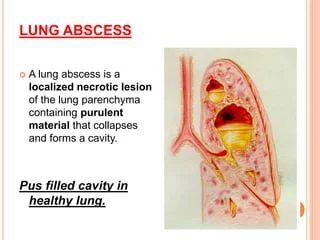
Lung Abscess
What is a Lung Abscess?
A microbial lung infection that causes the pulmonary parenchyma to necrotize is called a lung abscess. It can be categorized as acute (less than four weeks) or chronic (greater than four weeks) based on how long it lasts.
They can be categorized as primary if they arise without underlying pulmonary lesions or as secondary if they arise in the context of pulmonary lesions, depending on their cause. This exercise examines the reason for, pathophysiology, and clinical manifestation of lung abscesses while emphasizing the importance of the interprofessional team in treating these patients.
Defination
A localized deposit of pus within the lung that causes cavitation that usually has a thick wall is called a lung abscess. The most prevalent cause of abscesses is microbial infection, which results in lung parenchyma necrosis and the formation of one or more cavities.
When these cavities communicate with the bronchial tree, an x-ray of the chest shows air-fluid levels and a cough that produces purulent sputum.
Causes of Lung Abscess
If no probable pathogen is identified in the expectorated sputum, the abscess can be characterized as nonspecific. If an anaerobic bacteria is thought to be the source, the abscess can be characterized as rotten. The microbe that is generating the abscess defines the classification.
It is usually polymicrobial, involving anaerobic bacteria such as Prevotella, Fusobacterium, Peptostreptococcus, Bacteroides, or streptococci. Streptococci, Staphylococcus aureus, Klebsiella pneumoniae, Streptococcus pyogenes, Burkholderia pseudomallei, Hemophilus influenzae type b, Nocardia, and Actinomyces are the causative agents of monomicrobial lung abscess.
The most frequent bacteria linked to lung abscesses in persons with alcohol use disorders are Actinomyces, Klebsiella pneumoniae, Staphylococcus aureus, and Streptococcus pyogenes. An independent risk factor for the formation of a lung abscess is poor dental hygiene.
Pathophysiology
Lung abscesses are typically the result of aspirating oropharyngeal contents with anaerobes; this process begins as aspiration pneumonia, becomes worsened by pneumonitis, and, if treatment is not received, progresses to tissue necrosis in one to two weeks.
Causes of bronchiolitis include aspiration of oropharyngeal secretions, tumors, foreign bodies, swollen lymph nodes, and congenital malformations. Hematogenous spread is the method used in other situations. Infectious endocarditis, septic thromboembolism, and abdominal sepsis are common causes of hematogenous spread.
Symptoms of Lung Abscess
One of a lung abscess’s most obvious symptoms is a productive cough. Coughed material may have a bad smell and appear pus-like.
Common symptoms:
- bad breath
- High fever
- Breathlessness
- chest discomfort
- too much sweating day or night
- tiredness
- loss of weight
Differential Diagnosis
- Excavating bronchial carcinoma (squamocellular or microcellular)
- Excavating tuberculosis
- Localized pleural empyema
- Infected emphysematous bullae
- Cavitary pneumoconiosis
- Hiatal hernia
- Pulmonary hematoma
- Hydatid cyst of the lung
- Cavitary infarcts of lung
- Polyangiitis with granulomatosis (Wegener granulomatosis)
- Foreign body aspiration
- Septic pulmonary emboli
Diagnosis
Physical and History
Lung abscesses can be asymptomatic or present symptoms, depending on the patient’s immunological system. The history should concentrate on identifying individuals with immunological incompetence, oral or rectal instrumentation, intravenous drug misuse, recent upper respiratory illness, and conditions that put them at risk of aspiration (such as impaired cognition, loss of bulbar motor function, and immobility).
Depending on how close the abscess is to the airway, patients may present with fever, chills, weight loss, tiredness, loss of appetite, or a cough that is either productive or ineffective.
