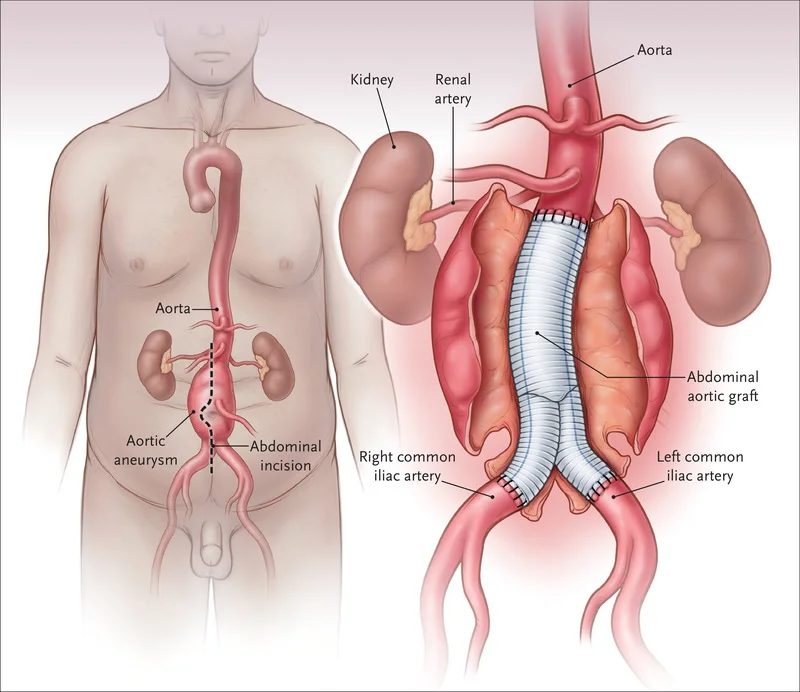
Abdominal Aortic Aneurysm (AAA)
An Abdominal Aortic Aneurysm (AAA) is a potentially life-threatening vascular condition characterized by the abnormal dilation or ballooning of the abdominal aorta, the large blood vessel that supplies blood to the abdomen, pelvis, and legs.
The aorta, when healthy, is a sturdy and elastic vessel, but when weakened, it can develop a localized bulge or aneurysm, particularly in the abdominal segment.
Introduction
- The biggest blood artery in the body is the aorta. It transports blood that has been oxygenated by the heart to every part of the body.
- An aortic aneurysm is a weak spot in the aortic wall that bulges. The blood vessel enlarges over time and becomes vulnerable to rupture or dissection.
- This may result in fatal bleeding and other serious health problems.
- The area of the aorta that passes through the abdomen is where aneurysms most frequently arise (abdominal aortic aneurysm).
- Another name for an abdominal aortic aneurysm is triple A or AAA. The section of the aorta that passes through the chest is known as a thoracic aortic aneurysm.
- An aneurysm will get larger and weaker over time after it has developed.
- An abdominal aneurysm’s treatment may either be removing or surgically repairing the aneurysm, or it may involve putting a metal mesh coil (stent) in place to support the blood artery and keep it from rupturing.
- Fusiform is the most typical type when the aorta swells out on both sides. Until an artery’s breadth grows by 50%, a bulging artery is not considered a real aneurysm.
- A single protrusion on the aorta is called a saccular form. This is referred to as a pseudoaneurysm at times.
- It often indicates a tear in the inner layer of the artery wall, which may be the result of arterial damage or an ulcer.
- Men, those over 50, and people with a family history of the condition are the groups most likely to develop AAAs. Smoking, hypertension, and other conditions affecting the heart or blood vessels are additional risk factors.
- Genetic disorders such as Ehlers-Danlos syndrome and Marfan syndrome are associated with a higher risk. The most prevalent kind of aortic aneurysm is AAA.
- The remainder either occur at or above the level of the kidneys, with around 85% occurring below the kidneys. In the US, males with a history of smoking between the ages of 65 and 75 are advised to undergo abdominal ultrasonography screening.
- In Sweden and the United Kingdom, screening is advised for all males over 65. Additional ultrasounds are usually performed regularly after the discovery of an aneurysm.
- Refusing to engage in The most effective method of preventing the illness is to smoke cigarettes. Treating high blood pressure, high blood cholesterol, and being underweight are other preventative measures.
