How to relieve sciatica in lower back? Physiotherapy Treatment, Exercise
What is Sciatica?
- Sciatica refers to pain that radiates along the path of the sciatic nerve, which branches from your lower back through your hips and buttocks and down each leg. Typically, sciatica affects only one side of your body.
- Sciatica most commonly occurs when a herniated disk, bone spur on the spine or narrowing of the spine (spinal stenosis) compresses part of the nerve. This causes inflammation, pain and often some numbness in the affected leg which radiates through your hips and buttocks and down to leg.
- Although the pain associated with sciatica can be severe, most cases can resolve with non-operative treatments in a few weeks.
- People who have severe sciatica that is associated with significant leg weakness and pain or bowel or bladder changes might be candidates for surgery.
What are the Causes of Sciatica?
- Sciatica occurs when the sciatic nerve becomes pinched, usually by an overgrowth of bone (bone spur) on your vertebrae or by a herniated disk in your spine. More rarely, the nerve can be damaged by a disease such as diabetes or compressed by a tumor.
- Spondylolisthesis is a slippage of one vertebra so that it is out of line with the one above it, narrowing the opening through which the nerve exits. The extended spinal bone can pinch the sciatic nerve and cause sciatica.
- Trauma injury to the sciatic nerve or lumbar spine.
- Tumors in the lumbar spinal canal that compress the sciatic nerve.
- Spondylolisthesis is a slippage of one vertebra so that it is out of line with the one above it, narrowing the opening through which the nerve exits. The extended spinal bone can pinch the sciatic nerve and cause sciatica.
- Cauda equina syndrome is a rare but serious condition that affects the bundle of nerves at the end of the spinal cord called the cauda equina. severe back pain can be a sign of cauda equina syndrome (CES), This syndrome causes pain down the leg, numbness around the anus and loss of bowel and bladder control.
What are the Risk factors for sciatica ?
- Age : Age-related changes in the spine like herniated disks and bone spurs, are the most common causes of sciatica.
- Obesity: By increasing the stress on your spine, excess body weight can contribute to the spinal changes that compresses the nerve and trigger sciatica.
- Prolonged sitting: People who have a sedentary life style or sit for a prolonged periods are more likely to develop sciatica than active people.
- Diabetes: This condition, which affects the way your body uses blood sugar, increases your risk of nerve damage so that it can cause sciatica.
- osteoarthritis: Osteoarthritis can cause damage to your spine and compress the nerve and put nerves at risk of injury.
- Have an injury/previous injury: An injury to your lower back or spine puts you at greater risk for sciatica.
- lack of core strength : Your “core” are the muscles of your back and abdomen. The stronger your core, the more support you’ll have for your lower back. Unlike your chest area, where your rib cage provides support, the only support for your lower back is your muscles.
Which are the symptoms of sciatica ?
- Usually, sciatica affects only one leg at a time and the symptoms radiate from the lower back or buttock to the thigh and down the leg. Sciatica may cause pain in the front, back, and/or sides of the thigh and leg.
- A few common symptoms seen in sciatica are:
- Pain:- Sciatica pain may be constant or intermittent. The pain is usually described as a burning sensation or a sharp, shooting pain.
- The pain is generally more severe in the leg compared to the back. Leg pain and burning sensation commonly occurs more in the calf below the knee joint compared to other parts of the leg.
- Altered sensation :- tingling , numbness and/or a pins-and-needles like sensation may be felt at the back of the leg.
- Weakness:- Weakness may be felt in the affected leg and foot. A feeling of heaviness in the affected leg may make it difficult to lift the foot off the ground.
- Change in posture may aggravate or relieve pain:-
- Certain postures may affect sciatica pain :
- Sciatica pain may get worse while sitting, trying to stand up, standing for a long time, bending the spine forward, twisting the spine, and/or while coughing.
- Pain may increase or remain constant while lying down, causing disturbed sleep. Lying on the back with the knees slightly elevated and propped up with the support of pillow, or lying on the side with a pillow between the legs, may help relieve the pain in such cases.
- The pain may be relieved while walking, applying a heat pack to the rear pelvic area, or doing pelvic exercises.
- There may be other sciatica symptoms that are specific to the affected nerve root. The sciatic nerve is formed by the combination of 5 nerve roots : L4, L5, S1, S2, and S3.