A lung abscess can be simplified by the examination of chest CT scans and X-rays. Lung abscesses show up as cavitary lesions with infiltrates on imaging examinations. Together with an abscess’s anatomic interactions, CT will be able to provide more precise information. Sputum microbiologic analysis may be able to help with management.
It should be considered to request specific cultures if the patient has a medical history that includes risk factors for fungus or mycobacteria. In rare instances, pleural fluid analysis and bronchoscopy with bronchoalveolar lavage have also been used.
Lung abscesses are more likely to form across the right middle and posterior segments of the lobes, then the superior segment of the right lower lobe, and occasionally the left lung in the event of aspiration of contents from the oropharynx.
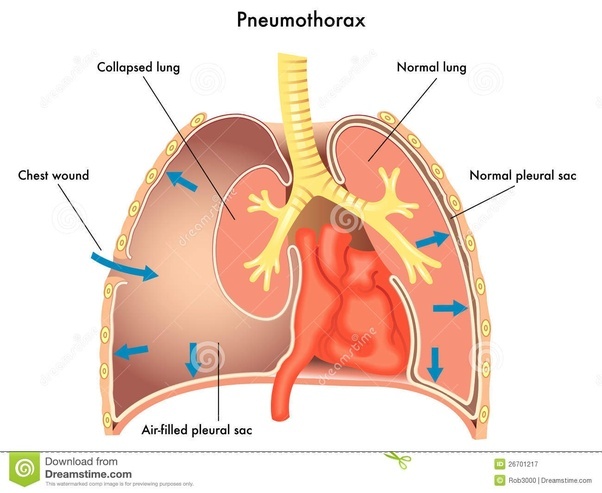
Pyopneumothorax or pleural empyema can result from a complicated lung abscess. Pleural fluid analysis can help with the diagnosis in specific cases. If a patient has impaired immune function, a lung abscess may become more complicated. With proper care, immunocompetent patients have a lower risk of problems, which often go away in three weeks. Blood cultures and echocardiography are crucial tools in the therapy of lung abscesses that result from hematologic spread.
Treatment of Lung Abscess
there is a possibility of a lung abscess, consider empirical antibiotic therapy. Targeted by empiric coverage should be colonized organisms seen in the oropharynx and upper airways, such as aerobic and anaerobic gram-negative bacilli, respiratory gram-negative cocci, and gram-positive cocci.
Consideration should be given to MRSA coverage if the patient was exposed to healthcare three months before to the presentation. When broad-spectrum antibiotic therapy is not helping an abscess, atypical organisms may be present.
Age, significant comorbidities, immunosuppression, bronchial blockage, and neoplasms are poor prognostic factors.
The recommended first line of empirical antibiotic therapy is beta-lactamase inhibitors (ticarcillin-clavulanate, ampicillin-sulbactam, amoxicillin-clavulanate, and piperacillin-tazobactam), which are followed by imipenem or meropenem. Clindamycin is still an option, however, it is no longer advised as a medication of choice for lung abscesses due to the possibility of Clostridium difficile infection continuing to be a penicillin allergy patient’s option.
The best treatments for methicillin-resistant Staphylococcus aureus (MRSA) are vancomycin or linezolid. When it comes to lung infections, daptomycin is ineffective. Cefazolin 2 g IV every 8 hours, nafcillin 2 gm IV every 4 hours, or oxacillin 2 gm IV every 4 hours are the recommended treatments for methicillin-sensitive Staphylococcus aureus (MSSA). In individuals with impaired renal function, dosage modification is taken into consideration.
The length of an antibiotic is typically three weeks, though this can change based on the patient’s reaction.
Once patients are stable, afebrile, and able to take an oral diet, think about transferring them to peroral (PO) antibiotics. The recommended medication for PO antibiotics for lung abscesses is amoxicillin-clavulanate.
