Genu Recurvatum and Physiotherapy Treatment
What is a Genu Recurvatum?
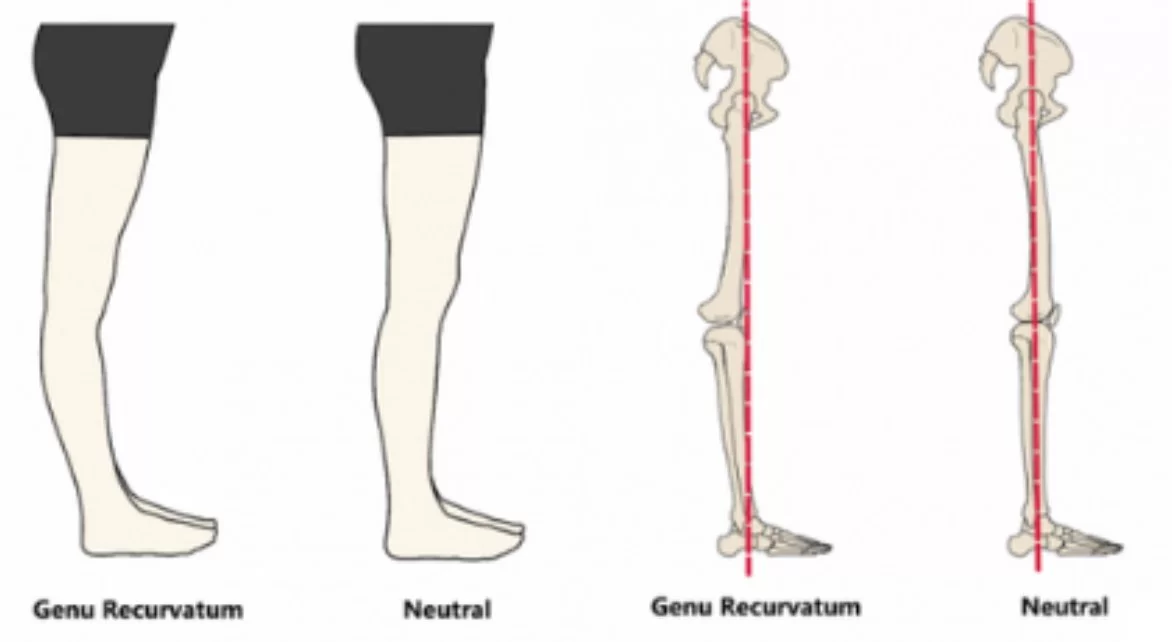
Genu recurvatum, also known as knee hyperextension, is a condition characterized by excessive extension or backward bending of the knee joint beyond its normal range of motion. In this condition, the knee joint extends backward, causing the lower leg to be positioned behind the thigh when standing upright.
- Knee recurvatum is a deformity in the knee joint so that the knee bends backward. In this deformity, excessive extension occurs in the tibiofemoral joint.
- this deformity is more common in women.
- The normal range of motion (ROM) of the knee joint is from 0 to 135 degrees in an adult. Full knee extension should be no more than 10 degrees. In genu recurvatum, normal extension is increased. The development of genu recurvatum may lead to knee pain and knee osteoarthritis.
Types of Genu recurvatum
Genu recurvatum can be classified as either congenital (present at birth) or acquired (developed later in life).
- Congenital genu recurvatum is often associated with other musculoskeletal abnormalities and may be caused by genetic factors or intrauterine positioning.
- Acquired genu recurvatum, on the other hand, can result from various factors such as ligamentous laxity, muscle imbalances, joint hypermobility, or previous knee injuries.
Genu recurvatum can vary from mild, moderate, to severe and is divided into three types :
- External rotary deformity (ERD)
- Internal rotary deformity (IRD)
- Non-rotary deformity
Causes of Knee recurvactum
- Inherent laxity of the knee ligaments
- Weakness of biceps femoris muscle
- Instability of the knee joint due to ligaments and joint capsule injuries
- Inappropriate alignment of the tibia and femur
- Malunion of the bones around the knee
- Weakness in the hip extensor muscles
- Gastrocnemius muscle weakness (in standing position)
- Upper motor neuron lesion (for example, hemiplegia as the result of a cerebrovascular accident)
- Lower motor neuron lesion (for example, in post-polio syndrome)
- A deficit in joint proprioception
- Lower limb length discrepancy
- Congenital genu recurvatum
- Cerebral palsy
- Muscular dystrophy
- Limited dorsiflexion (plantar flexion contracture)
- Popliteus muscle weakness
- Connective tissue disorders. In these disorders, there are excessive joint mobility (joint hypermobility) problems.
Symptoms of Genu recurvactum
- Pain on the outer back part of the knee is referred to as the posterolateral ligamentous.
- Aching pain in the medial tibiofemoral joint.
- The knee moves into hyperextension in the midstance phase.
- A nipping feeling in the front part of the knee
- difficulty walking or standing for extended periods, and compensatory changes in gait
- Individuals with this condition may experience difficulty in fully flexing the knee joint due to excessive extension.
Treatment of Genu recurvatum
Treatment for genu recurvatum depends on the underlying cause and severity of the condition. Conservative treatment options may include physical therapy to strengthen the muscles surrounding the knee, improve joint stability, and correct muscle imbalances.
Orthotic devices, such as braces or knee immobilizers, may be recommended to support the knee joint and prevent hyperextension. In cases where conservative measures are ineffective, surgical intervention may be considered to address the underlying structural abnormalities or correct ligamentous laxity.
Physiotherapy Treatment

