Heel Pain and Physiotherapy Treatment
Heel pain is a common complaint that affects people of all ages and lifestyles. It refers to discomfort or pain experienced in the bottom or back of the heel. Heel pain can have various causes and may range from mild and intermittent to severe and chronic.
One of the most prevalent causes of heel pain is plantar fasciitis, which is the inflammation of the plantar fascia—a thick band of tissue that connects the heel bone to the toes. Plantar fasciitis often occurs due to repetitive strain or overuse, leading to small tears and inflammation in the fascia. This condition is particularly common among runners, athletes, and individuals who spend long hours on their feet.
Another common cause of heel pain is Achilles tendonitis, which involves inflammation of the Achilles tendon—a thick band of tissue that connects the calf muscles to the heel bone. This condition typically develops due to overuse, inadequate stretching, or a sudden increase in physical activity. Achilles tendonitis is commonly observed in athletes who engage in sports that require repetitive jumping or running motions.
Heel spurs are another potential cause that leads to heel pain. These are abnormal bony growths that develop on the underside of the heel bone. Heel spurs often result from long-term plantar fasciitis, where the inflammation causes calcium deposits to accumulate on the heel bone. While not everyone with plantar fasciitis develops heel spurs, their presence can contribute to persistent pain.
- there are many reasons behind heel pain but we are discussing only two plantar fasciitis and calcaneal spur.
Calcaneal spur
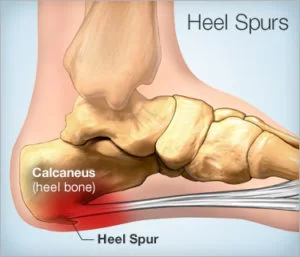
- A calcaneal spur, commonly known as a heel spur, occurs when a bony outgrowth forms on the heel bone. Calcaneal spurs can be located at the back of the heel (dorsal heel spur) or under the sole (plantar heel spur).
- The dorsal spurs are often associated with Achilles Tendinopathy, while spurs under the sole are associated with Plantar fasciitis.
- The apex of the spur lies either within the origin of the plantar fascia (on the medial tubercle of the calcaneus) or superior to it (in the origin of the flexor digitorum brevis muscle).
- The relationship between spur formation, the medial tubercle of the calcaneus, and intrinsic heel musculature results in a constant pulling effect on the plantar fascia resulting in an inflammatory response.
Anatomy related to Heel pain
- There are numerous muscles (Soleus, gastrocnemius, plantaris, abductor digiti minimi, flexor digitorum brevis, extensor digitorum brevis, abductor hallucis, extensor hallucis brevis, quadratus plantae) and the plantar fascia which exert a traction force on the tuberosity and adjacent regions of the calcaneus, especially when excessive or abnormal pronation occurs.
- The origin of the spurs appears to be caused by repetitive trauma which produces micro-tears in the plantar fascia near its attachment and the attempted repair leads to inflammation which is responsible for the production and the maintenance of the symptoms.
Symptoms of Heel pain
- The painful heel is a relatively common foot problem, but calcaneal spurs are not considered a primary cause of heel pain. A calcaneal spur is caused by long-term stress on the plantar fascia and foot muscles and may develop as a reaction to plantar fasciitis.
- The pain, mostly localized in the area of the medial process of the calcaneal tuberosity, is caused by pressure in the region of the plantar aponeurosis attachment to the calcaneal bone. The condition may exist without producing symptoms, or it may become very painful, even disabling.
- Most heel pain patients are middle-aged adults. Obesity may be considered a risk factor. Not all heel spurs cause symptoms and is often painless, but when they do cause symptoms people often experience more pain during weight-bearing activities, in the morning, or after a period of rest.
Causes of Heel pain
- Peroneal tendonitis
- Haglund’s deformity (with or without bursitis)
- Sever’s disease (calcaneal apophysitis): inflammation of the calcaneal apophysis due to overloading
- Traumatic Influences
- Calcaneal fractures (and stress fractures): fractures as a consequence of repetitive load to the heel
- Baxter nerve entrapment: (chronic compression of the first branch of the lateral plantar nerve)
- Tarsal tunnel syndrome (sinus tarsi): Impingement of the posterior tibial nerve
- Clinical (Tinel’s sign, dorsiflexion-eversion test)
- Heel fat pad syndrome: Atrophy or inflammation of the shock-absorbing fatty pad or corpus adiposum
- Chronic lateral ankle pain with other causes.