Due to polymicrobial flora, metronidazole does not seem to be very helpful when used alone. Abscesses bigger than six centimeters (cm) may need to be surgically or percutaneously treated because they are unlikely to go away with antibiotic therapy alone.
Pneumonectomy or lobectomy is a surgical option that is taken into consideration for patients who do not respond to medicinal therapy.
Percutaneous and endoscopic drainage are taken into consideration for patients who are not good candidates for surgery.
When the clinical response is inadequate, associated conditions or alternative diagnoses are considered, especially for certain fungi and mycobacteria. Sometimes a parenchymal abscess is mistakenly diagnosed as empyema.
Chronic lung abscesses have been shown to benefit after antibiotic administration.
Additionally, underlying illnesses including infective endocarditis, septic thromboembolism, and others should receive comprehensive treatment in the event that hematologic causes of lung abscess occur.
Physiotherapy Treatment
A key component of lung abscess care is physiotherapy. Interventions in physical therapy should be used to encourage healing, enhance pulmonary function, and avoid problems. The following are a few common physiotherapy treatments for lung abscesses:
- Breathing Exercises: To help increase the clearance of secretions and prevent problems like atelectasis (partial or complete lung collapse), deep breathing and coughing exercises are frequently advised. These exercises are designed to increase lung capacity, develop stronger breathing muscles, and improve cough efficiency in order to help remove secretions.
- Airway Clearance Techniques: To help mobilize and remove secretions from the affected lung segment, a variety of airway clearance techniques, including postural drainage, directed coughing, and huffing, may be used. To help with secretion clearance, methods including vibratory positive expiratory pressure (PEP) therapy and chest physical therapy may be employed.
- Positioning and Mobilization: To maximize ventilation, relieve discomfort, and encourage lung expansion, physiotherapists may help with patient positioning. Reduced lung capacity and muscle weakness are two issues linked to prolonged bed rest that can be avoided with mobilization and mildly upright posture.
- Exercise Prescription: To prevent deconditioning, increase cardiovascular endurance, and improve general physical function, the patient’s condition may allow for the initiation of mild exercise and mobility training. Exercises for strength, endurance, and aerobic conditioning may be recommended, depending on the patient’s capabilities.
- Education and Self-Management: Educating patients is crucial. This can involve teaching them how to breathe properly, clear their airways, save energy, and follow at-home workout regimens. The key to the healing process is giving the patient the tools they must actively participate in self-management and use proper airway clearance treatments at home.
- Pain Management: Physiotherapists might present pain management plans and gentle approaches that reduce the patient’s discomfort while breathing and movement. if they are experiencing pain or discomfort related to the lung abscess. Facilitating pulmonary recovery, restoring respiratory function, and avoiding problems associated with immobility and reduced lung ventilation are the main goals of physical therapy in the treatment of lung abscesses.
Complications
The underdiagnosis, undertreatment, or ignored underlying cause of the lung abscess is what leads to complications. These consist of:
- Percutaneous fistula
- Bronchopleural fistula
- Trapped lung
- Pleural fibrosis
- Rupture into pleural space.
Prognosis
With a 90% cure rate, empiric antibiotic therapy is typically effective in treating primary lung abscesses. Targeted medication is then administered based on gram stain and culture results. Treatment of the underlying causes of secondary abscesses is necessary to ameliorate the situation.
Prognosis is poor, especially in immunocompromised patients and patients with bronchial neoplasm compared to primary lung abscesses with a mortality rate of around 75%.
Patient Education
The most crucial thing is to inform patients and their families about the risk factors for lung abscesses, such as avoiding excessive alcohol consumption, getting regular dental care, and elevating the head of the bed in cases when a patient is at high risk of aspirating.
They need to be taught how to recognize fever, dyspnea, coughing, and productive or nonproductive sputum as early indicators of a lung abscess.
Instructions about the importance of compliance with antibiotics and monitoring for side effects of medications to avoid complications are necessary.
