Knee Arthrocentesis
Introduction
The procedure of collecting synovial fluid from a Knee joint cavity is called Knee arthrocentesis. It can be used for treatment as well as for diagnosis.
Although arthrocentesis is regarded as a minor surgical procedure, blood vessels, nerves, and tendons can still be injured around the procedure.
Thus, the process should only be carried out by healthcare providers who know joint anatomy. The joint’s extensor surface should be in extension with little flexion for a decreased chance of injury.
Anatomy and Physiology
Anatomical considerations involve:
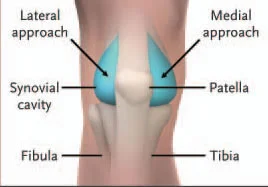
- Medially, laterally, superiorly, or inferiorly to the patella, surgeons can access the knee.
- The quadriceps muscle should be relaxed and raised to a 20-degree flexion position when the patient extends their knee.
- When the doctor inserts the needle, they should press the patella with their thumb.
- They should set it 1 cm lateral and 1 cm superior during the suprapatellar approach.
- Following establishing the patella’s midpoint, they should insert a needle 1 cm medially or laterally.
For this procedure to facilitate aspiration, they should aim the needle posterior to the patella and up toward the joint space. Then, they should squeeze or “milk” both sides of the joint space.
Relevant Anatomy for Knee Arthrocentesis
The needle enters 1 to 2 cm medial to the superior half or third of the patella when using the anteromedial approach. From the lateral side of the knee, the same technique can be performed.
Arthrocentesis of the knee

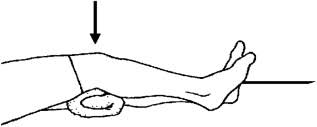
When the patient is in a supine position with their knee extended, the knee and the associated suprapatellar pouch can be punctured. Anteromedially, under the cephalad half or third of the patella, is where an 18- or 20-gauge needle can be inserted. An alternative position for the needle is laterally, directly below the patella’s cephalad edge (illustrated in drawing).
Equipment for Knee Arthrocentesis
- Sterile gauze, gloves, and an antiseptic solution (that includes chlorhexidine, povidone iodine, or isopropyl alcohol) are required.
- Nonsterile underpads.
- 1% lidocaine, a 25–30 gauge needle, and a 3- to 5-mL syringe are a few examples of local anesthesia.
- A 20- to 60-mL syringe and an 18- or 20-gauge needle measuring 51 mm (2 inches) are required for joint aspiration.
- Multiple syringes and either a hemostat or a three-way stopcock may be needed to treat large effusions.
- Correct containers to collect fluid for tests in the lab (such as cultures, crystals, and cell counts).
- A syringe with a corticosteroid (triamcinolone acetonide, 20–40 mg, or methylprednisolone acetate, 40–80 mg)and/or a long-acting anesthetic (0.25% bupivacaine, 20–40 mg), a 23–25 gauge needle, and a hemostat to assist with syringe changing if needed, are necessary for intra-articular therapeutic injection.
Preparation
Assistance and procedural sedation may be required for nervous patients who are in pain or who are unable to cooperate during the procedure. Providing some kind of local anesthesia is strongly suggested.
For most surgeons, 1% lidocaine will be necessary to produce skin numbness. Deep injections of local anesthetic should be avoided as there is the possibility that this could change the results of the synovial fluid analysis.
Positioning for Knee Arthrocentesis
The patient should be positioned supine on the stretcher, with a towel roll under the knee, and either fully extended or flexed 15 or 20 degrees. Position the foot so that it is parallel to the ground.
Step-by-Step Description of Knee Arthrocentesis
- To determine the patella, palpate the knee. When cleaning the skin, make an indentation or, if selected, apply a skin-marking pen to show the location of the needle insertion.
- Applying an underpad, support to the knee. Use an alcohol wipe to remove any skin-cleansing agent that might have been applied to the area and the site, such as povidone iodine or chlorhexidine.
- Using a 25-gauge needle, use a wheal of local anesthetic over the needle entry site. Following that, inject further anesthetic into the deeper tissues in the path that the arthrocentesis needle is expected to travel; do not, however, enter the joint space.