Sciatica Symptoms for Each Nerve Root :-
Sciatica symptoms usually occur when L4, L5, and/or S1 nerve roots are affected. Sciatica symptoms arising from each of these nerve roots are discussed below:
Sciatica from the L4 nerve root may cause :
- Pain, in the hip, thigh, and the inner (medial) areas of the knee and calf of the affected side.
- Loss of sensation over the inner calf.
- Weakness in the thigh muscles and the hip muscles that help pull the legs together.
- Loss of tendon reflex in the knee (reduced knee-jerk reflex).
Sciatica from the L5 nerve root may cause :
- Pain in the buttock and the outer part of the thigh and leg.
- Loss of sensation in the area of skin in between and over the great toe and the second toe.
- Weakness in the buttock and leg muscles.
- Difficulty in moving the ankle and in raising the great toe upward.
Sciatica from the S1 nerve root, also called classic sciatica, may cause :
- Pain in the buttock, back of the calf, and side of the foot.
- Loss of sensation in the lateral(outer) side of the foot, including the third, fourth, and fifth toes.
- Difficulty while raising the heel off the floor or walking on tiptoes.
- Weakness in the buttock and foot muscles.
- Loss of tendon reflex in the ankle (reduced ankle-jerk reflex).
- Sciatica pain mostly occurs when the nerve roots are irritated due to an inflammatory condition such as a herniated disc or pelvic muscle spasm. If a nerve is compressed, the symptoms are usually severe, resulting in marked weakness,pain and loss of function in the leg.
Which are the types of Sciatica ?
Depending on the duration of symptoms and if one or both legs are affected, sciatica can be of different types :
Acute sciatica :-
- Acute sciatica is a recent onset, 4 to 8-week duration of sciatic nerve pain. The pain may be self-managed and may not typically require medical treatment.
Chronic sciatica :-
- Chronic sciatica is persistent sciatic nerve pain that lasts for more than 8 weeks and usually does not subside with self-management. Depending on the cause, chronic sciatica may require surgical or nonsurgical treatment.
Alternating sciatica :-
- Alternating sciatica is sciatic nerve pain that affects both legs alternately. This type of sciatica is rare and may result from degenerative problems in the sacroiliac joint.
Bilateral sciatica :-
- Bilateral sciatica occurs in both legs together. This type of sciatica is rare and may occur due to degenerative changes in the vertebrae and/or the disc at several spinal levels, or from serious conditions such as cauda equina syndrome.
Wallet sciatica :-
- Informally, the term wallet sciatica may be used to describe sciatic pain that occurs while sitting on a wallet (or any object in the back pocket of a trouser).
How to diagnose sciatica ?
- A diagnosis of the underlying cause of sciatica is essential in formulating an effective treatment plan and managing sciatica pain. When sciatica is suspected, a doctor will take a medical history and conduct a physical examination to diagnose a sciatica. Medical imaging tests and diagnostic nerve blocks may be appropriate in some cases.
Physical Examination and Medical History :
- The goal of conducting a physical examination and review of medical history is to identify the pain pattern in the patient’s leg.
- Sciatica pain typically follows the areas of skin which is called the dermatome that are supplied by the sciatic nerve. The pain may also include other deeper tissues outside the classic dermatomal areas known as dynatomes. It is believed that pain from all the nerve roots that comprise the sciatic nerve usually have a dynatomal distribution, except S1 nerve pain, or classic sciatica, which typically involves a dermatomal pain pattern.
Physical examination :-
During a physical examination, the doctor may check for :
- Localized pain in the area of lower back, buttock, thigh, and leg
- The response to leg movements that elongate the nerve (straightening the leg)
- The response to certain stimuli, such as gently pressing the toes or calf region of leg
The doctor may also conduct certain clinical tests to check for sciatic nerve pain.
Clinical tests for sciatica :-
A few examples of clinical tests for sciatica are following :
1.Straight leg raise (SLR) test :-

- This test includes the patient lying on his/her back and lifting one leg at a time with the other leg flat or bent at the knee. A pain encountered while lifting the affected leg usually indicates sciatica.
2. Slump test :-

- This test includes the patient seated upright with hands behind the back. The patient bends (slumps) forward at the hip. The neck is bent down with the chin touching the chest and one knee is extended to a degree possible. If pain occurs in this position, sciatica may be present.