- When a AAA’s diameter increases to more than 5.5 cm in men and more than 5.0 cm in women, surgery is typically advised. In addition, symptoms and a size expansion that is faster than one centimeter per year are causes for correction.
- Endovascular aneurysm repair (EVAR) or open surgery are the two possible methods of repair.
- Though it might not always be an option, EVAR has a shorter hospital stay and a lower short-term mortality risk than open surgery.
- There seems to be no distinction in the long-term results between the two. With EVAR, repeat operations are more frequent.
- 2-8% of males over 65 are affected with AAAs. In men, they occur five times more frequently. Less than 1% of those with aneurysms less than 5.5 cm will experience a rupture during the next year. The risk is around 10% for aneurysms between 5.5 and 7 cm and approximately 33% for individuals with aneurysms larger than 7 cm.
- Ruptures result in 85% to 90% mortality. Aortic aneurysms caused 168,200 fatalities in 2013, an increase from 100,000 in 1990.
- Between 10,000 and 18,000 people died in the US as a result of AAAs in 2009.
Causes of Abdominal Aortic Aneurysm (AAA)
- High blood pressure: The walls of the aorta may become weakened and damaged by high blood pressure.
- Blood vessel diseases: These are illnesses that result in inflammation of the blood vessels.
- Aortic infection: An abdominal aortic aneurysm may sporadically result from an aortic infection caused by certain bacteria or fungi.
- Smoking tobacco: Over 90% of those who get a AAA have smoked at some point in their life.
- Alcohol and hypertension: Another long-term cause of AAA is the inflammation brought on by chronic alcohol consumption and the hypertensive consequences of abdominal edema, which can result in hemorrhoids, esophageal varices, and other diseases.[Reference required]
- Genetic influences: Genetic factors have a significant effect. With a 20–30% risk, AAA is four to six times more likely in male brothers of known patients.
- Male individuals have the most noticeable family incidence rate.
- Regarding the precise genetic condition that may be responsible for the increased prevalence of AAA in male members of the afflicted families, there are several theories.
- Some assumed that the impact of a deficit in alpha 1-antitrypsin might be significant, however, additional research supported the idea that an X-linked mutation accounts for the reduced prevalence in heterozygous females.
- There have also been other theories developed about hereditary reasons. Furthermore closely linked to AAA are connective tissue diseases including Ehlers-Danlos syndrome and Marfan syndrome.
- An abdominal aortic aneurysm can be brought on by either pseudoxanthoma elasticum or relapsing polychondritis.
Symptoms of Abdominal Aortic Aneurysm (AAA)
- Approximately three of every four abdominal aortic aneurysms are asymptomatic. An X-ray, computed tomography (CT or CAT) scan, or magnetic resonance imaging (MRI) performed for other purposes may detect an aneurysm.
- An abdominal aneurysm is known as the “silent killer” since it can burst before a diagnosis is made and may not even show any symptoms.
- The lower back, groin, chest, or abdomen can all be the site of discomfort related to an abdominal aortic aneurysm. There might be dull or intense discomfort.
- Abdominal or back discomfort that suddenly becomes intense might indicate that the aneurysm is likely to burst. This is a medical emergency that might be fatal.
- Severe discomfort in your legs, lower back, or abdomen.
- Breathlessness.
- Rapid heart rate.
- Low pulse rate.
- Fainting or vertigo.
- Vomiting or nausea.
- Sweaty, clammy skin
- Additionally, pulsating sensations like those caused by abdominal aortic aneurysms can In the abdomen, a heartbeat.
- An abdominal aortic aneurysm might present with symptoms that mimic other illnesses or issues. See your doctor for a diagnosis at all times.
Pathophysiology
- The tunica media and intima layers of the aneurysmatic aorta exhibit the most notable histological alterations.
- Lipid build-up in foam cells, extracellular free cholesterol crystals, calcifications, thrombosis, and layer ulcerations and ruptures are some of these alterations.
- There is an adventitious inflammatory infiltration. Nonetheless, the primary pathophysiologic mechanism of AAA formation appears to be the breakdown of the tunica media by a proteolytic process.
- According to several studies, people with AAA had higher levels of matrix metalloproteinase expression and activity. As a result, the media loses its elastin, making the aortic wall more vulnerable to the effects of blood pressure.
- According to some accounts, the cleavage of decorin by the serine protease granzyme B may lead to the rupture of an aortic aneurysm. to a reduction in the adventitia’s tensile strength and a disturbed collagen arrangement.