- Using an 18- or 20-gauge needle on a 20- to 60-mL syringe, aspirate the joint. A three-way stopcock should be inserted between the syringe and the needle when making use of one.
- Insert the needle perpendicularly into the skin, then point it posteriorly, behind the patella, in the path of the intercondylar notch. Try to maintain the needle trajectory horizontal to avoid making contact with articular cartilage. In addition, you can hold the patella and slowly pull it upward.
- The needle increases as you slowly pull back on the plunger. Once the capsule is opened, synovial fluid will flow into the syringe. Retraction almost to the skin’s surface and subsequent redirection at an alternate angle is required if the needle contacts a bone.
- When aspiration proves ineffective, consider attempting the process from the other side of the knee or advancing from a slightly flexed to a fully prolonged posture.
- Take in as much liquid as you can. Use light pressure on the suprapatellar area to aid in the drainage of excess fluid.
- A second syringe may be required for large effusions. Using the three-way stopcock or a hemostat to hold the needle properly in place during syringe exchanges are two methods used to leave the needle in place.
- If taking intra-articular medications (such as anesthetics or corticosteroids), remove the syringe that contained synovial fluid and replace it with the syringe that contained the medication while making the needle’s hub motionless (using a hemostat if one is available). No resistance will arise after the injection of medication if the needle has remained in the joint space.
- To be certain that the corticosteroid is distributed throughout the joint, move the joint through its full range of motion after injecting it.
- Before testing synovial fluid, transfer it to tubes and other transport media. Take the liquid for fat and blood.
- When aspiration is complete, remove the needle and cover the wound with a sterile dressing or an adhesive bandage.
Aftercare for Knee Arthrocentesis
- Oral nonsteroidal anti-inflammatory drugs (NSAIDs), elevation, and ice packs may all aid in reducing pain.
- To decrease pain and swelling during surgery for large effusions, cover the area with an elastic bandage.
- It is suggested to prescribe limited joint activity for 4 to 8 hours after the injection of an intra-articular anesthetic.
- Knee and ankle injuries are particularly common after anesthesia. These are weight-bearing joints.
- The joint should be rested around 24 to 48 hours following the injection of an intra-articular corticosteroid.
- A possible infection in the joint should be examined if the patient experiences increased erythema, pain, or swelling more than 12 hours following the procedure.
Warnings and Common Errors for Knee Arthrocentesis
- Check you are positioned optimally before puncturing the joint.
- Give the local anesthesia sufficient time to work before continuing.
- Avoid pushing the needle against resistance or moving it once the synovial fluid has started to drain to protect the synovium and articular cartilage.
- When the needle tip needs to be moved, pull it almost to the skin’s surface before redirecting it. Never attempt to alter the insertion angle while the needle is embedded in tissue.
- Determine between an effusion in the knee and swelling of the prepatellar bursa.
Equipment Required
General arthrocentesis equipment
- Betadine or Chlorhexadine.
- Sterile gloves/drape.
- Sterile gauze.
- Lidocaine.
Syringes
- A little syringe (6–12 cc) is used to inject local anesthetic.
- Large aspiration syringe (one 60 cc or two 30 cc).
Needles
- 18 gauge: knee.
- 20 gauge: most other joints.
- 25 gauge: MTP joints.
- 27 gauge for anesthetic injection.
Purple collection tubes for crystal analysis and red tops).
Culture bottles.
Consider utilizing U/S to assess for effusion.
Procedure
General Setup
- Using a circular motion away from the joint, prep the area three times with betadine or chlorhexidine.
- Drape joint in a sterile fashion.
- Place lidocaine topically with a 25–30 ga needle, and then subtly into deeper tissues.
- Pull back on the syringe as you insert the 18 ga needle (for larger joints) into the joint space.
- Once you start taking liquid, stop; try to aspirate as much as you can.
- Send Gram Stain, crystal analysis, cell count, or culture.
Specific Approach
- Can be placed either superior or inferior to the patella, medially or laterally.
- Extend the knee fully and make sure your quadriceps are relaxed (you may also optionally add a bump with 20 degrees of flexion).
- Place your thumb on the patella and slide it over as the needle is inserted.
- For the Suprapatellar Approach, get 1 cm to the side and 1 cm up.
