Responsive Neurostimulation
What is Responsive Neurostimulation?
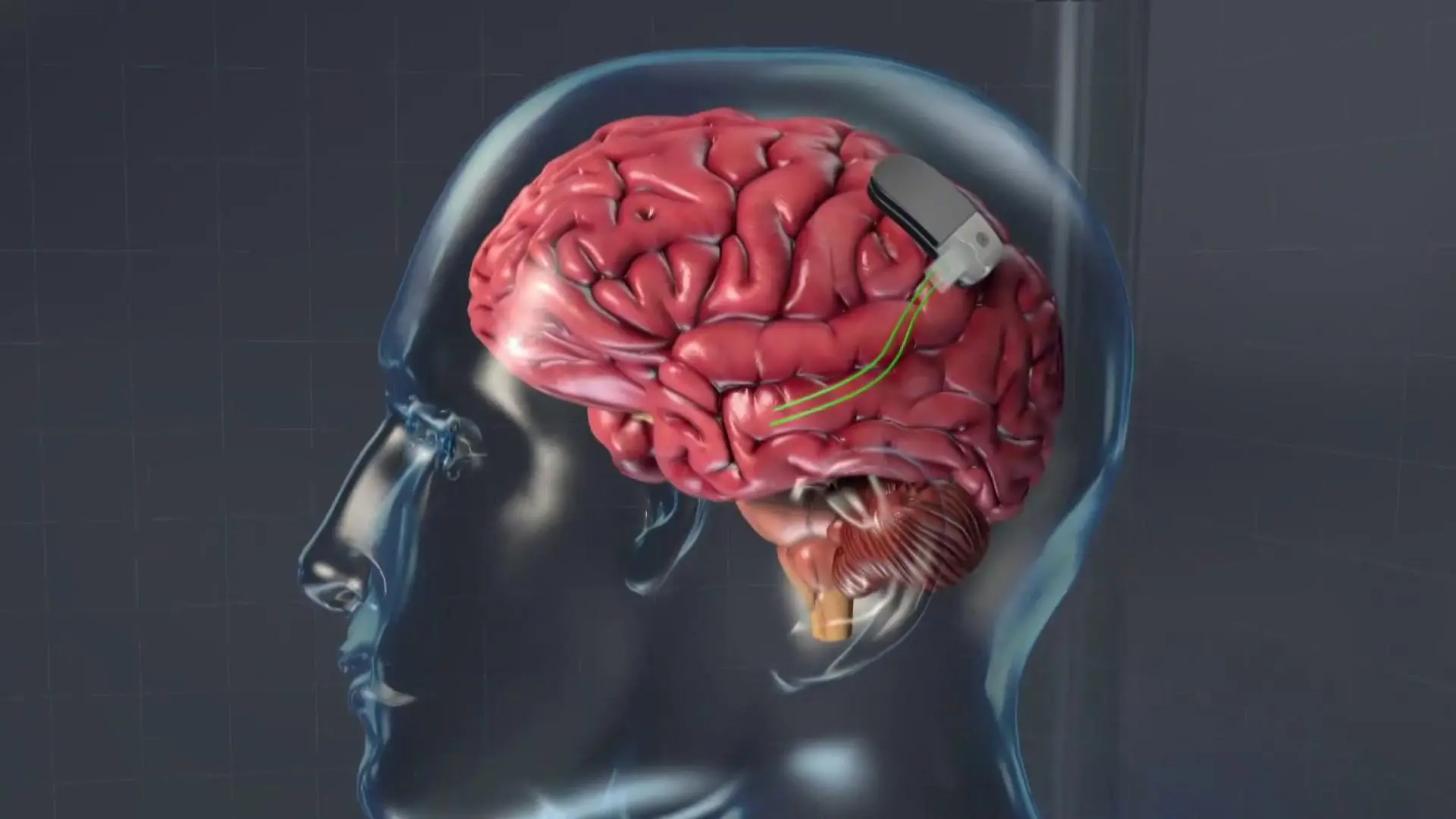
Responsive neurostimulation (RNS) is a breakthrough surgical method for managing seizures that are not managed by a drug. A neurostimulator is put underneath the scalp and within the skull, and it is attached to 2 electrodes put either on the surface of the brain, into the brain, or a mixture of both. The machine constantly monitors brain movement and then is programmed to detect seizures.