- The abdominal aorta has less vasa vasorum than the thoracic aorta, which means that the tunica medium must rely mostly on diffusion for nourishment, leaving it more vulnerable to injury.
- The development of AAA, which preferentially affects the infrarenal aorta, is influenced by hemodynamics.
- The thoracic aorta and the infrarenal aorta have different histological structures and mechanical properties.
- From the root to the aortic bifurcation, the diameter reduces, and there is also less elastin in the infrarenal aorta wall. As a result, the abdominal aortic wall has a larger mechanical tension than the thoracic aortic wall.
- Additionally, the elasticity and distensibility decrease. with aging, which may cause the segment to gradually enlarge. In individuals with arterial hypertension, higher intraluminal pressure significantly accelerates the disease process.
- Adequate blood flow may be connected to certain intraluminal thrombus (ILT) patterns in the aortic lumen, which might influence the development of AAA.
Risk factors
- Tobacco use: The biggest risk factor for aortic aneurysms is smoking. The aorta is one blood artery whose walls might get weaker due to smoking. The risk of aneurysm rupture and aortic aneurysm is increased by this. Your risk of an aortic aneurysm increases with the amount and duration of tobacco usage. An abdominal aortic aneurysm can be detected with a single ultrasound for men 65 to 75 years old who smoke now or in the past.
- Years old: The age group 65 and above is the most common for abdominal aortic aneurysms.
- Family History: Abdominal aortic aneurysms occur in men far more frequently than in women.
- Having white skin: White people are more likely to have abdominal aortic aneurysms.
- background in the family. The risk is increased if there is a family history of abdominal aortic aneurysms. of being affected by the illness.
- Additional aneurysms: An abdominal aortic aneurysm may be more likely to develop if you have a thoracic aortic aneurysm, or if you have an aneurysm in another major blood vessel, such as the artery behind your knee
Diagnosis
- CT or CAT scans are other names for computed tomography scans: This test creates horizontal, or axial, pictures (commonly referred to as slices) of the body using X-rays and computer technologies
- CT or CAT scans are other names for computed tomography scans: This test creates horizontal, or axial, pictures (commonly referred to as slices) of the body using X-rays and computer technologies.
- A CT scan may provide extremely detailed images of any part of the body, including the muscles, organs, fat, and bones.
- CT scans supply more information than standard X-rays. CT scans offer greater detail than standard X-rays.
- MRI stands for magnetic resonance imaging: Large magnets, radiofrequency technology, and a computer are used in this test to create precise photographs of the body’s organs and structures.
- Echocardiogram, also known as an echo: This test uses sound waves captured on an electronic sensor to create a moving image of the heart and heart valves, as well as the structures inside the chest, to assess the structure and function of the heart such as the chest organs, the lungs, and the region around the lungs.
- echocardiography via the esophagus (TEE). This examination employs echocardiography to look for an aneurysm, heart valve problems, or a rupture in the aortic lining. The procedure for TEE involves passing a probe down the throat that has a transducer on the end.
- chest radiography: In this test, interior tissues, bones, and organs are imaged on film using invisible electromagnetic radiation beams.
- Angiogram, or arteriogram: This blood vessel X-ray picture is used to evaluate diseases including aneurysms, blood vessel constriction, and blockages. Through a thin, flexible tube inserted into an artery, a dye (contrast) will be injected. The blood vessels are made of dye.
- A physical examination, abdominal ultrasound, or CT scan is often used to detect an abdominal aortic aneurysm. When an aneurysm’s walls are calcified, the contour of the mass can be seen on plain abdomen radiographs. However, less than half of aneurysms will have an X-ray showing the outline. If an aneurysm is found, its size can be ascertained via ultrasonography. Furthermore, free peritoneal fluid is detectable. Although it is sensitive and noninvasive, its applicability may be restricted by obesity or the presence of intestinal gas. A CT scan may identify an aneurysm with about 100% sensitivity. It is also helpful for preoperative planning, providing information on the anatomy and potential for endovascular treatment. It is also capable of accurately detecting retroperitoneal fluid in cases of suspected rupture. Alternative, less common techniques use angiography and MRI to see an aneurysm.