- orthosis will be provided on the severity of the deformity
- ankle foot orthosis
- knee orthosis
- knee ankle foot orthosis.
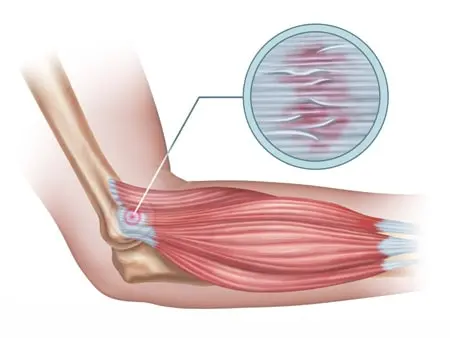
Pain relieving modalities

SWD: short wave diathermy is a deep heating modality that uses heat to provide pain relief, it improves the blood supply to targeted muscles, and removal of waste products. exercise therapy
Stretching of calf muscle :
seated calf stretch :
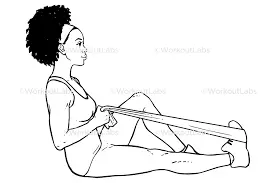
- Sit on the floor with your legs extended.
- Loop a long towel (or whatever tool you’re using) around one foot, holding both sides of it with your hands.
- Gently pull your toes toward your shin until you feel the stretch in your calf.
- Repeat on the other side.
Strengthening of gluteus muscle :
hip extension in a quadruped :

- How to: Get on all fours, with your hands stacked directly under your shoulders, and knees under your hips. Make sure your back is flat, and tuck your chin slightly so the back of your neck is facing the ceiling.
- Without rounding your spine, engage your lower abdominals. Keeping the 90-degree bend in your right knee, slowly lift your leg straight back and up toward the ceiling.
- Your max height is right before your back starts to arch, or your hips begin to rotate. Return to the starting position. Repeat all reps on one side, then switch legs.
Strengthening of knee muscles :
- Prone Theraband Knee Flexion: Theraband is a great tool to use with hamstring strengthening exercises.

- Starting Position: Tie the theraband so it forms a loop and hooks it around the foot of your good leg and the ankle of the leg you want to work. Lie on your stomach with your legs out straight.
- how to perform: Bring your heel towards your bottom pulling against the theraband as far as you can. Hold for 3-5 seconds and slowly lower the leg.
strengthening of calf muscles :
Double-Leg Heel Raise :
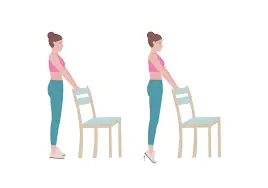
Builds concentric calf strength.
- How to do it: As with the assessment test, stand barefoot on the balls of your feet with your heels hanging off a step. Perform full-range-of-motion heel raises (with both legs) for four or five sets of six to ten repetitions, with a minute rest between each set.
- single-leg heel raise :

