Mannerfelts Syndrome
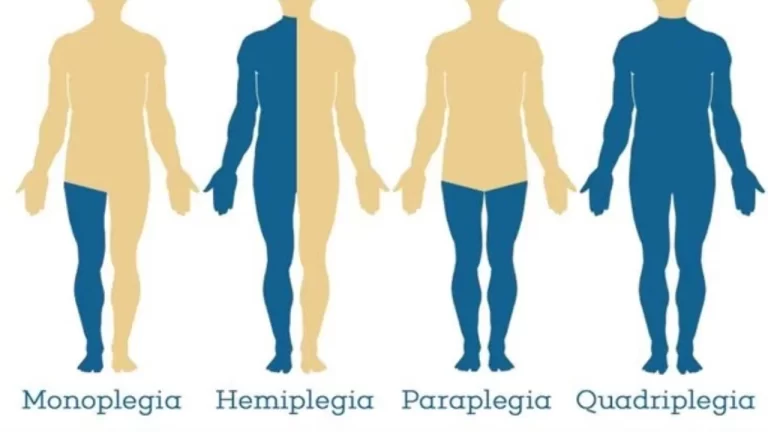
Mannerfelt’s Syndrome, also known as Mannerfelt lesion, is a rare but significant condition associated with chronic rheumatoid arthritis (RA). It specifically involves a rupture or attrition of the flexor pollicis longus (FPL) tendon, which is the tendon responsible for the flexion of the thumb.
Rheumatoid arthritis (RA), which results in joint deformity and persistent inflammation, is frequently linked to this injury. Thumb bending is controlled by the FPL tendon, which runs through a groove in the distal radius, one of the forearm bones. People with RA are especially susceptible to damage to this tendon.
Others broaden the term to include the index and long fingers’ lack of flexibility at the distal IP joints. Some researchers and publications characterize Mannerfelt syndrome 1 as total non-flexion at the thumb’s interphalangeal (IP) joint.
More prone to rupture are the flexor digitorum profundus (FDP) and superficial (FDS) tendons that supply the index and long fingers, after the rupture of the flexor pollicis longus (FPL) tendon in the thumb. This could lead to conflation.
Patients may be reluctant to seek medical attention and diagnoses may be delayed since tendon rupture can occur without pain.
Introduction
Some researchers and publications characterize Mannerfelt syndrome 1 as total non-flexion at the thumb’s interphalangeal (IP) joint. Others broaden the term to include the index and long fingers’ lack of flexibility at the distal IP joints.
When the tendon that attaches the flexor pollicis longus (FPL) to the thumb ruptures, the flexor digitorum profundus (FDP) and superficial (FDS) to the index and long fingers become more vulnerable to rupture, this could lead to conflation.
The systemic cause is most commonly rheumatoid arthritis (RA). Patients may be reluctant to seek medical attention and diagnoses may be delayed since tendon rupture can occur without pain.
What is a Mannefelt Syndrome?
- A fracture of the pollicis longus tendon caused by a bone spur in the carpal tunnel results in Mannerfelt syndrome.
- There is a connection between rheumatoid arthritis and the basal pores in the carpal tunnel.
- Mannerfelt states that a torn tendon in the flexor pollicis longus is the most prevalent injury. The syndrome is hence known as Mannerfelt. In Mannerfelt syndrome, there is no discernible breakdown in the processes.
- The pseudorandom or peritoneal sheath is where the long flexor tendon of the wrist continues when it is injured.
- Most people have very little or no flexion of their distal phalanx.
- Both the flexor tendon and flexor tendons can sustain injuries that impact the ulna.
- One frequent kind of treatment is surgery.
