Gluteus Medius Muscle
Introduction
- Gluteus medius is a large fan-shaped muscle located in the posterior hip, extending from the ilium to the proximal femur. Together with the gluteus maximus, gluteus minimus, and tensor fasciae latae muscles, it belongs to the muscles of the gluteal region.
- The gluteus medius muscle acts on the hip joint producing two movements; its anterior part internally rotates the thigh, while the contraction of the whole muscle abducts the thigh. Additionally, the gluteus medius muscle stabilizes the pelvis while standing or walking. This article will discuss the anatomy and function of the gluteus medius muscle.
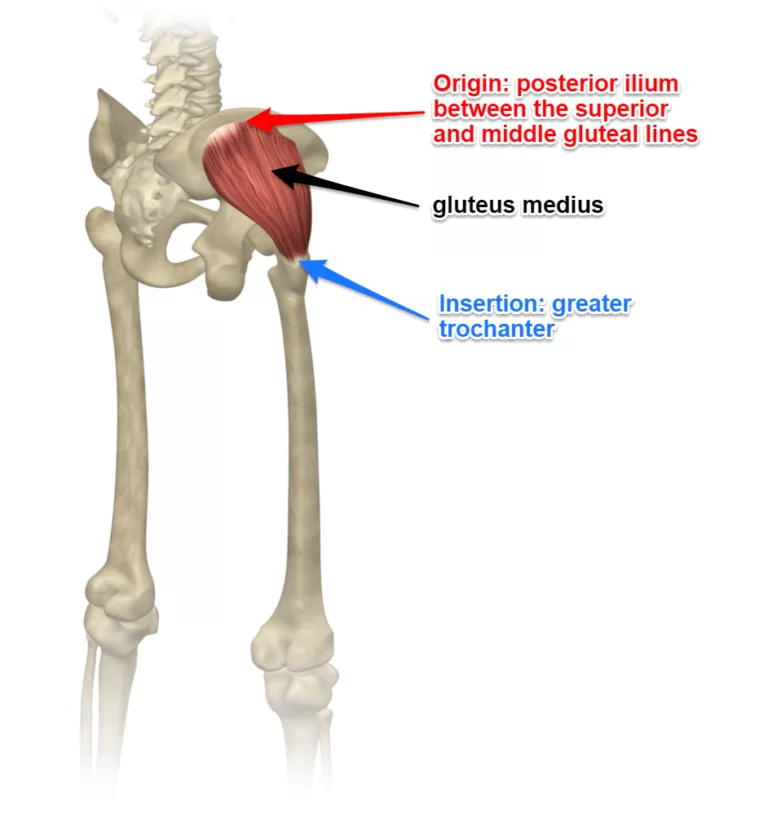
Origin
- Gluteal, or lateral surface of the ilium between the posterior and anterior gluteal lines and gluteal aponeurosis. This is a large area, reaching from the iliac crest above to almost the sciatic notch below.
Insertion
Glutes medius is divided into three portions similar to the deltoid muscle of the shoulder joint:
- Fibers of the posterior portion pass forward and downwards.
- Fibers of the middle portion pass downwards.
- Fibers of the anterior portion pass backward and downward. All Fibers combine to form a flattened tendon that attaches to the posterior and lateral part of the superior portion of the greater trochanter of the femur.
Nerve Supply
The gluteus medius is supplied by the superior gluteal nerve (root L4, L5, and S1). Cutaneous supply is mainly provided by L1 and 2.
Blood Supply
Deep branch of superior gluteal artery, trochanteric anastomosis.
The gluteus medius muscle is supplied by the superior gluteal artery. It is the internal iliac artery’s greatest branch. The artery passes between the lumbosacral trunk and the first sacral ramus in a posterior direction. It splits into deep and superficial branches after leaving the pelvis through the larger sciatic foramen located above the piriformis. The superior branch enters into the gluteus medius via 4–7 perforators, whereas the inferior branch inserts into the gluteus minimus via 0–2 perforators. The deep branch runs between the gluteus medius and the surface of the bone.