- Determine the patella’s midpoint and place a needle 1 cm medially or lateral.
- Direct needle posterior to the patella and horizontally toward the joint space.
- Placing force or “milking” to the joint space on both sides may make aspiration easier.
Tips and Tricks for Knee Arthrocentesis
If there’s no apparent large effusion, think about undergoing ultrasonography.
A suction-applied pressure to the popliteal space and then the suprapatellar pouch can occasionally result in the aspiration of additional fluid.
In addition take note of the possibility that an acutely inflamed arthritic joint may be covered in warmth, tenderness, and erythema, which might suggest an extramuscular infection.
Infectious arthritis is more likely when the following factors are taken into consideration when attempting to distinguish it from infection of the surrounding structures, which is recommended for arthrocentesis:
- Knee Joint effusion.
- Joint pain around the edges and soreness in the capsule.
- Both mild, passive motion and rapid joint motion may cause pain.
Consider the following when analyzing fluid:
- A traumatic tap usually causes nonuniform bleeding and clotting during the hemarthrosis.
- One reason for fat within a hemarthrosis (lipo hemarthrosis) is an occult fracture.
Indications of Knee Arthrocentesis
General arthrocentesis indications
- Suspicion of septic arthritis.
- Suspicion of crystal-induced arthritis.
- Evaluation of therapeutic response for septic arthritis.
- Unexplained arthritis with synovial effusion.
- Joint capsule integrity is determined if there is an overlying laceration.
- Therapeutic: (injection of steroids or anesthetics, decrease intra-articular pressure).
Therapeutic: Taking large, painful joint effusions can help reduce pain. In addition, it can be used to inject some medications—mostly steroids—intraarticularly. Evaluate the way the treatment is working.
Diagnostic: Doctors may differentiate between septic arthritis and an inflammatory cause of bloody monoarthritis with precision by using synovial fluid analysis, which can also provide an apparent etiology of acute arthritis.
The clinic or the small operating room can be used to perform the procedure.
Contraindications to Knee Arthrocentesis
General arthrocentesis contraindications
Absolute contraindications
- infection of the skin or deeper tissues where the needle is expected to be placed.
- Use an alternate, unaffected puncture site if at all possible. Acutely inflamed joints, however, can often be warm, tender, and erythematous; this can mimic extra-articular infection and complicate the determination of an uninvolved insertion site.
- The decision to execute arthrocentesis despite the surrounding erythema may be supported by the visualization of a joint effusion by ultrasonography.
- No absolute contraindications for diagnostic arthrocentesis.
- A joint that you suspect may already be infected should not receive a steroid injection.
- NOTE: Joint infection must not be overlooked, thus arthrocentesis should be given if infectious arthritis is highly suspected, regardless of erythema or negative ultrasonographic results.
Relative contraindications
- Severe bleeding diathesis, which should be treated before arthrocentesis; regular therapeutic anticoagulation is safe to use, particularly in situations in which infection is suspected.
- prosthetic joint arthrocentesis, which is prone to iatrogenic infection, should typically be performed by an orthopedic surgeon.
- Overlying cellulitis.
- Coagulopathy.
- Joint prosthesis.
Complications
- Damage to surrounding structures, discomfort, infection, and re-accumulation of effusion are symptoms of local trauma.
- A dry tap can happen from improper needle placement or thickened synovium.
- If a big needle punctures a blood vessel during several attempts, hematuria could occur. The hemarthrosis usually appears a few hours after the procedure. The condition is frequently related to joint pain, stiffness, and swelling. The majority of cases of hemarthrosis are self-limited and go away in just a few weeks. A hematologist’s advice may be helpful if the patient has a coagulopathy that requires to be treated.
- The patient is required to start taking antibiotics right away if arthrocentesis—searching for a septic joint—is done through an infected skin area. Admission is suggested if the fluid is completely purulent.
- Infection.
- Traumatic tap damage to a tendon, nerve, or blood vessel.
- Pain.
- Re-accumulation of effusion.
- Damage to tendons, nerves, or blood vessels.