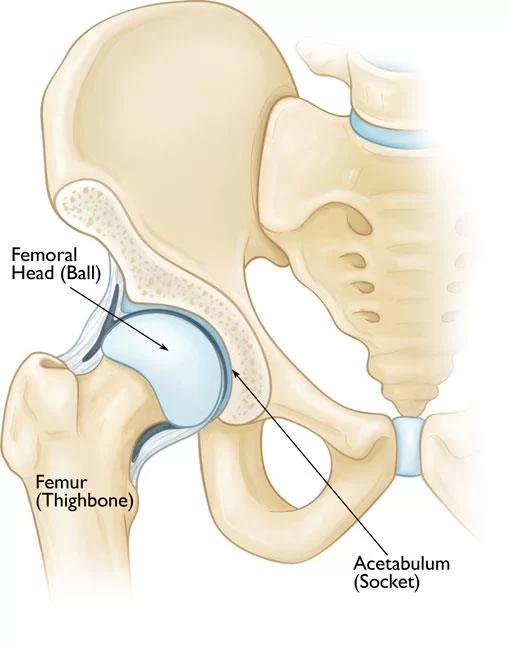
Flexor pollicis longus anatomy
Resides on the flexor digitorum profundus’s lateral side.
Origin:
- Originating from the anterior surface of the radius, the fibers stretch almost to the wrist before the tendon forms, next to the anterior surface of the ulna’s coronoid process between the pronator quadratus and the radial tuberosity above and below it. The tendon goes behind the retinaculum flexor.
Insertion
- The palmar/volar region outside the base of the thumb’s distal phalanx
Action
- The thumb’s flexor at the interphalangeal joint, which also flexes the thumb at the metacarpophalangeal and carpal joints, is crucial for all hand-grabbing activities.
Pulley system in hand
- An essential anatomical feature to consider while discussing the hand’s tendon system is the pulley system.
- The ring pulley system’s job is to prevent the tendons from bending during vigorous flexion by keeping them near the bone.
- It is possible to digitally bend the cruciform pulley system without it becoming deformed because it is foldable and flexible.
- Patients who have had tendon repair may occasionally develop spring pain following the procedure, therefore this should be kept in mind when providing care.
- Therapists can consider the pulley system’s clinical cause more effectively when they are aware of its anatomy and function.
Mechanism of injury
- The most frequent reason for flexor tendon injury is volar/palmar rips.
- Patients typically visit the hospital right away due to the likelihood that they have suffered a significant injury, which is too horrible. It can occur with associated neurovascular disease.
- A rip, such as when the FPL tendon is pulled from its original location, is an alternate mode of damage.
Distal phalanx –
- Usually as a result of an injury’s closed mechanism.
- This is typically the outcome of a forceful extension that takes place during active flexion.
- This happens when a player grips their opponent’s shirt (shirt finger), bends their finger, and is forced to stretch, as in ball sports, or when they engage in rock climbing.
What is the cause of Mannerfelt syndrome?
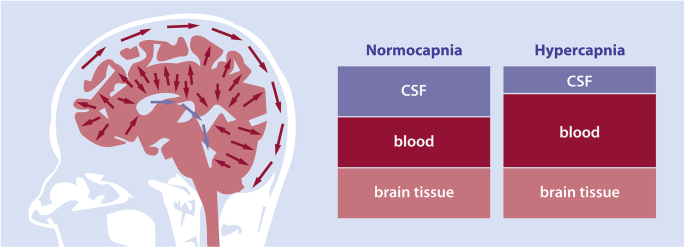
- The carpal flexors’ continual traction from the weakened ligaments between the carpal bones in rheumatoid arthritis leads to the carpal bone’s voluntary subluxation.
- The distal volar vasculature and proximal volar trapezium erode as a result of destructive rheumatoid arthritis, which follows nutritional vessels.
- Sharp bones are created by osseous tissue erosions, which further chill the carpal tunnel floor and aggravate the flexor tendon.
- The flexor pollicis procumbent tendon ruptures as a result of tendon support.
- The dorsum, trapezius, distal ulna, hamate, lunate, distal radius, and sesamoid of the ulna are the most often torn places.
What is the prognosis of Mannerfelt syndrome?
- Following the permanent restoration of the flexor pollicis longus tendon injury through index finger flexor digitized sublimes grafting, the patient’s prognosis was assessed.
- The prognosis is good if the interphalangeal joints can move again.
- The least complicated cases occur when tendon reconstruction ruptures or interphalangeal fusions occur.
What are the symptoms of Mannerfelt syndrome?
- Rheumatoid arthritis is common in people with Mannerfelt syndrome.