When a seizure or seizure-like movement is noticed, the machine produces a small portion of electrical current to the brain to stop or shorten the seizure, or perhaps control a seizure altogether.
The Responsive Neurostimulation – RNS machine curbs seizures by doing three crucial tasks:
Monitoring. Even during sleep, the machine observes brain waves for abnormal movement.
Detecting. The system can specify if the uncommon electrical movement is corresponding to a seizure.
Responding. When a seizure is about to start, the RNS system reacts in milliseconds. The machine transmits small bursts of stimulation to potentially control the seizure before it begins.
Who should get RNS?
The Responsive Neurostimulation – RNS system is used to manage grown-up people with focal epilepsy who have failed therapy with at least 2 seizure drugs. Our method is always first to decide whether people are prospects for resection of their seizure focus, the only possible cure for epilepsy. Persons are considered prospects for RNS when they have experienced comprehensive diagnostic testing that has localized one or two seizure foci but is chosen not to be candidates for surgical resection for a particular cause. These causes involve seizures that originate from more than one region of the brain, seizures that originate from regions of the brain that cannot be safely resected, or seizures that are hard to discretely localize.
How does RNS work?
Responsive Neurostimulation – RNS is a closed-loop method that continuously observes the brain’s electrical activity and transmits a short pulse of electrical stimulation straight to the brain when a seizure or seizure-like activity is noticed. Doctors or physicians specially qualified in RNS program the neurostimulator and slowly train it to notice precise ways special to a patient’s seizure.
How effective is RNS?
In clinical tests, more than half of the people managed with Responsive Neurostimulation – RNS had 50% or fewer seizures reached their presurgical baseline. The median reduction in seizure frequency with therapy was:
- 67% at 1 year
- 75% at 2 years
- 82% or better in years 3 through 6
Maybe more significantly, most persons noted marked progress in their quality of life with Responsive Neurostimulation – RNS.
It is necessary to maintain in mind that seizure decline from Responsive Neurostimulation – RNS is not quick. It may bring several months to see progress, and it will probably bring years to reach the optimal outcomes.
Side Effects of Responsive neurostimulation
Persons using the machine have not conducted many side effects. Side results during the implant surgery are more familiar but still very irregular; they contain:
- Bleeding
- Infection
- Pain
- Neurological deficiencies
There’s a small possibility that the electrical brain stimulation of the Responsive Neurostimulation – RNS machine may generate discomfort, but most patients don’t feel any stimulation from the machine.
The Placement Procedure
Responsive Neurostimulation – RNS is a breakthrough surgical method for managing seizures incapable to be managed by a drug. The RNS neurostimulator is a battery-powered machine put in a small tray in a kid’s skull by a pediatric neurosurgeon. It does not feel the brain, and it rests under the scalp, not seeable to the kid or anyone else.
The neurostimulator is linked to two tiny electrodes put either on the cover of the brain, into the brain, or a mixture of both. The neurostimulator is programmed by a pediatric neurologist to see a kid’s seizures, even during the duration of sleep. When a seizure or seizure-like movement is noticed, within milliseconds, the machine transmits short pulses to the brain to control, shorten or maybe even control the seizure entirely. The pulses standardize brainwaves, frequently before a kid can feel seizure symptoms.
The electrodes even continuously document and accumulate brainwave data, seizure movement, and patient improvement. This data provides us with a better knowledge of our person’s seizures, permitting us to create the best method of therapy in a real-time, ongoing causality.
The method generally needs only a 1 to a 2-night hospital stay, and the battery in the neurostimulator is calculated to last approximately eight years.
What are the patient’s responsibilities with RNS?
