Prepatellar Bursitis and Physiotherapy management
What is a Prepatellar Bursitis?
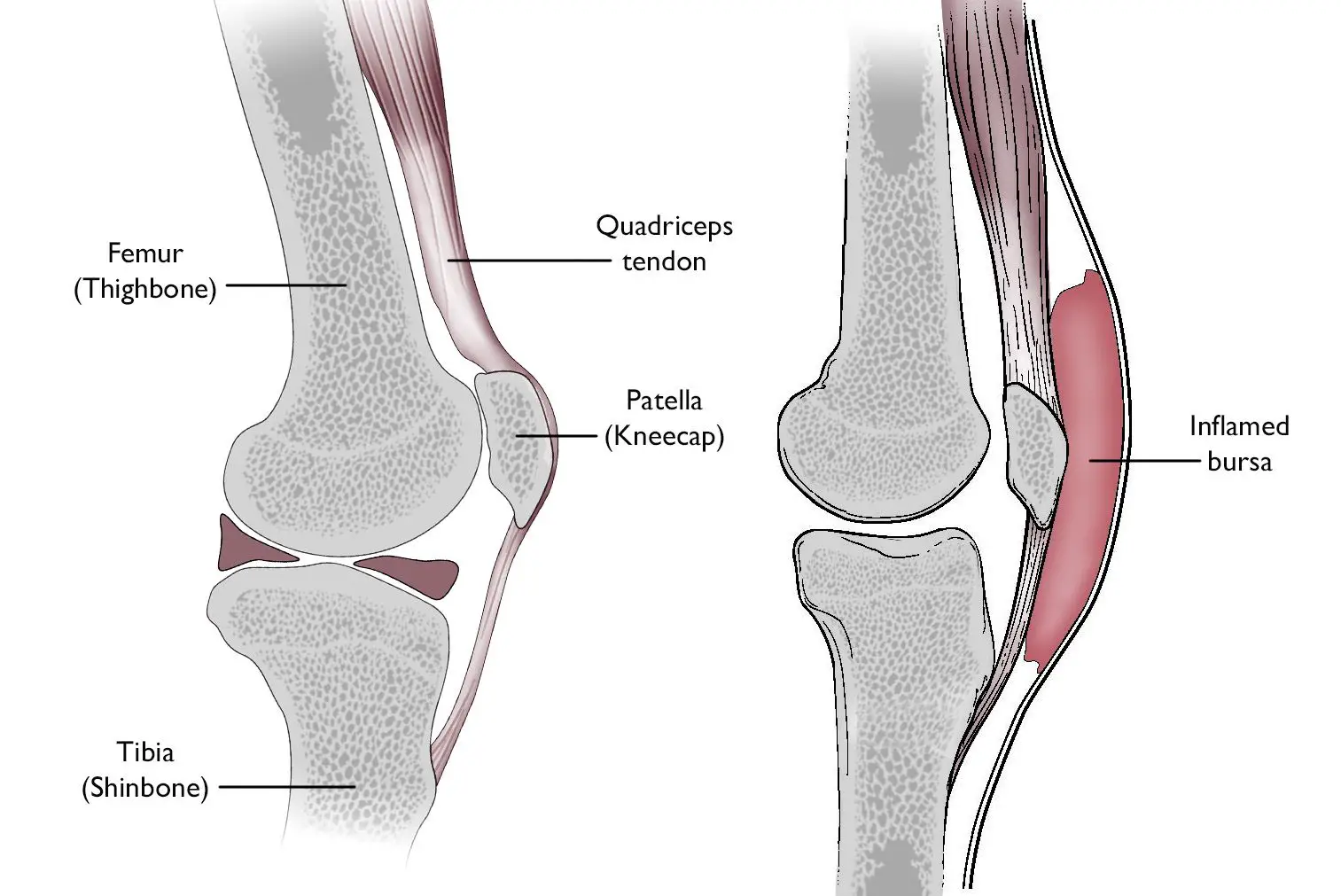
- Prepatellar bursitis is also called housemaid’s knee or carpenter’s knee. A bursa is a fluid-filled sac that ensures there is less friction between body parts. The prepatellar bursa is located superficially between the skin and the patella.
- The inflammation of a bursa is called bursitis. This inflammation can take the form of either an infectious nature or a non-infectious nature. A direct fall on the patella, an acute trauma, repeated blows, or friction on the knee may cause prepatellar bursitis.
- Other causes include infections or low-grade inflammatory conditions, such as gout, syphilis, tuberculosis, or rheumatoid arthritis.
- Prepatellar bursitis often occurs in specific jobs that involve a position where they work on their knees for a prolonged period of time such as miners, gardeners, carpet layers, and mechanics.