- These tests, however, may be positive only when the sciatic nerve is mechanically compressed at any point along its origin, such as from a herniated disc. Other causes of sciatica such as inflammation or chemical irritation of the nerve may not cause pain in these tests.
Medical history :
A medical history may include the doctor reviewing the following :
- The onset of pain and other symptoms
- Type, nature, and duration of pain
- Injury or trauma to the back or hip area
- The occurrence of muscle spasms or cramps in the pelvic region
- Decreased muscle strength in the leg
- If sciatica is suspected, some doctors may order medical imaging or diagnostic nerve block tests. These tests are used to confirm the cause of sciatica. Medical imaging or diagnostic injections also help plan surgeries or other invasive treatments.
Medical Imaging Tests for Sciatica :-
Medical imaging tests used in diagnosing the cause of sciatica include :
Magnetic resonance imaging (MRI) :- An MRI scan allows the doctor to visualize the sciatic nerve, surrounding soft tissues, and facet joint capsules. Tumors, facet joint inflammation, and herniated discs affecting nerve roots may also be seen on MRI scans.
Discogram:- A discogram test may be helpful in determining abnormalities in an inter vertebral disc. A contrast dye injected into the tissues may allow abnormalities in the disc, such as bulging or herniation to be seen on a medical imaging scan (such as computed tomography scan). A discogram may also be useful in identifying chemically induced sciatic nerve pain.
Diagnostic Nerve Block Injections for Sciatica :-
- Physical therapy incorporates a combination of streching, strengthening and aerobic conditioning and is a central component of almost any sciatica treatment plan. Therapeutic exercises may also be added to a physical therapy program.
- Selective nerve block injections are considered an accurate and effective method to diagnose sciatic nerve pain. An anesthetic solution is injected around the sciatic nerve root(s) to numb the pain transmitted by the nerve. The injection is performed under the guidance of fluoroscopy (live x-ray), ultrasound, or computed tomography (CT). These techniques allow the physician to help and guide the needle to the accurate location where the medication needs to be deposited.
- If pain relief is experienced, sciatica may be confirmed As with any injection technique, a small risk of bleeding, spinal cord tissue damage, and nerve damage may be possible with diagnostic nerve block injections.
- Once the cause of sciatica is diagnosed, a structured treatment approach for the specific condition is formulated. Both nonsurgical and surgical treatments are used to treat sciatica.
- It is advisable to treat sciatica as early as possible in order to avoid the progression of symptoms. Sciatica treatment may include both nonsurgical and surgical methods. Typically, nonsurgical methods are tried first. Surgery may be indicated when the underlying cause is severe and/or progressive neurological deficits such as leg weakness and severe pain occurs.
Nonsurgical Treatment for Sciatica :-
- First line treatments of sciatica typically include some combination of physiotherapy, therapeutic injections, medication and alternative therapies.
- Acute sciatica usually gets better with 4 to 6 weeks of nonsurgical treatment. For chronic sciatica with pain lasting over 7 to 8 weeks, treatment time may take longer and may depend on the underlying cause.
Medication for Sciatica Pain:
- Both prescription and over-the-counter (OTC) medications may be used to relieve sciatica pain.A few examples of medications used to treat sciatica pain are following :
- Non steroidal anti-inflammatory drugs (NSAIDS), such as ibuprofen or naproxen
- Oral steroids, such as prednisone
- Anticonvulsant medications, such as gabapentin
- Tricyclic antidepressants, such as amitriptyline
- Opioid analgesics, such as tramadol or oxycodone
- These drugs are ideally taken in order to obtain pain relief and allow the patient to participate in physical therapy. Drugs such as opioid analgesics are commonally prescribed for short durations to avoid addiction.
Chiropractic Therapy :
- Manual manipulation, usually performed by a chiropractor, aims at improving the alignment of the spine. This technique may help address the underlying conditions that can cause sciatic nerve pain and its symptoms, such as herniated discs or spinal stenosis. Manual manipulation can also create a better healing environment and should not be painful.
Massage Therapy :
- Certain forms of massage therapy, such as deep tissue massage, may have benefits for pain relief.
- The benefits of massage therapy are following :
- Improving blood circulation, which in turn creates a better healing response in the body
- Relaxing tight muscles, which may be contributing to the pain
- Releasing endorphins, which are hormones in the body that function as natural pain relievers
Physiotherapy treatment for Sciatica :
- Physiotherapy incorporates a combination of strengthening, stretching, and aerobic conditioning and is a central component of almost any sciatica treatment plan. Therapeutic exercises may also be added to a physiotherapy program.