It anastomoses with the deep circumflex iliac artery and an ascending branch of the lateral circumflex femoral artery. The inferior branch nourishes the gluteus minimus via one to three perforators and the gluteus medius via three to eight perforators as it passes obliquely through both.
It joins the lateral circumflex femoral artery anastomosely. Because the superior gluteal artery leaves the pelvis at an acute angle, shearing forces can more easily cause damage to the structure. When displaced fractures occur, the artery may be compromised by the piriformis’s acute fascia. Surgery like acetabular fracture surgery puts the superior gluteal arteries and nerves in danger of damage.
Seldom does the internal pudendal artery give birth to the superior gluteal artery. On rare occasions, the inferior gluteal artery develops straight from the internal iliac artery. The branches of the internal iliac vessels, which receive the lymphatic drainage of the gluteal region, are surrounded by internal iliac nodes. The internal iliac nodes, which are located surrounding the common iliac artery, supply lymphatic drainage to the common iliac nodes. The lateral aortic nodes receive the outflow of the common iliac nodes.
Venous Drainage
There are two branches of the superior gluteal vein (SGV) that drain blood from the gluteal region: a superficial branch and a deep branch. The huge ischial foramen in the supra-pyriform canal allows the superior gluteal vein to enter the pelvis, where it meets the upper gluteal artery and terminates in the internal iliac vein. The inferior gluteal vein and the superior gluteal vein anastomose.
The buttock and posterosuperior area of the thigh are drained by the inferior gluteal vein (IGV). It starts from two branches that meet together to form a single trunk that travels parallel to the lower gluteal artery. The superior perforating vein and the medial circumflex veins of the femur, which are tributaries of the deep femoral vein, anastomose with the inferior gluteal vein.
Via the lower portion of the big ischial foramen, the inferior gluteal vein enters the pelvis and empties into the distal section of the internal iliac vein.
Function
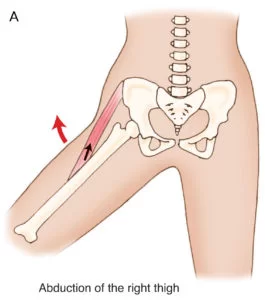
- Gluteus medius is the prime mover of abduction at the hip joint.
- Anterior portion of Gluteus medius abduct, assists in flexion and medial rotation of hip.
- Posterior portion of Gluteus medius abduct, assists in the ext. and lateral rotation of the hip.
- In hip flexion, all portions internally rotate the hip and it has been shown that at 90` of hip flexion the leverage of medial rotation of Gluteus medius is increased eight folds.
- All portions of Gluteus medius will produce hip abduction regrades the position o the hip.
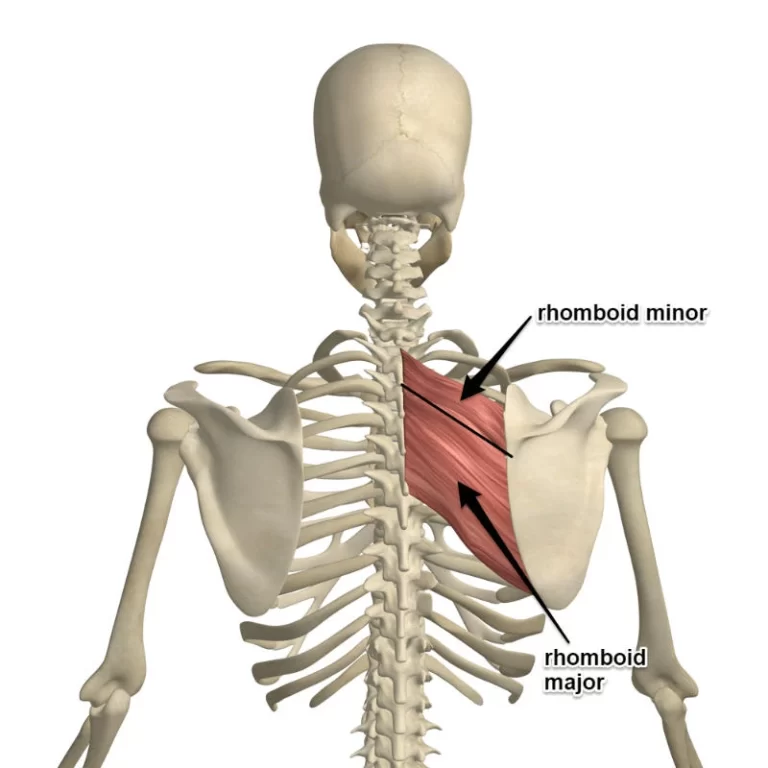
- Glutes medius is an extremely important muscle in maintaining frontal plane stability of the pelvis it forms with the ipsilateral tensor fascia latae and contralateral quadratus lumborum a lateral fascial sling whose main role is to provide frontal plane stability.