Anatomy related to Prepatellar Bursitis
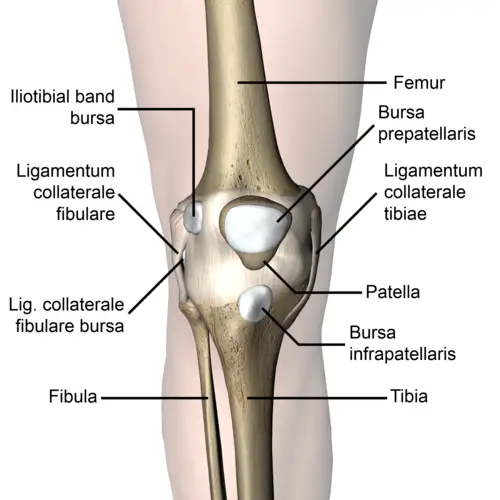
- The patella is a triangular-shaped bone in front of the knee. It moves up and down in the groove of the femur when you bend and straighten your knee.
- The patellar tendon is a thick structure that connects the bottom of the patella with the tibia.
- The upper part of the patella is connected to the quadriceps, which allows the knee extension and moves the patella upwards.
- Bursae around the knee can be divided into two groups- those around the patella (suprapatellar bursa, the superficial and deep infrapatellar bursae & prepatellar bursa) and those that occur elsewhere (pes anserine bursa, and the iliotibial bursa)
Causes of Prepatellar Bursitis
- Direct trauma/blow to the anterior knee
- Frequent falls on the knee
- Constant friction between the skin and the patella can be a cause of this condition. By the impact, the damaged blood vessels in the knee result in inflammation and swelling of the bursa. Actually, bacterial seeding of the bursal sac caused by a hematoma is rare, because of the limited vascular supply of the bursal tissue.
- Infection: Typically septic prepatellar bursitis is a break in the skin near the bursa, which leads to swelling and pain around this area. This happens when bacteria have passed across the soft tissues from a break in the skin and begin to multiply within the bursa. When a bursa is infected it can probably cause pain, fever, tenderness, and an elevated amount of white blood cells.
- Co-existing inflammatory disease- rheumatoid arthritis, gout, etc.
Symptoms of Prepatellar Bursitis
- Pain
- Swelling
- Differential warmth around the knee
- Painful and limited ROM at the knee
- If bursitis is caused by an infection, pain is associated with fever and chills.
Epidemiology
It is challenging to determine the precise incidence of prepatellar bursitis since a significant portion of cases that do not progress to the point of presenting to a healthcare facility are probably septic, and mild patients might never seek medical attention. Yet, the yearly incidence is thought to be 10/100,000, and men between the ages of 40 and 60 account for more than 80% of all cases of bursitis.
Although most of these instances are not septic, it is crucial to understand that up to one-third of them may show septic bursitis, which has a higher risk of morbidity. Prepactellar bursitis affects people of any age, however septic bursitis seems to affect kids more frequently. Bursitis is more common in those with long-term immunosuppressive diseases like diabetes mellitus.
Pathophysiology
An increase in bursa blood flow, leukocyte migration into the bursa, and fluid generation from the bursa’s synovial cells provide the basis for the inflammatory response observed in bursitis. Septic bursitis can result from hematogenous dissemination, direct inoculation, overlaying skin and soft tissue infections, or trauma itself.
A direct microscope study of the bursa’s synovial fluid may identify germs, crystals of calcium pyrophosphate dihydrate, gout, or other causes of inflammation. Tumor necrosis factor-alpha, different interleukins, and cyclooxygenases are examples of inflammatory mediators that are likely to be enhanced when fluid is molecularly examined.
Differential Diagnosis
Prepatellar bursitis is frequently mistaken for other conditions that can cause knee pain, such as:
- Medial Collateral Ligament Injury
- Lateral Collateral Ligament Injury
- Osteoarthritis
- Pes Anserinus bursitis
- Posterior Cruciate Ligament Injury
- Rheumatoid Arthritis
- Patellar tendon rupture
- Chondromalacia patellae
- Patellofemoral pain
Diagnosis of Prepatellar bursitis
- Bursitis can be diagnosed through a detailed history (about the onset of symptoms, the pattern of knee pain and swelling, and how the symptoms affect their lifestyle)and a physical examination, however, X-ray, MRI, and CT-scan can be done to rule out the possibility of a fracture or soft tissue injury.
- If it is uncertain whether or not the bursa is infected, an arthrocentesis can be done. It is typically done for three reasons: necessary information is needed to make a diagnosis, to relieve the pressure in the joint, and will help alleviate the pain and excess fluid also needs to be removed before a therapeutic injection is given.
Physical examination in Prepatellar bursitis
Physical examination involves checking for:
- Differential warmth around the knee
- Erythema
- Tenderness
- Swelling
- Pain
- Range of motion
- When there is a limited range of motion or swells, a doctor may recommend using a needle and syringe to remove the fluid from the joint. This fluid can be sent to labs for testing whether or not the bursa is infected.
