Lyme Arthritis
What is Lyme Arthritis?
Lyme disorder is caused by the bacterium Borrelia burgdorferi and infrequently, Borrelia mayonii. It is transferred to humans via the bite of infected black-legged ticks. If Lyme disorder isn’t detected and treated with antibiotics promptly, the disease can ultimately spread via the body. The most familiar late-stage symptoms involve joint swelling and pain, a condition called Lyme arthritis.
What Are the Stages of Lyme Infection?
There are three-3 stages:
- Early localized Lyme: Flu-like symptoms such as chills, fever, swollen lymph nodes, headache, sore throat, and a rash that appears like a bull’s eye or is rounded and red in color and at least two inches long
- Early disseminated Lyme: Flu-like symptoms such as weakness, pain, or numbness in your arms and legs, differences in your vision, heart pulsations and chest ache, a rash (that may or may not be a bulls-eye rash), and a variety of facial paralysis called Bells palsy
- Late disseminated Lyme: This can happen months, weeks, or years after the tick bite. Symptoms might involve severe fatigue, arthritis, dizziness, trouble sleeping, headaches, and confusion.
About 10% of humans treated for Lyme infection don’t have a surprise for the disorder. They may move on to have three core symptoms: fatigue, joint or muscle pain, and short-term memory defeat or confusion. This is known as post-treatment Lyme disorder syndrome. It can be difficult to diagnose because it has the exact symptoms as other conditions. Plus, there isn’t a blood test to prove it.
Specialists aren’t confident why Lyme symptoms don’t always go out. One idea is that your body maintains fighting the sickness even after the bacteria are moved, such as an autoimmune disorder.
Lyme Disease symptoms
Early symptoms and signs (3 to 30 days after tick bite)
- Fever, headache, chills, muscle and joint aches, fatigue, and swollen lymph nodes may appear in the lack of ras Erythema migrans (EM) rash
- This happens in about 70 to 80 percent of infected humans
- Starts at the site of a tick bite after a wait of 3 to 30 days (standard is about 7 days)
- Develops slowly over several days running up to 12 inches or more (30 cm) across
- May sense warm to the contact but is infrequently itchy or painful
- Occasionally clears as it widens, resulting in a target or bulls-eye impression
- May happen in any region of the body
- Does not ever seem like a classic erythema migrans rash
Later symptoms and signs are seen (days to months after the tick bite)
- Extreme headaches and neck immobility
- Other EM rashes on other regions of the body
- Facial paralysis (loss of muscle control or droop on one or both sides of the face)
- Arthritis with extreme joint ache and swelling, especially the knees and further large joints.
- Irregular pain in muscles, tendons, joints, and bones
- Heart palpitations or an uneven heartbeat (Lyme carditis)
- Episodes of dizziness or shortness of breath
- Inflammation of the brain and spinal cord
- Nerve pain
- Shooting aches, numbness, or tingling in the feet or hands
Lyme Arthritis Symptoms
- By the period late-stage Lyme infection has evolved into arthritis symptoms, the pain senses separate from those early flu-like symptoms.
- The early stages of Lyme disorder are more compatible with a viral infection where you type of pain all over. Possibly some achiness in the joints and all-around discomfort, but its more generalized and there’s no associated swelling
- Here are some features that determine late-stage Lyme arthritis from other kinds of arthritis:
- Lyme arthritis is not symmetric on both sides or both extremities. This is unlike many kinds of inflammatory arthritis, like rheumatoid arthritis.
- Lyme arthritis generally causes aches in only a rare joint. It generally causes pain in rarer than five joints or junctions at a time occasionally even in only one joint. Lyme arthritis most frequently affects the knee joint and ankle joint, but it can impact other joints also.
- Lyme arthritis pain isn’t consistent. It also generally isn’t sufficient to maintain a person from walking.
- Lyme arthritis ache could look more painful than it touches. A human can get a very swollen knee joint, but that, paradoxically, is not very acheful.
- Nevertheless, the symptoms of Lyme arthritis can simulate other kinds of arthritis, which can cause it tricky to diagnose, particularly if the people never saw a tick or has reason to doubt they have Lyme disease.
What does the rash look like?
A few Lyme rashes look like a bull’s eye with a circle near the center. But most are rounded, red in color, and at least two-2 inches across.
The rash gradually brings bigger over several days. It can increase to about 12 inches across. It may sense warm to the touch, but it’s generally not itchy or painful. It can show up on any portion of your body.
How small are ticks?
Ticks arrive in three sizes, depending on their life phase. They can be the size of a seed of sand, a poppy source, or an apple source.