Transcript
This protocol describes arthrocentesis, a procedure that includes taking synovial fluid from the knee joint after a needle is inserted. A therapeutic or diagnostic arthrocentesis is necessary. To test and determine the type of effusion, synovial fluid may be recovered.
Pain in the knee can be decreased by draining fluid from it. When the patient is in a supine position, locate the patella by gently palpating the knee, and mark the patella’s four corners with a skin marker. Using a skin marker, draw an X at the location of one finger’s breath superolateral to the patella, being cautious to avoid visible veins and infected skin.
Consider a medial approach immediately posterior to the patella if an examination reveals an extensive effusion and the patella appears to be sitting on fluid. Consider three two-by-two-inch gauze sponges and soak them in iodine to clean the chosen needle entry site. Allow antiseptic to air dry.
Gently press the fluid laterally with the nondominant hand over the area superomedial to the patella. Making use of a syringe-attached 1.5-inch, 18–22 gauge needle, insert it along the anesthetized pathway. Whenever synovial fluid is apparent, slowly advance the needle and gently retract the plunger.
If you need to aspirate more fluid after the first syringe fills up, use a different one. Following that, cover the site with a sterile dressing and apply pressure until any bleeding stops. Remove the needle and syringe in one fluid motion. After through an alcohol pad to take off the iodine and skin marker, apply a bandage once hemostasis has been achieved.
When treating rheumatoid arthritis patients with intraarticular corticosteroids, aspirating as much synovial fluid as possible may reduce the risk for a recurrence of arthritic symptoms, according to a comparative study comparing complete aspiration of knee synovial fluid and intraarticular injection with corticosteroid alone.
There is no statistically significant difference in the incidence of clinically significant bleeding between patients receiving Warfarin and those whose anticoagulation was adjusted to an international normalized ratio of less than 2.0, according to a retrospective chart review of arthrocentesis and joint injections. The most important aspect to keep in mind is to gradually advance the needle and reconsider the plunger until synovial fluid is visible.
The hand is required to be steady. The synovial fluid can then be sent for a cell count, crystallography, Gram staining, and culture. This could help in determining the cause of the knee effusion.
This approach allows for the microscopic examination of bacteria, crystals, or cells in the synovial fluid to assess for infection and inflammation. I can relieve the patient’s discomfort and determine the cause of the swelling by aspirating synovial fluid from the knee. This may lessen the chance that the arthritis will return.
Clinical Significance
For determining the source of pain relief, medication injection, or effusion drainage, arthrocentesis is done. The clinician is required to understand the anatomy to prevent complications. Making use of the right technique may decrease the possibility of complications.
The outcome of a successful knee aspiration is typically significant for crystal analysis. Gout (negatively birefringent urate crystals), pseudogout (weakly positive birefringent crystals), and an infectious process are frequently distinguished by the clinician.
The following features of synovial fluid are related to septic or infectious joint effusions:
- Above 25,000/microliter, the total white blood cell count is considered to be 75% sensitive and 75% specific.
- Above 50,000/microliter, the total white blood cell count is considered to be 60% sensitive and 90% specific.
- Above a microliter, the total white blood count is greater than 100,000 (about 20% sensitive, 99% specific).
- PMN cell proportion of 0.9 or greater (specificity: about 75%, sensitivity: about 80%).
- A concentration of more than 250 U/L of lactic dehydrogenase (LDH) (about 100% sensitive, 50% specific).
- Less than 0.5 for either synovial or serum glucose (about 50% sensitive, 85% specific).
- Greater than 3 g/dL of protein (roughly 50% sensitive, 50% specific).
Summary
The procedure called “arthrocentesis of the knee” is described in this protocol. It includes putting a needle into the knee joint and taking synovial fluid. To determine the type of knee effusion, synovial fluid may be taken for examination. A knee arthrocentesis is usually done while the patient is supine.
FAQs
What is a knee Arthrocentesis?
Arthrocentesis, or joint aspiration, is a medical procedure in which a physician takes fluid from a joint using a needle. A joint is formed where two bones converge.
What is the landmark for knee Arthrocentesis?
3–4 mm below the midpoint of the patella’s medial or lateral border, insert an 18-gauge needle (see the image below). Put the needle in the path of the intercondylar notch of the femur, perpendicular to the femur’s long axis. medial parapatellar approach for left-knee aspiration.