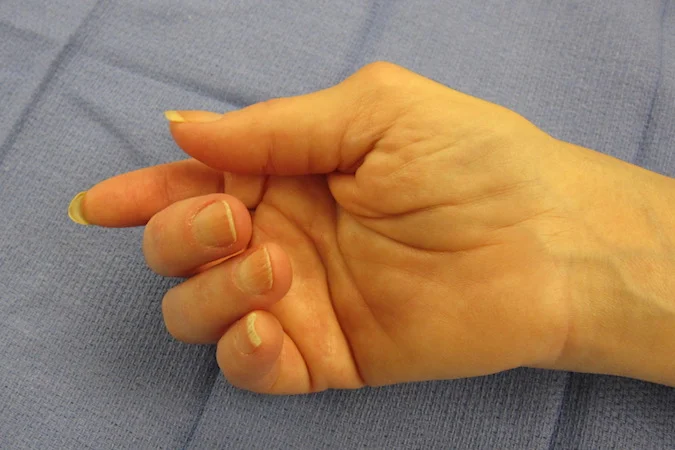
- A Mannerfelt lesion is easily identified during a physical examination since the tendon of the long flexor pollicis is the only muscle that flexes the thumb’s interphalangeal joint.
- When an interphalangeal joint is stabilized and the patient is asked to flex it, it indicates a tear if the patient is not able to do so.
- Partial anterior intercostal nerve palsy and flexor pollicis longus tendon rupture share comparable clinical manifestations. It’s distinguishable by a basic test.
- A medical professional dorsiflexes a patient’s wrist.
- As well as the carpal and wrist joints, the thumb is hyperextended at the metacarpophalangeal joint.
- When an examination is done, the interphalangeal joint flexes naturally and accepts passive stretching if the flexor longus tendon is paralyzed but intact.
- A rupture of the tendon of the long flexor pollicis is indicated by the interphalangeal common remaining extended.
Diagnostic procedures
- Pollicis Flexor: The longus tendon flexes each interphalangeal (IP) joint of the thumb separately.
- X-rays: they could show a fracture.
- Ultrasound: a tool for evaluating possible damage.
- MRI
Outcome measures
- Force of pressure
- Dash
- Measurement using goniometry
Complication
Therapists who treat patients with flexor tendon injuries need to take into account several issues, such as:
Rupture
- Particularly during the first course of the six-week loading period, be cautious about rupture. Symptoms of a ruptured tendon could be:
- When the joint separates, patients with FDP Tendon may experience active flexion of the DIP joint.
- Patients may not have active PIP joint flexion if the PIP is isolated, according to FDS Tendon Repair.
- The patient might not have isolated flexion of the IP joint after FPL tendon repair.
- You must get in touch with your surgeon right once if you suspect a patient may have a ruptured tendon.
An infection
During surgery, there is always a chance of infection, therefore it’s critical to let the surgeon know if any symptoms emerge. Indications of inflammation to be aware of include:
- Redness surrounding and inside the wound
- The presence of muddy or foul-smelling wound drainage
- A fever or rise in temperature near the wound
- A bad odor emanates from the wound.
Contractures
- It could happen to someone who has had FDS and FDP tendon repair.
- After surgery, a patient may require a dynamic splint if they develop a contracture, usually 8 to 10 weeks later.
- For the first six weeks, patients should aggressively stimulate stretching, particularly in the posterior side of the PIP joint splint, and undertake exercises in the back block splint to prevent contractures.
- Moreover, it eliminates flexor adhesions and PIP joint contracture.
Scar Adhesions
- The patient’s flexor arch and finger may have limited flexion and extension, as well as active and passive range of motion due to scar adhesions.
- It’s critical to give the scar as much massage as you can and to let the skin separate easily from the tendons underneath.
- Preventing infections starts with the first step.
- Patients may need tenolysis or tendinopathy if severe adhesions are discovered and confirmed.
Loss of sensation
Nerve damage symptoms can appear six weeks after the injury, even in cases when patients have limited nerve damage at the time of injury that does not require surgical repair. These signs consist of:
- In the affected finger, numbness, tingling, or tingling
- Talk to your surgeon about these symptoms and indicators since, if the nerve is damaged beyond conservative treatment, more surgery might be required.
