular issues
Nerve and muscular diseases can also generate hypercapnia. In some diseases, the nerves and muscles that assist you to breathe may not work correctly. These can contain Guillain-Barr syndrome, an immune system disease that weakens your nerves and muscles. This disease can involve your capability to get sufficient oxygen and can lead to too great CO2 in your bloodstream. Muscular dystrophies, or diseases that generate your muscles to weaken over time, can also cause it hard to breathe and get adequate oxygen.
Genetic causes
In rare patients, hypercapnia can be caused by a genetic disease in which your body doesn’t create adequately a protein known as alpha-1-antitrypsin. This protein arrives from the liver and is used by your body to maintain the lungs healthy.
Brain Disorders
Diseases that damage your brain’s capability to control breathing may result in CO2 collection in your blood (central hypoventilation). Your respiratory control can be damaged by:
Brainstem stroke
Medicine overdoses, like with an opioid or benzodiazepine (used to manage anxiety)
Nervous system diseases such as encephalitis (a brain infection) or a large stroke
Neuromuscular conditions like amyotrophic lateral sclerosis (ALS) and muscular dystrophy can create a struggle to breathe, resulting in a buildup of blood CO2 levels.
Myasthenia gravis is another neuromuscular reason for hypercapnia.
The onset of Lung Disease
Lung conditions can interrupt CO2 removal. A situation known as ventilation/perfusion (V/Q) mismatch happens when you have extreme lung damage that controls the flow of blood and/or air in your lungs.
The subsequent chronic diseases can cause CO2 gas to build up in the body:
- Chronic obstructive pulmonary disease (COPD)
- Bronchiectasis
- Emphysema
- Interstitial lung condition (involving pulmonary fibrosis)
- Cystic fibrosis
Whos at risk for hypercapnia?
Some risk factors for hypercapnia, particularly as an outcome of COPD, contain:
smoking cigars, cigarettes, or pipes heavily
age, as many diseases that generate hypercapnia, are progressive and generally don’t start to show symptoms until after age 40
having asthma, particularly if you also smoke
breathing in fumes or chemicals in workplace environments, like warehouses, factories, or electrical or chemical plants
A late diagnosis of COPD or another disease that generates hypercapnia can also raise your risk. Visit your doctor at least once per year for a full physical examination to make certain you’re maintaining an eye on your general health.
Differential Diagnosis
There is a myriad of condition pathologies that conduct hypercapnia. These contain:
- Acute respiratory distress syndrome
- Asthma Exacerbation
- Central or obstructive sleep apnea
- Chronic obstructive pulmonary disease chronic state
- Chronic obstructive pulmonary acute exacerbation
- Drug overdose
- Exogenous CO2 inhalation
- Head or cervical cord injury
- Myasthenia gravis
- Myxedema
- Obesity-hypoventilation syndrome (Pickwickian syndrome)
- Polyneuropathy
- Poliomyelitis
- Primary muscle diseases
- Porphyria
- Primary alveolar hypoventilation
- Pulmonary edema
- Tetanus
Diagnosis
Frequently, the symptoms of mild hypercapnia are simple sufficiently for an experienced healthcare provider to manage. They are worth observing, especially if they linger or get more harmful.
Extreme hypercapnia needs a more assertive approach. Efforts generally concentrate on a search for the underlying reason, and the search forms with a careful record and physical examination.
You will probably require a blood examination that calculates your CO2 level. An arterial blood gas (ABG) examination calculates your CO2, bicarbonate, blood oxygen, and pH.
Generally, blood examinations use blood specimens carried from a vein. An ABG examination needs a sample of blood from your artery.
You may also require further diagnostic examinations. In the meantime, you may need intervention with drugs and/or assistance with breathing from a breathing mask or mechanical ventilator.
Aside from blood examinations, specific go-to tests contain:
Imaging tests: A chest X-ray and chest computerized tomography (CT) scan can assist to estimate the severity of pulmonary diseases such as emphysema and pneumonia. If your healthcare provider believes the reason may be related to the brain, you may require a brain imaging examination, like magnetic resonance imaging (MRI).
Pulmonary function tests (PFTs): Several steps of your respiratory function can assist to evaluate your lung function. These contain your vital capacity (the highest quantity of air that can be inhaled or exhaled from the lung) and forced expiratory volume in 1 second (FEV1). This examination estimates how much air you can forcefully exhale in 1 second.
Pulse oximetry: Your oxygen level can read as normal actually when you have hypercapnia, but pulse oximetry is a noninvasive examination that can be used to monitor sudden modifications.