What are the locations for knee arthrocentesis?
After establishing the patella’s midpoint, they ought to place a needle 1 cm medially or laterally. Aim the needle up toward the joint space and posterior to the patella. Then, squeeze or “milk” the joint space on both sides to make aspiration easier.
What is the risk of knee arthrocentesis?
Blood clots may form in the joint capsule. An allergic reaction to the anesthetic happens in the patient. Blood or an infection may enter the joint capsule as a result of the needle puncture. According to experts, fewer than 0.01% of patients who receive joint injections experience infection.
Is knee arthrocentesis painful?
Since a local anesthetic is usually used, there won’t be much pain or discomfort. You can have it done in a hospital or your doctor’s office. Medical imaging techniques such as ultrasound can be used to confirm that the needle enters the joint capsule to decrease the risk of damaging other tissues.
What is the best approach for knee Arthrocentesis?
Insert the needle parallel to into the skin, then point it posteriorly, behind the patella, in the direction of the intercondylar notch. Try to maintain the needle’s trajectory horizontally to avoid making contact with articular cartilage. In addition, you can hold the patella and slowly pull it upward.
Who performs arthrocentesis?
Specialists in musculoskeletal issues and orthopedic surgeons can perform bursal aspirations and arthrocentesis. Physicians with training in internal medicine, emergency medicine, family medicine, and rheumatology may also carry out the procedure.
What are the indications for knee arthrocentesis?
Therapeutic: Taking large, painful joint effusions can help reduce pain. In addition, it can be used to inject some medications—mostly steroids—intraarticularly. Evaluate the way the treatment is working.
Diagnostic: Doctors may differentiate between septic arthritis and an inflammatory cause of bloody monoarthritis with precision by using synovial fluid analysis, which can also provide an apparent etiology of acute arthritis.
What is an arthrocentesis injection?
Your healthcare provider may help you in determining the cause of painful, swollen joints through arthrocentesis, also referred to as joint aspiration. Furthermore, it may reduce symptoms. A small needle is used by medical professionals to aspirate fluid out of the afflicted joint. Your doctor might inject medicine into the joint following aspiration.
What angle is arthrocentesis?
The needle is angled 45 degrees below the patella and 45 degrees distally into the knee. After placing the needle a quarter to an inch deep, aspiration is carried out, and the syringe ought to fill with liquid.
What fluids are used in arthrocentesis?
Although superimposed cellulitis is a relative contraindication to the procedure, arthrocentesis is required if infection is suspected. White blood cell count with differential should be performed on synovial fluid; this count will usually be elevated with polymorphisms visible in the differential count.
What to do after knee arthrocentesis?
Pain relief measures such as ice, elevation, and oral nonsteroidal anti-inflammatory drugs (NSAIDs) may be helpful.
What are the contraindications for knee arthrocentesis?
No absolute contraindications. Relative contraindications involve overlying cellulitis (potential intra-articular seeding of bacteria), coagulopathy/bleeding disorders, a joint prosthesis (preferably performed by orthopedic surgery in theatre ), acute fracture, adjacent osteomyelitis, and uncooperative patient.
Does fluid come back after knee aspiration?
An effusion is the accumulation of fluid inside a joint. After an important quantity of fluid is removed, an effusion frequently returns.
References
- Akbarnia, H. (2022, August 29). Knee Arthrocentesis. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK470229/.
- Image-www.msdmanuals.com%2Fprofessional%2Fmusculoskeletal-and-connective-tissue-disorders%2Fhow-to-do-arthrocentesis
- Villa-Forte, A. (2023, December 8). How To Do Knee Arthrocentesis. MSD Manual Professional Edition. https://www.msdmanuals.com/en-in/professional/musculoskeletal-and-connective-tissue-disorders/how-to-do-arthrocentesis/how-to-do-knee-arthrocentesis.
- Arthrocentesis: knee – WikEM. (n.d.). https://wikem.org/wiki/Arthrocentesis:_knee.
- Tieng, A., & Franchin, G. (2022, February 25). Knee Arthrocentesis in Adults. Journal of Visualized Experiments. https://doi.org/10.3791/63135.