Treatment of Mannerfelt syndrome
Treatment involves:
Medical management:
- Medical treatment for inflamed tenosynovium has been used to lessen discomfort, the creation of caps, and the possibility of tendon rupture.
- If the lesion is found, surgery will be the course of therapy.
Surgical treatment:
- Before the operation, the patient is advised that specific construction techniques might be required and that the underlying condition—in this example, rheumatoid arthritis—will not be treated by the process.
- The patient is also informed that tears and tenosynovitis can return.
- The division of the transverse ligament in rheumatoid arthritis cures an unknown Mannerfelt lesion.
- The bony spur on the carpal tunnel floor is removed after examination, and then a complete flexor tenosynovectomy is performed.
- A great deal of research has been done on carpal tunnel syndrome, and tendon restoration can stop further tears.
- A complete evaluation of the carpal tunnel is advised in patients with a fused interphalangeal joint because a bone spur pressing on the flexor pollicis longus tendon may have an impact on other tendons as well.
- It is advised to reconstruct and repair tendons in interphalangeal joints that are functional.
- When the tendon’s distal end is outside the wrist and cannot be brought back to the injury, a tendon transplant, also known as a graft, is necessary.
- Additionally, a tendon transfer takes place in the flexor pollicis longus muscle, which is not working.
- An osteoarthritic or unstable thumb interphalangeal joint can be treated with tendon fusion.
- In the proximal palm, a linear incision is made across the fourth ray, and it extends in a zigzag fashion over the wrist.
- Steer clear of the cutaneous palmar, motor, and central nerves and their branches.
After removing the bone spur, the surrounding soft tissue is stimulated to cover the exposed bone. The following can cover the damage:
- Silicone covering.
- Transverse palm flap.
- Tendon transplantation.
- Short pons tendon graft.
- Conventional full-length tendon graft.
Tendon transfer
- When the incision is closed, the thumb should be held at 30 degrees of palmar flexion and the wrist at 15-20 degrees.
- A back brace is put on and the detachable suture is taken out after six weeks.
- Tendon transposition happens in the flexor pollicis procumbens tendon, which is not functioning.
- Comparatively speaking, a tendon graft has multiple attachment points.
Tendon transfer has other advantages such as:
- Provides a more practical tendon.
- To transplant the graft, a second surgery is not required.
- In cases of flexor wrist prolapse tendon injury, allows for mobility.
Postoperative tendon healing
Three phases comprise the tendon healing process:
Inflammatory phase
- The initial stage
- endures during the first seven days following surgery.
- This is the stage in which macrophages aid in initiating the healing and remodeling process, while fibroblasts produce type III collagen.
Proliferative phase
- Here’s the next action.
- It continues from the eighth day to roughly three weeks following surgery.
- At this point, a significant amount of degraded collagen is used to mimic the tissue, and angiogenesis also takes place.
Transformational phase
- This is the third stage, which happens about eighteen months following surgery.
- At this point, type I collagen replaces type III collagen due to tensile pressures causing tissue regeneration. This process occurs more linearly and forms a connection, strengthening the tendon.
Management of postoperative physical therapy
- Knowing anatomy, pulleys, tendon damage sites, and the stages of tendon recovery is essential for therapists since it provides insight into the therapy approach.
- The location of tendon damage determines the type of splint that is used and how it is treated.
- The exercises used for rehabilitation depend on the extent and degree of tendon repair.
- After surgery, the tendons are at their weakest, therefore if the patient is sent for treatment 8 or 9 days after surgery and has not yet received treatment, the therapist probably did not want to start vigorous range of motion exercises.
- Therapists need to understand the flexor mechanism’s role in the arm’s functional use as well as how it works. The functioning of the patient may be impacted by tendon injury.
Wound and scar treatment
- Wound care is the first thing that needs to be attended to following surgery.
- A basic silicone dressing (like Mepitel) can be used to cover the postoperative wound.
- Breathable, convenient gauze surrounds the finger.
- Therapists can also use Coban, but an appropriate, comfortable, dry bandage will do just as well.