Diagnosis of Heel pain
- Diagnosis is based on the patient’s history and on the results of the physical examination. Diagnosis is usually confirmed by X-ray, but other diagnostic adjuncts are also used.
- Radiology may show calcaneal spur formation or calcification at either the insertion of the Achilles tendon or the origin of the plantar fascia. Rarely is an MRI required
Physiotherapy Treatment

- ULTRASOUND THERAPY: Ultrasound is a therapeutic modality that generates ultrasound causes deep heat, provides micro-massage to soft tissue, increases flexibility, promotes healing of tissue as well improves localized blood supply to the area. and ultimately pain relief.
- Cold therapy is used to relieve inflammation and reduce pain, Ice Massage- Ice on the area of inflammation for anti-inflammatory effects. Use ice in a paper or Styrofoam cup (peeled away) for 5-7 minutes, make sure to avoid frostbite.
- Heat therapy loosens tense muscles and promotes oxygen and blood flow to the affected area. Thermotherapy might be useful for the reduction of pain during exercises.
- Paraffin wax bath

- paraffin wax bath therapy is an application of molten wax on body parts.
- It acts as a form of heat therapy and can help increase blood flow, relax muscles, and decrease joint stiffness. Paraffin wax can also minimize muscle spasms and inflammation as well as treat sprains.
Low-level laser therapy
laser therapy is found to be an effective method for treating heel spurs.
- Night Splints
- A conservative treatment in combination with the use of a night splint that keeps the ankle in 5 degrees of dorsiflexion for eight weeks; Patients without previous treatments for plantar fasciitisobtain significant relief of heel pain in the short term with the use of a night splint incorporated into conservative methods; however, this application does not have a significant effect on prevention of recurrences after a two-year follow-up.
- Heel pads

Heel pads
Heel soft pads should relieve heel pain and inflammation and also help to absorb shock forces and distribute them evenly throughout the heel reducing stress.
However, We also recommend that Heel spur pads were effective in reducing foot pressure and reducing foot forces while customized can also be other options to reduce foot peak forces on both sides and are a better option compared to Heel pads.
Pre-fabricated and customized orthotics are therefore useful in distributing even pressure over the foot region through Footwear Modification
Footlogics: It helps in reducing relief from Plantar Fasciitis (heel pain and heel spurs), Achilles Tendinopathy, and also forefoot pain. The main goal is to correct overpronation, fallen arches, and flat feet.
Insoles study: If you are suffering from heel pain, diagnosed as Severe injury, wore insoles with no other treatments added and all patients maintained their high level of physical activity throughout the study. The study shows that significant pain relief during physical activity when using insoles was found.
Plantar Fasciitis
- Plantar fasciitis is a disorder that results in pain in the heel and bottom of the foot. Plantar fasciitis is the result of degenerative irritation of the plantar fascia origin at the medial calcaneal tuberosity of the heel as well as the surrounding perifascial structures.
- The pain is usually most severe with the first steps of the day or following a period of rest. Pain is also frequently brought on by bending the foot and toes up towards the shin and may be worsened by a tight Achilles tendon. The condition typically comes on slowly. In about a third of people, both legs are affected.
Function of Plantar Fasciitis
- The plantar fascia plays an important role in the normal biomechanics of the foot. The fascia itself is important in providing support for the arch and providing shock absorption.
Anatomy
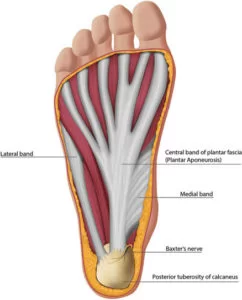
- Comprised of white longitudinally organized fibrous connective tissue that originates on the periosteum of the medial calcaneal tubercle, where it is thinner but extends into a thicker central portion.
- The thicker central portion of the plantar fascia then extends into five bands surrounding the flexor tendons as it passes all 5 metatarsal heads.
- Pain in the plantar fascia can be insertional and/or non-insertional and may involve the larger central band, but may also include the medial and lateral band of the plantar fascia.
Risk factors:
- Including overuse such as from long periods of standing, an increase in exercise, and obesity. It is also associated with inward rolling of the foot and a lifestyle that involves little exercise. While heel spurs are frequently found it is unclear if they have a role in causing the condition.