- Common tests for infection are gram stain, white blood cell count (an elevated number of white blood cells in the synovial fluid indicates infection), and glucose levels tests (when the levels are significantly lower than normal it may indicate an infection).
- Gram stain is used to determine if there are certain troublesome bacteria present. Not all bacteria can be identified. Even when the test comes back negative, septic bursitis cannot be completely ruled out.
Medical management of Prepatellar bursitis
- The treatment for prepatellar bursitis depends primarily on the cause of the bursitis and secondarily on the pathological changes in the bursa.
- The primary goal of treatment is to control the inflammation.
- Conservatively, the R.I.C.E regime in the first 72 hours after the injury or when the first signs of inflammation appear.
- Medications including non-steroidal anti-inflammatory drugs, and topical medications- creams, sprays, gels, and patches can provide pain relief when they are directly applied to the skin over the knee. To reduce the gastrointestinal side effects that can be caused by oral medications, topical medications may be a good choice. Also, for cases of septic prepatellar bursitis, antibiotics are used to treat the infection.
- Corticosteroid injections
Surgical management of Prepatellar bursitis
- When conservative treatments have failed for chronic/post-traumatic prepatellar bursitis, outpatient arthroscopic bursectomy under local anaesthesia is an effective procedure.
- Arthroscopic or endoscopic excision of the bursa has more recently been reported to have satisfactory results with less trauma than open excision.
Physiotherapy management of Prepatellar bursitis
- SHORT WAVE DIATHERMY(SWD): short wave diathermy is a deep heating modality that uses heat to provide pain relief, it improves the blood supply to targeted muscles, and removal of waste products.
- TENS: transcutaneous electrical nerve stimulation is an electrical modality that provides pain relief by providing pain modulation.TENS closes the gate mechanism at the anterior grey horn in the spinal cord. also stimulates the endogenous opioid system which prevents the release of substance p at the anterior grey horn.
- Rest: Rest prevents the worsening of the initial injury. By placing the injured extremity to rest the first 3-7 days after the trauma, we can prevent further retraction of the ruptured muscle stumps (the formation of a large gap within the muscle), reduce the size of the hematoma, and subsequently, the size of the connective tissue scar.
- During the first few days after the injury, a short period of immobilization accelerates the formation of granulation tissue at the site of injury, but it should be noted that the duration of reduced activity (immobilization) ought to be limited only until the scar reaches sufficient strength to bear the muscle-contraction induced pulling forces without re-rupture At this point.
- gradual mobilization should be started followed by a progressively intensified exercise program to optimize the healing by restoring the strength of the injured muscle, preventing muscle atrophy, the loss of strength, and extensibility, all of which can follow prolonged immobilization.
- Ice or cold application: It is thought to lower intra-muscular temperature and decrease blood flow to the injured area. Regarding the use of cold on injured skeletal muscle, it has been shown that early use of cryotherapy is associated with a significantly smaller hematoma between the ruptured myofiber stumps, less inflammation and tissue necrosis, and somewhat accelerated early regeneration.
- However, according to the most recent data on the topic, icing of the injured skeletal muscle should continue for an extended period of time (6 hours) to obtain a substantial effect on limiting the hemorrhaging and tissue necrosis at the site of the injury.
- Compression: This may help decrease blood flow and accompanied by elevation will serve to decrease both blood flow and excess interstitial fluid accumulation. The goal is to prevent hematoma formation and interstitial edema, thus decreasing tissue ischemia. However, if the immobilization phase is prolonged, it will be detrimental to muscle regeneration.
- Cryotherapy, accompanied by compression, should be applied for 15–20 min at a time with 30–60 min between applications. During this time period, the quadriceps should be kept relatively immobile to allow for appropriate healing and prevent further injury.
- Elevation: The elevation of an injured extremity above the level of the heart results in a decrease in hydrostatic pressure, and subsequently, reduces the accumulation of interstitial fluid, so there is less swelling at the place of injury. But it needs to be stressed that there is not a single randomized, clinical trial to validate the effectiveness of the RICE principle in the treatment of soft tissue injury.
- Once the initial inflammation has reduced a program of stretching and light strengthening will be initiated to restore full motion and improve strength to reduce stress on the tendons and knee joint. Therapeutic exercises to strengthen and stretch the muscles of the knee. This includes static contraction of the quadriceps.
- This should be an exercise that the patient can do at home 1 to 3 times a day. The objective of rehabilitation is that the patient can resume their everyday activities. To see if the exercise is working you have to put your fingers on the inner side of the quadriceps, you will feel the muscle tighten during the contraction of the muscle.
- The patient has to hold his contraction for 5 seconds; the exercise can be repeated 10 times as hard as possible. It is important not to forget this exercise must be pain-free.