- Compression bandages are applied to manage edema.
- Scar treatment can start as soon as the wound heals.
- Paper tapes or scars can be covered using silicone gel film.
Scar treatment
- Things like Fixomull. Scar massage can be done during therapy sessions as well as as a preventative measure at home.
Rehabilitation exercises
- Maintaining tendon glide and promoting differential tendon glide regulates early collagen deposition, making it simple to repair the repair shop and preventing adhesions, tent tears, or recurrence to give patients the best possible outcome following surgery. Exercises for rehabilitation are intended to achieve this after flexor tendon restoration.
- Many treatment plans are used for the rehabilitation of flexor tendons. The movement time used in these programs is usually a mix of active and passive.
Post-Operative Training– FPL Repair (first 6 weeks)
- Exercises for passive IP joint flexion
- Thumb compound flexion in a passive position
- Active flexion up to roughly 50% of the patient’s possible active range of motion
- Five times each day, ten reps
Post-operative exercises after 6 weeks
- Splints are worn for six weeks following any surgical repair of a tendon.
- The patient is removed from the splint after the first six weeks to start light functional use, gradually increase it, and evaluate the patient’s fully active and passive range of motion. Approximately eight weeks following surgery, strengthening can normally start.
- Activities that build strength include e.g.
- Dig the Play-Doh, Theraputty, or sponge into the boiling water.
- When complete upper extremity strengthening is required, wrist weights and Therabandin may be used.
- The patient can be discharged home with a home regimen that consists of consistent stretching, scar care, and strengthening exercises once they resume leisure activities, use their arm functionally with few limits, and their pain is under control.
Conclusion
Mannerfelt is credited with coining the term “lesion,” hence the syndrome is known as Mannerfelt syndrome.
Mannerfelt syndrome is caused by a flexuous pollicis longus tendon rupture brought on by a bony spur in the carpal tunnel. Surgery is required for the rare ailment’s treatment. However, diseases such as rheumatoid arthritis cannot be cured by surgery.
FAQs
In rheumatoid arthritis, what kind of tendon rupture occurs more frequently?
Either bone spur wear or direct hypertrophic tenosynovium penetration into the tendon is the cause of flexor tendon tears associated with rheumatoid arthritis.The most frequent cause of tendon rips is in the carpal tunnel, called friction tears.
What is the healing period for flexor tendonitis?
When your arm is strong enough to use without restriction, the flexor tendon needs three to four months to repair. Following surgery, a splint will typically need to be worn for six to eight weeks. It will only be taken off for exercise sessions that your therapist and doctor have recommended.
Can tendons mend on their own?
Tendons are the most self-healing type of connective tissue, while many other elements are also important for tissue repair and healing. An extremely important factor in the healing process is that, in contrast to muscles, tendons often have a fairly inadequate blood flow.
Which vitamin promotes tendon healing?
The importance of vitamin C (VC) in tendon and ligament repair has been linked to its antioxidant properties and its role as a cofactor in the synthesis of collagen.
What lack results in tendinitis?
Vitamin C is essential for the manufacture of new collagen, and its shortage can weaken your tendons and ligaments by preventing this process.
Refernces
- MANNERFELT’S SYNDROME | Hand Surgery Resource. (n.d.). https://www.handsurgeryresource.org/mannerfelt.
- Image-Redirect Notice. (n.d.-m). https://www.google.com/url?sa=i&url=https%3A%2F%2Fwww.handsurgeryresource.org%2Fmannerfelt&psig=AOvVaw2pmxabJ83rQ-8nUeLkELGC&ust=1718082448381000&source=images&cd=vfe&opi=89978449&ved=0CBIQjRxqFwoTCKjksoOi0IYDFQAAAAAdAAAAABAJ.
- Kavya. (2023, February 10). What Is Mannerfelt Syndrome? https://www.icliniq.com/articles/orthopedic-health/mannerfelt-syndrome.
- Thakkar, D. (2023, June 30). Mannerfelt Syndrome – Cause, Symptoms, Treatment – Samarpan. Samarpan Physiotherapy Clinic. https://samarpanphysioclinic.com/mannerfelt-syndrome/



One Comment