How to prevent tick-borne illness
High-risk areas for infection involve the Atlantic coast from Maine to Virginia, as well as Minnesota, Wisconsin, and Michigan. Lyme disorder was one-time infrequent in Canada but has been steadily ratcheting its range northward as a consequence of weather changes.
If you live in a region where Lyme disease is familiar, some simple measures can minimize the risk of tick bites:
- Avoid scrubby regions with bushes, tall grass, and leaf debris, where ticks abound.
- When walking in the woods, stick to the middle of the tracks.
- Tick repellents including picaridin, IR3535, or 20% DEET will supply several hours of defense to exposed skin.
- Clothing and camping equipment can be treated with jets including 0.5% permethrin.
- Looking at your body in a full-length mirror will allow you to recognize and dismiss ticks.
- When scanning children for ticks, pay particular awareness to the shoulder blades, the scalp, and ears, the belly button, the waist, behind the knees, and between the legs.
- Ticks are helpless to heat and dehydration. Washing your dresses in hot water, or placing them in the dryer on elevated heat, should destroy ticks secreting in them.
- If you discover ticks connected to your body, help fine-tipped (jeweler) tweezers to pull them. Hold them next to the skin and use constant, delicate pressure. Do not pull or twist the tick, as this may cause its mouth portions to break off and remain implanted in your skin.
- Do not use nail polish or petroleum jelly to the tick, or try to steam it off.
- Wash the bite site with iodine, soap, water, or rubbing alcohol.
- If you produce a rash at the bite site or sense ill, see your doctor or physician.
Whos likeliest to get Lyme Arthritis?
Boys up to age 15 and males between the ages of 40 and 60 are the most possible to get Lyme disorder. That’s because they manage to play outside and proceed to hunting, camping, and hiking.
Some humans think Lyme illnesses are less familiar in older teens and males in their 20s because those groups are the potential to be inside and on a computer. And by the same ticket, they may be more familiar with older grown-ups because they manage to work in their backyards, which is where most Lyme infections occur.
How do you know if you’ve been bitten?
Since ticks are so short, you’ve acquired to have pretty fine eyes to see them.
If you have a little, red spot on your skin that appears like a mosquito bite, it could be a tick bite. If it goes out in a few days, it’s no trouble. Recognize, a tick bite doesn’t necessarily indicate you have Lyme disorder.
If you detect a rash in the form of a bull’s-eye, you might have a tick bite. Talk to your doctor or physician about treatment.
If you have an allergic response to ticks, you’ll immediately detect a bite.
Differential Diagnosis
- Acute memory disorders
- Ankylosing spondylitis and rheumatoid arthritis
- Atrioventricular nodal block
- Cellulitis
- Contact dermatitis
- Gout and pseudogout
- Granuloma annulare
- Prion-related diseases
Physical examination
Peoples with Lyme arthritis generally have the subsequent features on physical examination:
Monoarthritis or oligoarthritis most typically involves the knee joint, but other large or small joints or junctions may be involved, like an ankle, elbow, shoulder, or wrist.
Involved knee joints may have very large effusions with warmth, but in contrast with specific bacterial (e.g., staphylococcal) septic arthritis, they are not significantly painful with a range of movement or weight bearing. Bakers cysts may be present in the knee joints given the large length of effusions.
Fever is generally not present.
Treatment of Lyme Arthritis
Medical Treatment
With early-stage Lyme disorder, you will carry antibiotics for about 10 days to 3 weeks. The most familiar ones are cefuroxime, amoxicillin, and doxycycline. The antibiotics will nearly never heal your infection. If they don’t, you might bring other antibiotics either by mouth or as a shot.
If you don’t treat your Lyme disease, you might require verbal antibiotics for symptoms like weakened facial muscles and uneven heartbeat. You may require antibiotics if you have meningitis, inflammation in your brain and spinal cord, or more extreme heart issues.
If your Lyme is at a late stage, the doctor or physician might give you antibiotics either by mouth or as a shot. If it generates arthritis, you’ll get arthritis treatment.
There’s no treatment for post-treatment Lyme infection syndrome.
Physiotherapy treatment in Lyme Arthritis
Early-stage Lyme disorder can only minister with antibiotics and other adjunct drugs like analgesics. Some doctors or physicians will refer people with chronic Lyme disorder symptoms that do not reply to medicine to physical therapy. The function that physical therapy plays in the therapy of Lyme disorder is primarily to:
- Reduce pain
- Prep de-conditioned patients to start a home-based exercise schedule
- Familiarize patients with proper activity techniques and frequency, period, and resistance suitable to achieve fitness uses without worsening Lyme-related symptoms.
Physical therapy interventions involve:
- Massage
- Range of motion
- Myofascial release
- Modalities involve moist heat, ultrasound, and paraffin.
- Normally, ice packs and electrical stimulation are contraindicated, though there is no study to reinforce this.