What treatment options are available?
If an underlying disease is causing your hypercapnia, your doctor will set up a treatment schedule for the symptoms of your disease. Your doctor will probably suggest that you quit smoking or restrict your disclosure to fumes or chemicals if they’ve generated COPD-related hypercapnia.
Medication
Some drugs can assist you to breathe better, involving:
bronchodilators, which assist your airway muscles work correctly
inhaled or oral corticosteroids, which assist maintain airway inflammation to a minimum
antibiotics for respiratory infections, like pneumonia or acute bronchitis
Ventilation
Ventilation is generally the first line of therapy for hypercapnia. A doctor may use:
Noninvasive ventilation: Airflow comes via a mouthpiece or nasal mask. This is useful for a patient with sleep apnea to maintain their airways open at night. It is also called continuous positive airway pressure, or CPAP.
Mechanical ventilation: A doctor will insert a tube via the mouth into the airway. This is known as intubation.
Patients with extreme hypercapnia symptoms may require a ventilation machine to assist them to breathe.
Intubation
Intubation needs that an endotracheal pipe to be put in your mouth and down into your airway. You are incapable to breathe or talk while you are intubated. You may require this kind of respiratory assistance temporarily while an extreme medical disease is being managed.
Surgery
Some patients may need surgery to manage or replace damaged airways or lungs. In a lung volume decrease surgery, your doctor or physician removes destroyed tissue to make room for your remaining healthy tissue to grow and obtain more oxygen. In a lung transplant, an unhealthy lung is extracted and substituted by a healthy lung from an organ donor.
Both surgeries can be difficult, so speak to your doctor regarding these choices to visit if they’re right for you.
Therapy
Pulmonary rehab is another therapy choice. It can differ significantly from one person to another but can contain a mix of physical exercises, breathing exercises, and diet and nutrition consultations.
Lifestyle changes
To decrease symptoms and avoid difficulties, a doctor may suggest:
- dietary changes
- raised physical activity
- quitting or avoiding smoking
- restricting exposure to dust, chemicals, and fumes, where possible
Prognosis
Hypercapnia has an irregular prognosis dependent on the same inducing etiology. In general, younger persons have a more suitable prognosis than more senior persons.
How to Prevent Hypercapnia?
Techniques for assisting to control hypercapnia contain:
- treating existing lung diseases
- quitting or avoiding smoking
- reaching or keeping a moderate weight
- following an exercise plan
- avoiding exposure to toxic fumes and chemicals
Complications of Hypercapnia
Extreme hypercapnia can generate noticeable and distressing results. Unlike mild hypercapnia, the body is unable of restoring CO2 balance, which can guide to acute symptoms:
- Acute paranoia, depression, or confusion
- Coma
- Dilation – widening of blood vessels in the skin
- Fainting
- Hyperventilation
- Panic attack
- Respiratory failure
- Seizure
- Swelling of the optic nerve (papilledema)
FAQ
What CO2 level is hypercapnia?
Hypercapnia is described as the PaCO2 being more significant than 42 mm Hg. If the PaCO2 is more significant than 45 mm Hg, and the PaO2 is shorter than 60 mm Hg, a person is told to be in hypercapnic respiratory failure.
What is a secure level of CO2 to breathe?
The American Conference of Governmental Industrial Hygienists (ACGIH) suggests an 8-hour TWA Threshold Limit Value (TLV) of 5,000 ppm and a Ceiling exposure limit (not to be exceeded) of 30,000 ppm for 10 minutes. A value of 40,000 is believed instantly hazardous to life and health (IDLH value).
How do you remove CO2 from your lungs?
Ventilator, a breathing device that blows air into your lungs. It also brings carbon dioxide out of your lungs. Further breathing therapies, like noninvasive positive pressure ventilation (NPPV), use mild air pressure to maintain your airways open while you sleep.
Is CO2 harmful to the lungs?
At low concentrations, gaseous carbon dioxide seems to have a little toxicological impact. At higher concentrations, it leads to a raised tachycardia, respiratory rate, cardiac arrhythmias, and damaged consciousness. Concentrations >10% may generate coma, convulsions, and death.
What machine removes CO2 from the lungs?
Carbon dioxide is extracted by a pump-driven modified ECMO device with venovenous bypass, while oxygenation is performed by elevated levels of positive end-expiratory force, with a respiratory rate of 3-5 breaths/min.





One Comment