- To evaluate the risk of a AAA rupture, it has been discovered that peak wall stress (PWS), mean wall stress (MWS), and peak wall rupture risk (PWRR) are more trustworthy metrics than diameter. An aneurysm ruptures when the mechanical stress (tension per area) surpasses the local wall strength. Utilizing conventional clinical CT data, medical software calculates these rupture risk indicators and generates a diagnostic of AAA rupture risk unique to each patient. It has been demonstrated that this kind of biomechanical method may precisely anticipate where AAA rupture would occur.
- Atherosclerosis: Because the walls of the AAA typically have an atherosclerotic load, it was long believed that the AAA was caused by atherosclerosis. Nevertheless, the process’s observed blockage and initial flaw cannot be explained by this theory. Another theory is that a build-up of plaque may result in a feed-forward malfunction in the communication between the neurons that control the aortic pressure.
Treatment of Abdominal Aortic Aneurysm (AAA)
- Preventing the rupture of an aneurysm is the aim of treatment for abdominal aortic aneurysms.
- Regular physical examinations and imaging, sometimes known as medical monitoring or watchful waiting, may be part of the treatment plan.
- Surgery. Treatment options for asymptomatic AAA include immediate repair, observation to eventually repair the damage, and conservative care.
- An AAA can be repaired with either open aneurysm repair or endovascular aneurysm repair (EVAR). If the aneurysm is larger than 5.5 cm or expands greater than 1 cm per year, an intervention is frequently advised. For symptomatic aneurysms, repair is also recommended. The total survival percentage ten years post-open AAA repair was 59%. The uncommon and potentially fatal disorder is known as mycotic abdominal aorta aneurysm (MAAA). Due to its rarity, there isn’t much sufficiently powered research or agreements on how to treat and monitor it.
Medical Examinations for Health
- All you may need to do if your abdominal aortic aneurysm is modest and not producing symptoms is to have regular check-ups and imaging tests to assess whether it is expanding.
- At least six months following diagnosis, a person with a minor, asymptomatic abdominal aortic aneurysm usually requires an ultrasound. Additionally, routine follow-up sessions should include abdominal ultrasounds.
- A medical professional looks for illnesses like high blood pressure that might exacerbate an aneurysm during routine exams.
- If the aneurysm is big or expanding quickly, which increases the risk of rupture, surgery can be required. Ruptures are more common in women than in males with big aneurysms.
- Currently, the only treatment option for suprarenal AAA (above the kidneys) in the United States is open surgery.
- However, endovascular device studies involving vascular surgeons at Johns Hopkins may offer an alternative. On the other hand, open or endovascular surgery can be used to treat AAA at or below the kidneys.
- Endovascular therapy is seen as less invasive and is defined as “within the blood vessel.”
- Endovascular treatment is an excellent alternative for those who cannot bear the danger of open surgery.
- Regretfully, not every patient can benefit from endovascular repair due to anatomical limitations.
- Speak with your vascular surgeon to determine which method is good for you.
- Beta Blockers: Although little data supports the use of beta blockers, it has been demonstrated that this innovation slows the rate at which AAAs are expanding, particularly in people with hypertension.
- Antibiotics: Research has demonstrated their ability to lessen inflammation in AAAs associated with a potential Chlamydia pneumonia involvement.
- Patients with AAA diameters between 3.0 and 4.0 cm are often placed on a waiting or monitoring list and should have medical imaging performed every two to three years.
- Every six to twelve months, the patient should have medical imaging performed if the AAA grows to a size of 4.0–5.4.
Surgery
Open aneurysm repair:
- To repair the aneurysm, a wide abdominal incision is performed. For the length of the aneurysm, another aortic incision is performed. For the repair, a graft—a cylinder—is utilized
- Polyester fabric or polytetrafluoroethylene (PTFE, nontextile synthetic graft) is used to make grafts. From slightly above the aneurysm site to slightly below it, the graft is sewn to the aorta. After that, the graft is sewn over by the artery walls.
Endovascular aneurysm repair (EVAR):
The procedure involves a little groin incision. A stent graft is transported to the aneurysm location and placed into the femoral artery under the supervision of X-rays. A stent is a long, thin tube made of metal mesh, whereas a graft is a mesh covering composed of PTFE, a polyester fabric.
The graft is kept open and in place by the stent. Only infrarenal (below the kidneys) AAAs are treated with EVAR. Patients at higher risk might be able to tolerate it more readily. But occasionally, the graft may come loose and require further adjustments.
Fenestrated stent graft:
- Open surgery was the previous standard of care for aneurysms that were juxtarenal, or at the kidneys, or that included the kidney arteries.