- Exercise prescription aims to enhance strength and slowly increase the patient’s activity level, which may be hardly impaired as an outcome of chronic Lyme infection. Whole-body workouts typically feature ample stretching, light exercise, and light resistance exercise with low loads and high repeats.
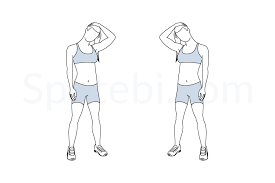
Shoulder stretch
Get your left arm across your body and keep it with your right arm.
Keep for nearly 30 seconds.
Change arms and repeat it again.

Knee to chest stretch
Lie on your back in a supine position with the backs of your heels flat on the bottom.
Slowly drag one knee joint up to your chest, sensing a stretch in your lower back.
Maintain the opposite leg rested.
Keep for nearly 30 seconds.
Change legs and repeat it again.

Neck stretch
Flex your head barely to the right side.
With your right hand, slowly drag your head below, experiencing a comfortable stretch along the left side of your neck.
Keep for nearly 30 seconds.
Change sides and repeat it again.
Rolling with a foam roller
One item you can efficiently do at house is to roll tight tissue in your body with a foam roller. This assists to lengthen and dismiss stress in your fascia, or connective tissue. (Fascia involves the connective tissue that sheaths each muscle, and even the tendons and ligaments.)
Rollers are affordable and available online. Only play with slowly moving the muscles encircling painful joints or junctions, or really any aching muscles at all, with the roller.
Gentle strengthening
Mild strengthening of the muscles that keep joints involved by Lyme arthritis can assist decrease inflammation and reducing pain. This type of strength work is special to each person. For instance, if a patient has an ache in her knee, which of the muscles that connect to the knee joint are weak, and desires to strengthen them in a form that relieves pain
Strengthening brings time and patience but is nearly ever helpful. It’s worth discovering a skilled physical therapist or Pilates instructor to assist you with this type of work.
Yoga
If you’ve attended it once, you’ve listened to it a million times: Yoga is excellent for detox! But also for patients with low energy. Begin with mild/newbie classes, then as your energy boosts, blend it up if you sense confidence! You understand your body the best so don’t experience something like hot yoga unless you understand the heat won’t reach you. A person who can’t control her temperature, I didn’t try hot yoga until two months after therapy, with an abundance of fluids.
Light Weight Lifting
Chronic Lyme can generate muscles to weaken and shrink. The heart, nerves, lungs, and liver were also involved. Light weight-lifting/toning and light activity classes permitted me to maintain some muscle and strength, my body collaborated more and then went into healing, and the change was smoother.
Walking
If you’re in your 20 or 30, walking doesn’t just sound like performing out. But during therapy, if it’s all you can accomplish, then accomplish it! Begin with 15 minutes per day, and performed way up to a regular 30. Don’t force yourself too difficult, but any exercise will help.
Bicycling
Low-impact way of bringing good activity. cycling has been a great cardio replacement.
Stair-Stepping
It assisted in gain power in the legs.
FAQ
My blood tests still test positive for Lyme disease even after my antibiotic course. Do I still have the disease?
Your immune system is running to continue producing antibodies against the bacterium for months or occasionally years after you were contaminated. That’s why the tests still show favorable results. This does not suggest you have the disorder now.
Does everyone with Lyme disease get a rash?
No, not everyone with Lyme infection brings a rash. The rash is not ever-present or efficiently recognizable in early Lyme infection. The rash can frequently be missed or misunderstood as a spider bite when not a stereotypical bull’s eye impression Some patients reach numerous rashes from the spread of the Lyme infection bacteria via the bloodstream
Is the maternal transmission of Lyme disease possible?
Untreated Lyme infection during pregnancy can conduct in an infection of the placenta, and the infection can extend from mother to fetus. The CDC says that with proper maternal antibiotic therapy there is no raised risk of adverse birth consequences. However, there are no posted studies evaluating the developmental effects of children whose mothers acquired Lyme infection during pregnancy. More study is required to sufficiently understand maternal transmission and its possible risks.
What is the prognosis after treatment of Lyme disease?
Most patients diagnosed and treated early with antibiotics get sounder Yet, 10% 20% of early interpreted/early treated people produce chronic ongoing symptoms The risk of chronic symptoms is increased if the initial disorder is more extreme or if there are neurologic symptoms Early diagnosis and therapy generally enhance prognosis
If you get Lyme disease can you get it again?
Yes, you can bring it also Spirochetes may navigate ways that interrupt immunologic memory If you’re reinfected with exactly the exact strain you may have some opposition However, there is not much data to illustrate how defensive immunity to following infections may or may not be developed






2 Comments