A person who selects therapy with the Responsive Neurostimulation – RNS system plays a key part in their care. Each person is provided a remote monitor, which is a laptop computer, to which they must download the data accumulated on their neurostimulator daily. This method brings just a few minutes a day. Once a week, they are invited to upload the data accumulated on their small monitor to a certain website database where their doctors or physician can examine it.
A person is provided a magnet and is requested to swipe the magnet over their neurostimulator when they have a seizure. This activity keeps that special event as necessary, and the machine stores the brain activity documented during that time so the doctor or physician can bring a closer look at it. It is also extremely useful for persons to maintain a detailed journal recording when they have a seizure. The patient must be ready and capable to hear the follow-up meetings so the machine can be programmed as required to gain the best outcomes. Generally, follow-up meetings are organized every 4-6 weeks throughout the first year but ultimately evolve less regularly.
FAQ
What is the success rate of responsive neurostimulation?
The moderate reduction in seizures was 67% after 1 year, 75% at 2 years, and up to 82% after 3 or more years of using Responsive Neurostimulation – RNS. So distant, approximately 3 out of 4 patients with the Responsive Neurostimulation – RNS System (77%) had their seizures cut in half after 2 years of operating it. Some patients had expanded times of being seizure-free as nicely.
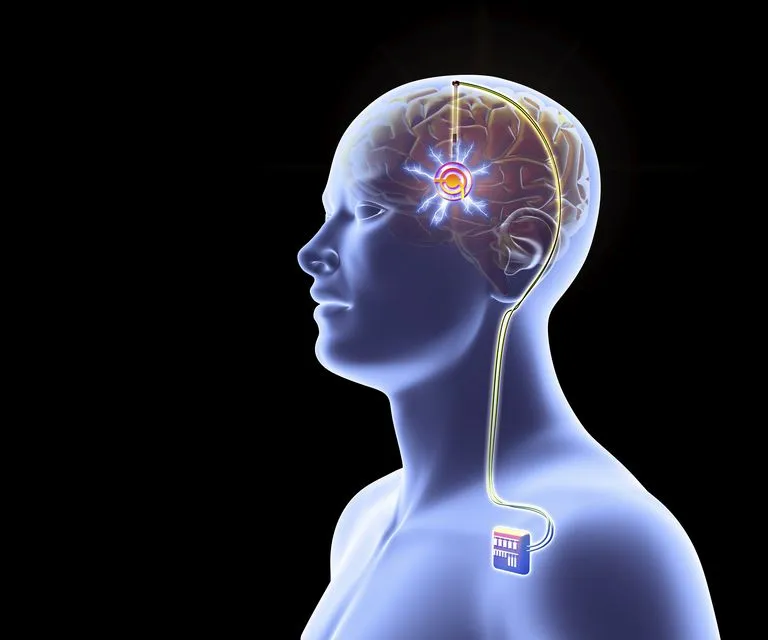
What is the difference between deep brain stimulation and responsive neurostimulation?
In deep brain stimulation, the leads are put in the thalamic anterior nuclei and the generator is even in the chest. In responsive neurostimulation, the area of the leads is infrequent, promoted up to 2 epileptic foci, and the generator is connected to the skull.
Does neurostimulation work for depression?
Vagus nerve stimulation (VNS) is a surgical method that can be operated on to manage those with treatment-resistant depression. A pacemaker-like machine, planted in the body, is connected to a stimulating wire that is interspersed along a nerve known as the vagus nerve.
What is neurostimulation used to treat?
Neurostimulators have been utilized to manage and ease symptoms of neurological diseases, involving pain, epilepsy, Parkinson’s disease, tremor, tinnitus, dystonia, incontinence, stroke, gastroparesis (GP), and obesity.
How long does Neurostimulator last?
Neurostimulator product life
Spinal cord stimulation systems (SCS) are created to stay for several years before requiring to be substituted. The neurostimulator may require to be substituted if the battery depletes or the machine malfunctions.