- How to do it: Stand barefoot on the balls of your feet with your heels hanging off a step. Hold on to a wall or doorframe for balance if necessary, but don’t use your hands for upward assistance. Lift one leg off the ground, and perform single-leg heel raises, also known as calf lifts, with the other.
- Move through a complete range of motion, from as low as you can go to as high as you can go. Try to do as many as you can with a full range of motion. Repeat on the other leg.
It is important to consult with a healthcare professional, such as an orthopedic specialist or a physical therapist, for an accurate diagnosis and appropriate management of genu recurvatum. They can assess the condition, identify any underlying factors contributing to the hyperextension, and recommend a tailored treatment plan.
Surgical Treatment
The standard course of therapy is to try a rehabilitation program to see if the patient can increase their overall quadriceps strength to make up for the symptomatic knee hyperextension if there are no related cruciate ligament and/or collateral knee injuries present. If this doesn’t work, a biplanar proximal tibial osteotomy, which involves raising the patient’s posterior tibial slope, may be necessary. Although they require substantial surgery, these procedures have been shown to reduce knee hyperextension and enable patients to resume their previous high level of functioning.
A proximal anteromedial or anterolateral osteotomy to improve the patient’s posterior tibial slope as a treatment for isolated genu recurvatum. After the osteotomy heals, these procedures have been found to be quite helpful in reducing a patient’s knee hyperextension and allowing them to resume greater activity levels.
Post-Operative Treatment
Combining the clinical examination with the abovementioned radiographs is crucial when creating a treatment strategy for a patient who presents with genu recurvatum. A physically supervised quadriceps strengthening program may be recommended for a patient if there are no evident collateral or cruciate ligament injuries.
A brace that seeks to prevent knee hyperextension may be recommended for patients who have previously participated in a rehabilitation program and/or who continue to experience knee hyperextension issues. In our experience, the majority of patients with this issue may temporarily benefit from a brace that restricts hyperextension but, in the long run, continue to experience symptoms and require surgical intervention.
Incidence
The congenital type of genu recurvatum is thought to impact 1 in 100,000 births, making it a rare ailment, however, it is a common aspect of some conditions, such as joint hypermobility, which affects 1 in 30 persons.
Summary:
Genu recurvatum, or knee hyperextension, is a condition where the knee joint extends backward beyond its normal range of motion. It can be congenital or acquired, with causes ranging from genetic factors to muscle imbalances or previous knee injuries. Symptoms include excessive backward bending of the knee, pain, instability, and difficulty walking.
Treatment options include physical therapy, orthotic devices, and surgery depending on the underlying cause and severity. Consulting with a healthcare professional is important for an accurate diagnosis and appropriate management.
FAQ
What is the most common cause of acquired genu recurvatum?
The most frequent cause of acquired genu recurvatum is polio. Compensatory: One may adapt hyperextension to make up for the opposite side’s shortening. Genu varum or valgum may be connected to recurvatum. Lower motor neuron lesion like post-polio syndrome, upper motor neuron lesion like hemiplegia.
What is another name for genu recurvatum?
Knee hyperextension and back knee are other names for genu recurvatum.
What orthosis for genu recurvatum?
In poststroke individuals with genu recurvatum, an articulated ankle-foot orthosis (AFO) has been demonstrated to be beneficial in reducing early stance knee moments.
Is genu recurvatum congenital?
A very complicated malformation of the knee joint is genu recurvatum. In this circumstance, the knee bends rearward with a significant extension of the tibiofemoral joint. It mostly affects women. A uncommon disorder called congenital genu recurvatum affects one in 100,000 newborns.
How do you diagnose genu recurvatum?
A malformation of the knee joint called genu recurvatum causes the knee to bend backward. The tibiofemoral joint extends excessively in this malformation. Knee hyperextension and back knee are other names for genu recurvatum. Women and those with a family history of ligamentous laxity are more likely to develop this deformity.





2 Comments