- Identified risk factors for plantar fasciitis include excessive running, standing on hard surfaces for prolonged periods of time, high arches of the feet, the presence of a leg length inequality, and flat feet.
- The tendency of flat feet to excessively roll inward during walking or running makes them more susceptible to plantar fasciitis. Obesity is seen in 70% of individuals who present with plantar fasciitis and is an independent risk factor.
- Achilles tendon tightness and inappropriate footwear have also been identified as significant risk factors.
- Loss of ankle dorsiflexion (talocrural joint, deep or superficial posterior compartment)
- Pes cavus OR pes planus deformities
- Excessive foot pronation dynamically
- Impact/weight-bearing activities such as prolonged standing, running, etc
- Improper shoe fit
- Elevated BMI > kg/m2
- Diabetes Mellitus (and/or other metabolic conditions)
Pathophysiology
- Originally, plantar fasciitis was believed to be an inflammatory condition of the plantar fascia. However, within the last decade, studies have observed microscopic anatomical changes indicating that plantar fasciitis is actually due to a noninflammatory structural breakdown of the plantar fascia rather than an inflammatory process.
- Due to this shift in thought about the underlying mechanisms in plantar fasciitis, many in the academic community have stated the condition should be renamed plantar fasciosis.
- The structural breakdown of the plantar fascia is believed to be the result of repetitive microtrauma (small tears). Microscopic examination of the plantar fascia often shows myxomatous degeneration, connective tissue calcium deposits, and disorganized collagen fibers.
- Disruptions in the plantar fascia’s normal mechanical movement during standing and walking (known as the Windlass mechanism) are thought to contribute to the development of plantar fasciitis by placing excess strain on the calcaneal tuberosity.
- Other studies have also suggested that plantar fasciitis is not actually due to inflamed plantar fascia, but may be a tendon injury involving the flexor digitorum brevis muscle located immediately deep in the plantar fascia.
Symptoms of Plantar Fasciitis
- Heel pain with first steps in the morning or after long periods of non-weight-bearing
- Tenderness to the anterior medial heel
- Limited dorsiflexion and tight Achilles tendon
- A limp may be present or may have a preference to toe walking
- Pain is usually worse when barefoot on hard surfaces and with stair climbing
- Many patients may have had a sudden increase in their activity level prior to the onset of symptoms.
Diagnosis
- Plantar fasciitis is diagnosed based on the history of the condition as well as the physical examination. Plantar fasciitis will have localized tenderness along the sole of the foot, most commonly at the inside arch of the heel.
- Usually, no further testing is necessary. X-ray testing can reveal an associated heel spur is present and rule out other causes of heel pain, such as fractures or tumors. Ultrasound imaging can also be helpful in diagnosing plantar fasciitis.
On palpation-
- Tenderness is present on the bottom of the heel, closer to the midline, and mild swelling and redness. There may be a presence of a nodule within the fascia.
Examination
- Take into consideration a patient’s medical history, physical activity, and foot pain symptoms.
- Active toe raise or passive dorsiflexion reproduces the symptoms
Look for the following:
- Pain reproduced by palpating the plantar medial calcaneal tubercle at the site of the plantar fascial insertion on the heel bone.
- Pain reproduced with passive dorsiflexion of the foot and toes.
- Windlass test – Passive dorsiflexion of the first metatarsophalangeal joint (test to provoke symptoms at the plantar fascia by creating maximal stretch), positive test if the pain is reproduced.
Secondary findings may include
- Tight Achilles heel cord, pes planus (see R), or pes cavus.
- An altered gait (look for biomechanical factors that may predispose the client to plantar fascia problems) or predisposing factors mentioned previously.
- Obesity
- Work-related weight-bearing
- Blends with the paratenon of the Achilles tendon, the intrinsic foot musculature, and skin and subcutaneous tissue.
- A thick viscoelastic multilobular fat pad is responsible for absorbing up to 110% of body weight during walking and 250% during running and deforms most during barefoot walking vs. shod walking.
- Windlass.