- This is so because the aorta’s branching to the kidneys is not accommodated by apertures in a conventional stent transplant.
- The renal (kidney) artery apertures in the fenestrated stent graft are precisely sized to match each patient’s aorta, ensuring that kidney circulation is maintained.
Aortic dissection: what is it?
- A rupture in the thoracic aorta’s inner layer of the aortic wall is the first sign of an aortic dissection. Three tissue layers make up the aortic wall.
- Blood is then directed into the aortic wall, dividing the layers of tissue, when a tear forms in the innermost layer of the wall. This leads to a possible rupture and weakening of the aortic wall. Aortic dissection may require immediate medical attention.
- Aortic dissection is most frequently diagnosed by abrupt, intense, persistent chest or upper back pain that is sometimes referred to as “ripping” or “tearing.” The discomfort can shift around.
- Upon confirmation of an aortic dissection diagnosis, prompt surgery is frequently done to the stent.
Aortic dissection: what causes it?
- Aortic dissection’s etiology is unknown. Nonetheless, several risk factors linked to aortic dissection include as:
- elevated blood pressure
- diseases of the connective tissue, including Turner’s syndrome, Ehlers-Danlos syndrome, and Marfan’s disease
- Aortic wall degeneration caused by cystic medial disease
- Aortitis, or aortic inflammation
- atherosclerosis
- Aortic valve with just two cusps, or leaflets, instead of the typical three cusps is known as a bicuspid valve.
- Trauma
- Aortic coarctation, or aortic narrowing,
- surplus volume or fluid in the blood (hypervolemia)
- A hereditary condition known as polycystic kidney disease is typified by the development of many fluid-filled kidney cysts.
Physical Therapy Management
- A physical therapist can offer education on risk factor reduction, quitting smoking to lessen the negative effects of smoking, screening for signs and symptoms, and public education that has increased awareness of the disease.
- At the moment, there is no conservative management to slow the progression of a AAA.
- Patients with AAA may benefit from improved cardiovascular fitness.
- Exercises that improve cardiovascular fitness (e.g., elliptical training, stair climbing, treadmills, cycle ergometers, and rowing three times a week for 45 minutes at a target intensity of 60% of HR reserve initially and working up to 80% as tolerated) and resistance training are safe in enhancing functional status, possibly lowering cardiovascular risk factors, and not increasing the rate at which patients with a AAA diameter progress.
- Pre-operative physical therapy has also demonstrated encouraging results in reducing the risk of complications following AAA surgery, while the exact mechanism is still unknown and needs more investigation.
- To reduce the risk of pulmonary problems, physical therapy for patients recovering from surgery should emphasize bronchial hygiene practices and incisional site check
Prevention
- There is currently no known mechanism to stop the formation of a AAA. If any of your biological parents, siblings, or children had a AAA, speak with your healthcare practitioner.
- To look for indications of the development of an aneurysm, they could suggest an ultrasound screening.
- You may take steps to minimize other risk factors and maintain your overall cardiovascular health whether or not you have a family history of AAA. Discuss with your supplier how to:
- Give up tobacco usage, including smoking.
- Create a fitness regimen that is good for you.
- Eat a heart-healthy diet.
- Control your blood sugar, cholesterol, and blood pressure.
- Limit your alcohol-containing drinks.
Prognosis
- While maximal diameter is the current criterion for measuring rupture risk, smaller AAAs (diameter<5.5 cm) are known to rupture as well as bigger AAAs (diameter>5.5 cm) that may stay stable. According to one research, the diameter of 10–24% of ruptured AAAs was smaller than 5 cm.
- Furthermore, it has been reported that out of 473 non-repaired AAAs that were analyzed from autopsy reports, 118 cases of rupture were found, with 13% of those cases having a diameter of less than 5 cm.
- Additionally, this study demonstrated that 54% of AAAs between 7.1 and 10 cm, or 60% of AAAs larger than 5 cm, never ruptured.
- Later, Vorp et al. concluded from Darling et al.’s observations that 7% (34/473) of patients would have died from rupture before surgical intervention if the maximum diameter criterion had been applied for the 473 individuals.
- Additionally, 25% (116/473) of cases could have required needless surgery because these AAAs might not have burst.
- There have been reports of other rupture evaluation techniques recently. Most of these strategies use the finite element method (FEM), a widely used engineering methodology, to perform a numerical analysis of AAAs to calculate the wall stress distributions.