- Also, the stretching of the quadriceps is a good exercise for the patient, it reduces the friction between the skin and the patella tendon. There is less friction when the patella tendon is more flexible. The physiotherapist can also help the patient by using electrotherapy modalities and patient education on the use of knee pads for kneeling activities.
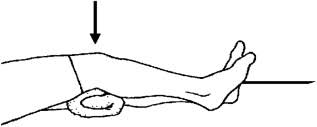
- isometrics exercise of quadriceps will help to maintain muscle power of quadriceps muscle, Isometrics: Initial isometrics with quadriceps contractions done with the knee fully extended and in different positions at 20-degree increments as knee flexion improves May discontinue isometrics when the patient can sit comfortably.
- Straight leg raises: Sit flat on the floor with the legs straight out in front of you. Raise one leg off the floor keeping the knee straight. Hold for 3 to 5 seconds before lowering back to the ground. Repeat 10 to 20 times. This exercise can be done daily. Progress the exercise by increasing the length of hold and the number of reps.

- Strengthening exercises and stretching: when the pain has reduced sufficiently, strengthening and stretching exercises can begin and these can then be built up gradually. The most effective form of muscle training in cases of tendon problems is eccentric training because the collagen fibers will be set in the right/functional direction.
- For the popliteus, eccentric strengthening (closed kinetic chain) of the quadriceps is effective in reducing strain on the popliteus.
- Patients should not run until the knee is free of pain, then they should limit their workouts and downhill running for at least 6 weeks. During the treatment, cycling provides a good alternative exercise.
How to Prevent Prepatellar Bursitis?
By following these easy tips, you may help avoid bursitis.:-
- If you perform knee exercises or engage in contact sports like basketball, football, or wrestling, wear kneepads.
- Regularly take a break to extend your legs and rest your knees. To prevent your knees from being overly stressed, you may also think about regularly changing up your activities.
- After working out, elevate your knees and apply ice.
Complications
The appearance of infection is the main side effect of prepatellar bursitis. Other complications, such as infection from bacteria injected through needle aspiration, a fistula between the skin surface and bursa following needle aspiration, subcutaneous atrophy from corticosteroid injections, bleeding following injections, and even rupture of the patellar tendon, are more likely to be secondary to management options.
Patient Education
The focus of patient education will be prevention. The right measures to prevent knee damage include avoiding kneeling as much as possible and, for those who are unable to do so, using protective gear such as large knee pads. Knee protectors may also be helpful in preventing the less frequent episodes caused by injuries associated with sports.
Prognosis
The majority of prepatellar bursitis instances have no long-term adverse effects and may be treated at home with rest, ice, and elevation. Treatment for chronic prepatellar bursitis may be more challenging, particularly if work involves a lot of kneeling. A treatment plan that is customized to your needs and circumstances will be developed by your healthcare team.
Infected prepatellar bursitis can have serious side effects, including septic shock and even death if it is not treated. If you think you may have an infection, you should visit the closest hospital or get in touch with your doctor immediately.
Summary
Prepatellar bursitis is a common condition that is generally treated with rest, pain medication, and Physical therapy exercises. See your doctor if your prepatellar bursitis is interfering with your daily activities or if it doesn’t improve within a few weeks. Make careful to get medical attention as soon as you notice any infection-related symptoms, such as fever or redness and warmth in the affected region.
FAQ
What is the best treatment for prepatellar bursitis?
The majority of prepatellar bursitis instances have no long-term adverse effects and may be treated at home with rest, ice, and elevation. Treatment for chronic prepatellar bursitis may be more challenging, particularly if work involves a lot of kneeling.
Will prepatellar bursitis go away?
An injury-related case of prepatellar bursitis will often heal on its own. Over several weeks, the bursa will absorb the blood within it, and it should recover to normal.
Who gets prepatellar bursitis?
Constant kneeling pressure is a common cause of prepatellar bursitis. The disorder is more common in coal miners, plumbers, roofers, carpet installers, and gardeners.
Is walking OK for knee bursitis?
Walking may make knee bursitis symptoms worse, so it’s critical to pay attention to your body’s signals and take it easy if you’re in discomfort. However, walking can assist in decreasing inflammation and is unlikely to do further harm to the joints.
Is massage good for prepatellar bursitis?
For those suffering from bursitis, massage therapy might be quite beneficial. Massage treatment can help the body repair itself and recover more quickly from bursitis by reducing pain and increasing blood flow to the affected areas. Reducing compression and relieving pressure on the bursa are the objectives of therapy.
What is the fastest way to heal the bursitis of the knee?
Several times a day, apply an ice pack to your knee for 20 minutes at a time until the pain subsides and the area no longer feels warm to the touch. Put compression on it. Swelling can be lessened by using a knee sleeve or compressive wrap. Raise one knee.





4 Comments