Medical Treatment of Plantar Fasciitis
Conservative measures are the first choice of Treatment:
Acute stage Treatment For Plantar Fasciitis
1)Relative rest– Discontinue running and walking for exercise until asymptomatic for 6 weeks. Switch to low-impact exercises like stationary bicycling, swimming, and deep water running with an alpha belt. Weight loss and modification of hard surfaces (cement) to soft surfaces (grass or cinder).
2)Anti-inflammatory– Oral anti-inflammatory has variable results. A brief trial of a cyclooxygenase (COX-2) inhibitor is tried. If the response is not dramatic, this therapy is discontinued because of the possible side effects.
3)Ice Massage– Ice on the area of inflammation for anti-inflammatory effects. Use ice in a paper or Styrofoam cup (peeled away) for 5-7 minutes, make sure to avoid frostbite
- Relative rest from offending activity as guided by the level of pain should be prescribed.
- Ice after activity as well as oral or topical NSAIDs can be used to help alleviate pain.
- Deep friction massage of the arch and insertion.
- Shoe inserts or orthotics and night splints may be prescribed in conjunction with the above.
- Educate patients on proper stretching and rehab of the: plantar fascia; Achilles’ tendon; gastrocnemius; and soleus.
- If the pain does not respond to conservative measures
- More advanced or invasive techniques may be tried eg extracorporeal shock-wave therapy, botulinum toxin A, autologous platelet-rich plasma, dex prolotherapy, or steroid injections.
- Important that advanced and invasive techniques be combined with conservative therapies.
- Surgery should be the last option if this process has become chronic and other less invasive therapies have failed.
Physiotherapy Treatment
Pain relieving modalities
- Ultrasound therapy: Ultrasound is a therapeutic modality that generates ultrasound and causes deep heat, which provides micro-massage to soft tissue, increases flexibility, promotes healing of tissue as well improves localized blood supply to the area. and ultimately pain relief
- Deep friction massage: Friction is a massage technique used to increase circulation and release areas that are tight; particularly around joints and where there are adhesions within the muscles or tendons. also has a soothing effect that provides pain relief.
- CONTRAST BATH: contrast bath work works on the principle of the combined effect of heat and cold the part alternatively immersed in the hot and cold temperature of hot water ranges from 36c-45c and cold water from 15c -20c.
- Treatment begins with hot water and should end with cold water. treatment time varies between 15 to 30 minutes, with immersion in hot water around 3 minutes and in cold water around 1 minute. it relieves the pain.
- TENS: transcutaneous electrical nerve stimulation is an electrical modality that provides pain relief by providing pain modulation.TENS closes the gate mechanism at the anterior grey horn in the spinal cord. also stimulates the endogenous opioid system which prevents the release of substance p at the anterior grey horn.

- reduce pain and inflammation by taking off the irritating focus of the strain of weight-bearing(heel-raised walking, walking while getting down from the bed in the morning or after long sitting)
- relieve strain from fascia by providing an appropriate wedge in the sole.
- faradism will be beneficial to induce contraction of the intrinsic muscle of the foot.
- hard shoes should be avoided.
- small heel shoes will help in transferring weight on toes.
- exercise of intrinsic muscle in warm water in the morning before initiating weight-bearing is useful in lessening pain.
- sustained toe-curling shoed be performed by the patient several times in the day.
- slow barefoot walking on the lateral border of the foot with cupping of the foot by curling of toes is effective in molding the longitudinal arch.
- Low-dye Taping- Some patients obtain relief with low-dye taping, but from a practical standpoint, daily taping is difficult to maintain.
- Shoe wear Modification (Running shoes)- Flared, stable heel to help control heel stability. Firm heel counters to control the hindfoot. Soft cushioning of the heel, raising the heel 12-15 mm higher than the sole. Well-molded Achilles pad. Avoid rigid leather dress shoes that increase torque on the Achilles tendon.
- Cushioned Heel Inserts in Treatment For Plantar Fasciitis- Viscoheels. Soft cushions are placed in and out of whatever shoe the patient is wearing.
- Patients with abnormal biomechanics of the lower extremity, such as pes cavus or pes planus, may benefit from the eventual use of custom cushioned orthotics.

- Plantar Fascia Stretching- Done 4-5 times a day, 5-10 repetitions. Done before first steps in the morning, before standing after a long period of rest. This gives good results as a Treatment For Plantar Fasciitis.