Pearls and Other Issues
Aspiration of Oropharyngeal Secretions
- Dental and periodontal infection
- Paranasal sinusitis
- Altered level of consciousness
- Gastroesophageal reflux disease
- Frequent vomiting
- Intubated patients
- Patients with tracheostomy
- Vocal cord paralysis
- Alcohol use disorder
- Cerebrovascular accident (CVA)
Hematogenic Dissemination
- Abdominal sepsis
- Infective endocarditis
- Intravenous drug abuse
- Infected cannula or central venous catheter
- Septic thromboembolisms
Coexisting Lung Diseases
- Bronchiectasis
- Cystic fibrosis
- Bullous emphysema
- Bronchial obstruction such as enlarged lymph nodes, tumor or foreign body
- Congenital malformations
- Infected pulmonary infarcts
- Pulmonary contusion
- Bronchoesophageal fistula
Healthcare Team for Best Treatment
Identifying individuals at high risk of aspiration is critical, and patients who are at risk of developing a lung abscess due to inhaling oropharyngeal secretions should be placed on tight aspiration precautions. Aspiration pneumonia must be properly diagnosed and treated because delay or underdiagnosis can result in lung abscess and associated complications.
Patients who have severe Parkinson’s disease, severe Alzheimer’s disease, or are bedridden due to a CVA and hemiplegia, as well as postoperative patients who run the danger of aspirating, need to be closely watched. Patients who stay in the hospital for an extended time should receive enough physical therapy to prevent respiratory muscle fatigue, bed condition, and the eventual aspiration of oropharyngeal contents.
Conclusion
Most patients will benefit from antibiotics to fully recover. Plus, it’s best to start treatment as soon as possible. If you’re weak, unwell, have a compromised immune system, or have an airway-obstructing tumor, it can be more difficult for you to recover.
FAQs
What is the most common cause of lung abscess?
A pus-filled cavitary lesion is the characteristic of a necrotizing lung infection known as a lung abscess. Patients with reduced consciousness most frequently aspirate oral secretions, which is the most prevalent cause of it. Weight loss, sweating, fever, and productive cough are the symptoms.
What is another name for a lung abscess?
A lung abscess is characterized by pulmonary tissue necrosis and the development of cavities filled with fluid or necrotic debris as a result of microbial infection. Necrotizing pneumonia or lung gangrene are terms that are occasionally used to describe the development of several tiny (less than 2 cm) abscesses.
What antibiotic is good for lung abscesses?
Due to the polymicrobial flora, it is advised to treat lung abscesses with broad-spectrum antibiotics, such as a combination ampicillin/sulbactam (1.5–3 gr IV on 6 h) or clindamycin (600 mg IV on 8 h), followed by 300 mg PO on 8 h.
How do they remove an abscess in the lungs?
When surgery is necessary, lobectomies are typically used to treat big, central lesions. Small localized lesions may be treated with segmentectomy if no more normal lung tissue is implicated. Nowadays, computed tomography (CT) guidance is used to drain the majority of these lung abscesses.
What are the main symptoms of lung abscess?
Fatigue, appetite loss, night sweats, fever, weight loss, and a cough that produces sputum are some of the symptoms. The diagnosis is typically made with a chest x-ray. Antibiotics are typically required for a few weeks before a lung abscess heals.
What are the main complications of lung abscess?
The underdiagnosis, undertreatment, or neglected underlying cause of the lung abscess is what leads to complications. These consist of percutaneous fistula, bronchopleural fistula, trapped lung, pleural fibrosis, and rupture into pleural space.
References
- Sabbula, B. R. (2023, August 15). Lung Abscess. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK555920/
- Lung abscess – Symptoms, diagnosis, and treatment | BMJ Best Practice. (n.d.). https://bestpractice.bmj.com/topics/en-gb/927
- Gabbey, A. E. (2021, June 29). Lung Abscess. Healthline. https://www.healthline.com/health/lung-abscess