- Gluteus medius is an important muscle in walking, running and single-leg weight-bearing because it prevents the opposite side of the pelvis from dropping during walking, running and single leg weight-bearing. When a limb is taken off the ground the pelvis on the opposite side will tend to drop through loss of support from below. Gluteus medius works to maintain the side of the pelvis that drops therefore allowing the other limb to swing forward for the next step.
- Gluteus medius also supports the pelvis during gait by producing rotation of hip with assistance from gluteus minimus and tensor fascia lata. Conversely, the hip is supported during the stance phase by acting on the same side.

Palpation
Find the middle of iliac crest which is located above the greater trochanter. Two fingers below is the bulk of gluteus medius. The contraction of the muscle can be felt by alternate single leg-stands.
Embryology
The lower limb bud develops at around four weeks, or embryonic stage 14. By stage 17, the lower limb lacks a genuine knee and has a flattened footplate with a discernible hip joint. The digits split during stages 20 to 23, and by stage 23, which corresponds to the end of week eight, the toes are well defined.
Similar to other skeletal muscles, cells originating from somites located at the level of the lower limb bud create the gluteus medius. From the dermomyotome’s hypaxial edge, these cells demyelinate. After that, they move into the limb bud and multiply there. They finally differentiate into the gluteus medius muscle with the expression of myogenic determining factors.
Clinical Importance
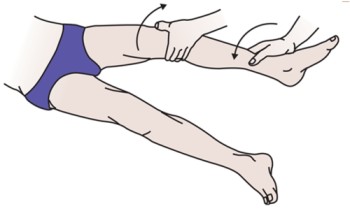
In a clinical environment, the gluteus medius and minimus can be examined jointly by internally rotating the thigh against resistance while lying supine with the hip and knee flexed. Nonetheless, an internal counter-resistance rotation test can be used to determine whether or not gluteus medius tears are present. Clinical tests for the gluteus medius and minimus, tensor fascia lata, and thigh abduction against resistance with the knee extended in a supine posture can be used.
The pelvis is supported by the combined action of the gluteus medius and minimus. The neck of the femur must be intact with its normal angulation to the shaft, the gluteus medius and minimus must be functioning normally, and the hip joint’s components must be normal for the gluteus medius and minimus to have their supporting effect on the pelvis when raising the contralateral foot. The Trendelenburg sign, which occurs when either of these diseases is present, is characterized by the pelvis sinking lower on the unsupported side while the patient stands on the affected limb.
Patients with paralysis of the gluteus medius and minimus will exhibit a distinctive lurching gait called Trendelenburg gait. Walking and running will not be significantly affected by the paralysis of other muscles functioning on the hip joint if these two muscles and their innervations remain intact. The cause of greater trochanteric pain syndrome (GTPS) might be either concurrent bursal disease or tendinopathy of the gluteus medius and/or minimus. Patients frequently report higher trochanter-localized lateral hip discomfort, which gets worse when they sleep on their sides or perform weight-bearing activities.
Clinically, the condition is identified by point soreness at the greater trochanteric region accompanied by lateral hip discomfort. Prolonged repetitive activities that involve the gluteus medius, such running, walking, standing on one leg, or ascending stairs, cause more pain. An intramuscular injection in the gluteal region may cause injury to the superior gluteal nerve. Injections should be made in the upper lateral quadrant to prevent damage to the sciatic and superior gluteal nerves, which are often located in the lower quadrants of the gluteal region.




14 Comments