- Sciatica treatment usually starts with nonsurgical methods and includes some combination of physiotherapy, medications, therapeutic injections, and alternative therapies.
The goals of physiotherapy and exercises for sciatica are following :
- Strengthen the spine and muscles of the lower back, abdomen, buttocks, and hip.
- Increase core muscles strength
- Stretch inflexible and tight muscles, such as hamstring muscle
- Encourage the exchange of fluids and nutrients in the body by light aerobic exercises such as walking, swimming, or pool therapy.
- While some rest or activity modification may be necessary, it is important to maintain as much activity as possible and avoid prolonged periods of physical in-activeness or bed rest.
- Certain exercises to treat sciatica may be specific to the underlying cause. Trained health professionals, such as psychiatrists, physiotherapists, chiropractors or qualified certified athletic trainers can help formulate an effective treatment plan to relieve sciatica pain through exercise and physical therapy.
Treatment of sciatica pain and sciatica exercises :
- Treatment for sciatica pain will almost always involve a controlled, progressive exercise program. The exercise treatment helps address, resolve, and prevent recurrences of the underlying cause of pain.
- Targeted sciatica exercises serve the following main purposes :
- Reduce the acute sciatic nerve pain
- Improve leg mobility and range of motion
- Promote soft tissue healing
- Improve sciatic nerve function
- Provide muscle and soft tissue conditioning
- Prevent, or at least minimize, recurrence of pain
- To be effective, therapeutic exercises must be done regularly and as prescribed, using the specific form and program. Close attention to exercise posture and body mechanics is a challenge but is essential for the exercises to be effective.
- This article provides a comprehensive guide to relieving sciatica pain through therapeutic exercise for the common diagnoses of sciatic nerve pain.
Exercise Provides Sciatica Pain Relief :
- While it may seem counterintuitive, exercise is more effective in relieving sciatica pain than bed rest or staying active with daily physical activities. Prescribed exercise is different from physical activity because it is planned, structured, repetitive, and a progressive process validated in improving overall fitness.
- While a short period of rest and limited movement or exercise may be necessary when the sciatica pain flares up, long periods of inactivity usually make the pain worse. With prescribed exercise, sciatica pain is relieved due to the following tissue changes:
Increased muscle strength :-
- Exercise increases the activation (proper engagement of the muscle) and area of the deep muscle fibers, improving muscle strength. Strong muscles help support the spine, improving its stability. Pain from muscle fatigue is also reduced.
Improved bone health :-
- Exercise increases bone density, resulting in stronger bones. The quality of bone in conditions such as osteoporosis and bone pain from arthritis and ankylosing spondylitis have shown to improve with exercise.
Enhanced blood flow :-
- Blood flow to the muscles, nerves, and other soft tissues in the spine is increased with exercise. This process results in a better supply of nutrients to these tissues, promoting healing and relieving stiffness.
Nourished spinal discs :-
- The spinal discs between the spinal vertebrae exchange fluids to receive nutrition and stay healthy. A healthy disc swells with nutrients and water and squeezes it out, similar to the action of a sponge. This action improves when forces are applied to the disc during exercise, distributing nutrients throughout the disc.
Reduced stiffness of the sciatic nerve :-
- Stiffness of the sciatic nerve can be improved through nerve glide (nerve stretching) or mobilization exercises. These exercises help maintain the flow of nutrients between the nerve and surrounding tissues, increasing its flexibility. This process also reduces nerve swelling and reverses negative immune system changes.
Without exercise and movement, the back muscles and spinal structures become weak and stiff or deconditioned and less able to support the back. The deconditioning can lead to further trauma and strain, which can cause additional pain.
Most customized exercise programs include a set of common principle as described below :
Building core muscle strength :-
- Many sciatica exercises serve to strengthen the core muscle group the back, abdominal muscles and pelvic muscles provide more support for the back. When patients engage in a regular program of gentle core strengthening exercises, they can recover more quickly from a worsening symptoms of sciatica and are less likely to experience future episodes of pain.