- It has been demonstrated in recent papers that these stress distributions correspond with the AAA’s entire shape rather than just its maximal diameter.
- It is also recognized that failure is not entirely determined by wall stress alone.
- An AAA will often burst when the wall’s strength is exceeded by its stress. Because of this, if patient-specific wall strength and stress are combined, rupture evaluation could be more accurate.
- Other studies in the field have used more conventional methods to determine strength via tensile testing, but a noninvasive strategy for measuring patient-dependent wall strength was recently published.
- AAA wall stress, AAA expansion rate, degree of asymmetry, presence of intraluminal thrombus (ILT), rupture potential index (RPI), finite element analysis rupture index (FEARI), biomechanical factors combined with computer analysis, growth of ILT, geometrical parameters of the AAA, and a method of determining AAA growth and intensity are some of the more recently proposed AAA rupture-risk assessment techniques. breakup using mathematical models.
- Over several decades, the postoperative mortality rate for an already ruptured AAA has gradually declined, yet it still exceeds 40%.
- However, the postoperative mortality rate is significantly lower, at only 1-6%, if the AAA is surgically corrected before.
Summary
- Most AAAs are discovered by accident and are asymptomatic. Men of Caucasian descent, those over 60, and smokers have an increased prevalence of AAA.
- Imaging modalities are typically used to make the diagnosis. The risk of aneurysm rupture rises with increasing diameter, fast growth, symptomatic aneurysm, and smoking history. Aneurysm rupture is a medical emergency.
- For every symptomatic aneurysm and any asymptomatic aneurysm larger than 5.5 cm in diameter, surgery is advised. Imaging investigations should be performed on an asymptomatic basis on any aneurysms 3 cm to 5.5 cm in size as part of routine surveillance.
- Patients with small- to medium-sized aneurysms that are not surgically repaired may benefit from medical therapy with beta-blockers, quitting smoking, and managing risk factors, such as dyslipidemia and hypertension.
FAQ
What is the aneurysm summary?
An irregular enlargement or protrusion in the wall of a blood vessel, such as an artery, is called an aneurysm. Although aneurysms can form anywhere in the circulatory system, they most frequently occur in the brain’s blood arteries and in the aorta, the body’s major artery that spans the length of the trunk.
What is the aortic summary?
The biggest blood artery in the body is the aorta. The blood that is rich in oxygen is sent from your heart to the other parts of your body through this artery. The heart’s left ventricle is where the aorta starts, and it rises into the chest in an arch shape
Aortic aneurysm: what is it?
Bulges that resemble balloons develop in the aortic the major artery that supplies your body with blood rich in oxygen, the aorta.
Aortic aneurysm: what causes it?
An elevated blood pressure level is the primary cause of thoracic aortic aneurysms and can also increase the risk of abdominal aortic aneurysms. Thoracic aortic aneurysms are at risk due to bacterial infections. diseases of the kidneys, including polycystic kidney disease, chronic kidney disease, and renal failure.
How big is an aneurysm in the aorta?
An aortic diameter of more than 3.0 cm is usually regarded as aneurysmal in most adult patients. The typical diameter of the adult human infrarenal aorta is around 2.0 cm; 95% of adults have an aortic diameter of less than 3.0 cm.
References
- Abdominal aortic aneurysm: MedlinePlus Medical Encyclopedia. (n.d.). https://medlineplus.gov/ency/article/000162.htm
- Professional, C. C. M. (n.d.). Abdominal Aortic Aneurysm. Cleveland Clinic. https://my.clevelandclinic.org/health/diseases/7153-abdominal-aortic-aneurysm
- Abdominal aortic aneurysm. (2024, January 17). Wikipedia. https://en.wikipedia.org/wiki/Abdominal_aortic_aneurysm
- Abdominal Aortic Aneurysm. (n.d.). Johns Hopkins Medicine. https://www.hopkinsmedicine.org/health/conditions-and-diseases/abdominal-aortic-aneurysm
- Abdominal aortic aneurysm – Diagnosis and treatment – Mayo Clinic. (2023, April 25). https://www.mayoclinic.org/diseases-conditions/abdominal-aortic-aneurysm/diagnosis-treatment/drc-20350693
- Abdominal Aortic Aneurysm. (n.d.). Physiopedia. https://www.physio-pedia.com/Abdominal_Aortic_Aneurysm