- Plantar fasciitis stretches
- Ultimately getting rid of plantar fasciitis long-term means stretching the plantar fascia so it does not put additional strain on the insertion to the heel. Below we outline a few simple exercises that should be done pain-free and in conjunction with other treatment options including massage.
Stretching the plantar fascia
- One way the plantar fascia can be stretched is by pulling up on the foot and toes with the hands. Hold the stretch for about 30 seconds. Repeat this stretch 5 times and aim to stretch 3 times a day
plantar fascia stretch by rolling

- The plantar fascia can be stretched by rolling the foot over a round object such as a ball, weights bar, rolling pin, or can of soup (or similar).
- Roll the foot repeatedly over the object, applying increasing downward pressure. Using an object that can be cooled in the freezer, such as a bottle or metal can, also applies cold therapy at the same time! This should be continued for 10 minutes per day until you can walk pain-free in the mornings.
- Runner’s stretches for the Achilles tendon- A tight Achilles tendon is often implicated as an exacerbating or a causative factor in plantar fasciitis. For this reason, much attention is given to Achilles tendon stretching exercises.
Gastrocnemius stretch
- Place the leg to be stretched behind and lean forward, ensuring the heel is kept in contact with the floor at all times. Hold the stretch for 20 to 30 seconds and repeat 3 times.
- This can be repeated several times a day and should not be painful. A stretch should be felt at the back of the lower leg. If not then move the back leg further back. A more advanced version of a calf stretch is to use a step and drop the heel down it.
Stretching on a step
- This stretch can be performed to further the stretch on the calf muscles and Achilles. Stand on a step with the toes on the step and the heels off the back. Carefully lower the heels down below the level of the step until you feel a stretch – make sure you have something to hold on to.
- Hold for 15-20 seconds. This should be performed with the knee straight and then repeated with the knee bent to make sure you are stretching both muscles. You should feel a gentle stretch. Be careful not to over-do this one.
Chronic Stage Treatment For Plantar Fasciitis-
- If the acute stage measures fail to relieve symptoms after several months, then before initiating chronic stage measures, reevaluate the patient for other causes of heel pain. Consider a bone scan if a calcaneal stress fracture is suspected. HLA-B27 and rheumatoid/seronegative spondyloarthropathy laboratory work-up if other systemic signs or symptoms are evident.
- the steps patients should take are part of Chronic stage Treatment For Plantar Fasciitis-
- Casting– In addition to acute stage measures casting has been shown to be helpful in about 50% of the patients. A short-leg walking cast can be used for 1 month with the foot placed in neutral. Evaluate success at 1 month, and consider an additional month of removable cast wear if necessary.
FAQ
What is the cause of heel pain?
The heel is a cushioned, fatty tissue-filled support that maintains its form under the force of movement and body weight. Obesity, poorly fitting shoes, running and leaping on hard surfaces, unusual walking gait patterns, traumas, and certain illnesses are among the common reasons of heel discomfort.
What is the best medicine for heel pain?
Plantar fasciitis Heel pain and inflammation can be reduced by over-the-counter painkillers such naproxen sodium (Aleve) and ibuprofen (Advil, Motrin IB, and others).
Will heel pain go away on its own?
With at-home treatment, heel pain frequently goes away on its own. Try the following if you have mild heel pain: Relax. Avoid activities that strain your heels, such as jogging, prolonged standing, and walking on hard surfaces, if at all possible.
Is heel pain due to uric acid?
Gout is a kind of arthritis marked by swelling, redness, trouble moving the feet, and an accumulation of uric acid. Walking usually involves the big toe. Nonetheless, certain forms of gout could be exclusive to the heel, making the distinction between it and plantar fasciitis challenging.
What are the 5 common causes of heel pain?
Common causes of heel pain are:
Achilles tendonitis
Achilles tendon rupture
Ankylosing spondylitis
Bone tumor
Bursitis
Haglund’s deformity
Heel spur
Osteomyelitis
Is walking good for heel pain?
Walking may relieve your heel pain or exacerbate it, depending on your unique situation. Try to relax as much as you can till the agony goes away if you have severe discomfort when walking.
Is hot water good for heel pain?
When treating foot pain, think about taking hot baths, but remember these points: Take cold and hot baths alternately. Some runners find that their problems worsen just because of the heat. If you are taking contrasting baths, immerse your heels in cold water to conclude the hot baths.





11 Comments