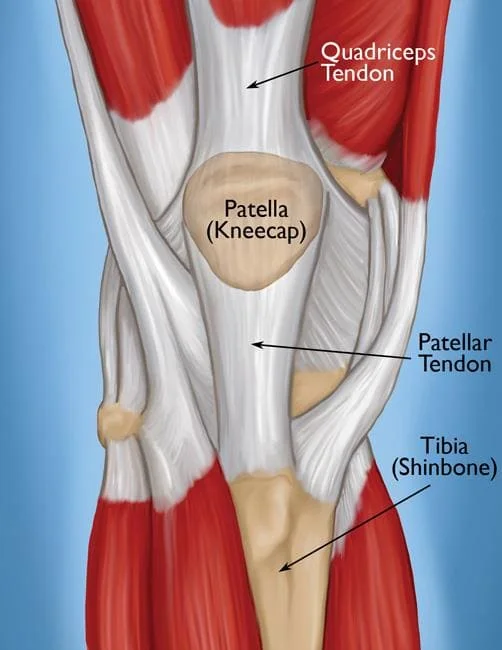
Improving hamstring flexibility :-
- Most types of sciatica will benefit from a regular routine of hamstring stretching. The hamstrings are muscles located in the back of the thigh. Overly tight hamstrings increase stress on the lower back and often aggravate or even cause some of the conditions that result in sciatica.
Practicing aerobic exercises :-
- Aerobic conditioning is recommended for general fitness, blood flow, and the release of pain-fighting hormones called endorphins. A simple exercise is walking, which can provide all the benefits of an aerobic workout. Walking can be performed at a pace that is comfortable and tolerable. As strength builds up, it is best to gradually progress to doing up to 3 miles of exercise walking at a brisk pace each day.
Support the Spine Throughout the Day to Minimize Sciatica Pain:-
Activity modification and ergonomics in daily activities are almost always required to avoid further aggravating the sciatic nerve. General recommendations include:
- Using appropriate ergonomics while lifting any object by bending the knees and leading with the hips
- Maintaining supported posture while sitting, standing and walking
- Avoiding long time of standing or sitting to prevent muscle fatigue
- Keeping one foot propped up on a step stool while standing for a long time
- Avoiding twisting and bending movements of the spine during morning hours to protect the discs
- Using heat therapy before exercise or physical activities or after waking up in the morning to loosen up the soft tissues and improve spinal flexibility
- Warming up for 10 to 15 minutes with light aerobic exercise before engaging in vigorous workouts
- Using an ice pack to reduce muscle soreness after physical activity and exercise
- Placing pillows between the two legs while sleeping on the side (side lying position) or under the knees while sleeping on the back (supine position)
Before beginning any exercise program, it is recommended to consult a trained healthcare professional to get a correct diagnosis for sciatic nerve pain. An accurate diagnosis of condition also helps to rule out serious problems, such as infections, tumors or cauda equina syndrome. Self treatment for sciatica is not a good idea and it may cause further irritation of the sciatic nerve if done incorrectly. Exercises must be learned from a trained professional physiotherapist and performed as a part of a guided program.
Strengthening the Lower Back Muscles :
Lower back strengthening and stabilizing exercises include more advanced workouts while lying on the stomach. These exercises increase muscle strength, maintain posture, and prevent excessive movements of the lumbar spine.

1. Upper Back extension:-
- This exercise strengthens the extensor muscles of the spine. In the prone position, with both hands clasped behind the lower back, gently raise the head and chest slightly while looking at the floor (stay low).
- Begin by holding the position for 5 seconds and gradually work up to 20 seconds. Aim to complete 8 to 10 repetitions.

2. Prone arm and leg lifts:
- This exercise strengthens the back, abdominal, trunk, and hip muscles. In the prone position with the head and chest lowered to the floor, slowly raise an arm and the opposite leg, 2 to 3 inches from the floor, without bending the knee.
- Begin by holding the position for 5 seconds. Complete 8 to 10 repetitions. As strength builds, aim to hold the position for 20 seconds.
Strengthening the Abdominal Muscles :
Exercises that build abdominal muscle strength and stability are performed while lying on the back (supine position).

1.Curl-ups for upper abdominal muscles:
- Start by lying on the back with both knees bent and feet flat on the floor. place both hand behind the neck and tilt the pelvis to flatten the back against the floor.
- Gently lift the head and shoulders off the floor.
- Hold for 2 to 4 seconds and slowly get back to the starting position.
As strength builds, aim to complete 2 sets of 10 curls. Do not attempt to lift the head up too high. If neck pain occurs, place the hands behind the head to support the neck.
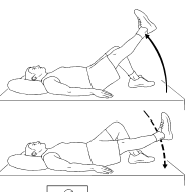
2.Single leg raises for the lower abdominal muscles:
- Start by lying on the back and tightening the stomach muscles.
- Slowly raise one leg 8 to 12 inches from the floor, without bending the knee. Keep the low back and opposite leg flat against the floor. Hold leg raise for 8 to 10 seconds, then slowly lower to starting position.
- As strength builds, aim to complete 2 sets of 10 lifts.
- If performing these exercises is painful, water therapy may be considered as an alternate option. The buoyancy water provides support, which in turn minimizes the pain. Water exercises can be particularly beneficial in strengthening the lower abdominal and hip muscles.
Ergonomics for sciatica :-
1. Take a Seat
- Sitting for long periods of time isn’t good for your spine or your sciatica pain. If possible, stand up every 15 to 20 minutes and walk a couple of laps around your workspace.
- Make sitting more comfortable by choosing a well-designed ergonomic chair. You can also add lower back support by placing a lumbar pillow or even a rolled-up towel at the base of your chair.
Simple tips to reduce sciatica pain in sitting :
- Don’t cross your legs in sitting position
- Position feet flat on the floor or resting on stool
- Keep hips and knees bent at a 45-degree angle
- If your chair has wheels, use them. Instead of twisting and turning your body, use the chair to move your body as a single unit.
2. take a stand
- Varying your posture is a smart way to care for your spine on the job, so mix it up when it comes to sitting and standing.
- Sitting all day has been connected to an array of health problems beyond back pain, including obesity and type 2 diabetes.
the potential benefits of incorporating standing into your work routine are numerous. To name a few:
- Standing lowers your type 2 diabetes risk: sitting for a long period during their day had higher levels of fasting blood sugar.
- Standing reduces your cardiovascular risk: people who spend at least two hours a day sitting boost their risk for cardiovascular-related health problems by 125%.
- Standing helps you burn some extra calories: regular use of sit-stand desks at work may help to burn extra calories and prevent weight gain when combined with other low-intensity activities.
one of the easiest ways to transition from a sitting to standing work posture is using a sit-stand desk (or sit-to-stand desk). A sit-stand desk allows you to adjust your desk height so you can work seamlessly from sitting to standing.
While standing at work is important, avoid standing in one place for a long time. If your job requires standing, try resting one foot on a small sturdy box or stool. Alternate every 10 to 15 minutes.
A note for standing with sciatica:
- Take special care when you go from sitting to standing when you have sciatica. Don’t bend at the waist to get up from your chair. Bending at the waist can stretch and aggravate an already irritable sciatic nerve. Instead, slide to the front of your seat and stand up by straightening your legs.
3. Stay Close to Work
- Keep your work close to your body to avoid forward bending. Again, forward bending can aggravate your sciatic nerve. Keep your shoulders relaxed, and rest your elbows and arms on the desk.
4. Tech Tips for Computer Users
Creating a sciatica-friendly computer workstation is easy. Consider these three tips:
- Position the monitor in front of you at eye level.
- Keep the keyboard and mouse close to you so that you can avoid reaching.
- Choose a chair that provides good back support.
By incorporating each point, you can avoid leaning (or slumping) forward.
5. Muscle Smarts with Sciatica
- Avoid or limit movements or activity that require muscular force, such as pushing a sofa or picking up a table or weight. Carrying a bag, briefcase, groceries, or luggage can present a challenge. A good tip is to carry an equal amount of weight in each hand. This might be a good time to rid your bag or briefcase of unnecessary items.
6. At the End of the Day, Your Mattress Matters
- After a long day, you want to get off your feet and rest. However, what you rest your back on can affect how good or bad you feel the next day. If your mattress is soft and lumpy, your spine will not be properly supported, leading to muscle fatigue and a poor night’s sleep.
How to sit with sciatica ?
| Do’s | Don’t |
| Keep hips at 45 degree angle | Don’t Cross your legs while seated |
| Keep knees at 45 degree angle | Don’t Twist or turn your body while seated in the chair |
| Keep feet flat on floor (or footrest) | |
| Ensure your bottom is at the back of the seat pan when seated | |
| Use an ergonomic chair : – with castor wheels to move your body around the space – lumbar support with the pillow or towel to support the spine – High back to support your whole back |