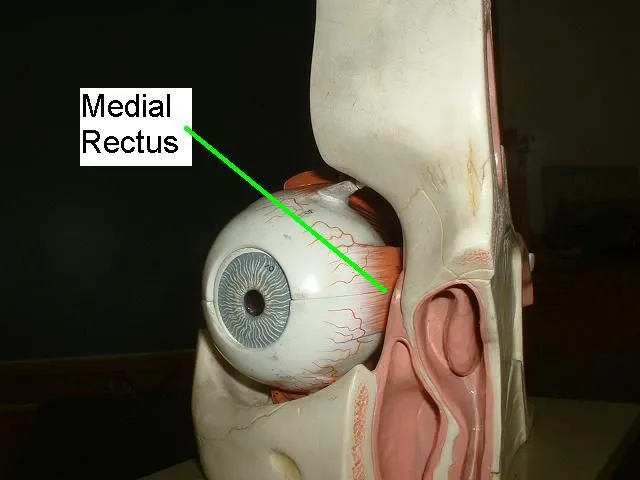
Medial Rectus Muscle
Introduction
The medial rectus muscle is a muscle that is in the orbit near the eye. It is an extraocular muscle of the eye. It arises from the ordinary tendinous ring and inserts into the anteromedial surface of the eye. It is innervated by the inferior division of the oculomotor nerve (III). It rotates the eye medially (adduction).
Origin and Insertion of Medial Rectus Muscle:
The medial rectus muscle is the smallest but strongest of the four recti muscles. It arises from the medial part of the common tendinous ring, which is in between the superior and inferior recti, and the adjacent surface of the dura mater (meninges) that surrounds the optic nerve (CN II).
The muscle courses anteriorly, sliding over the medial part of the eye to overlap its equator and reach the anterior half of the eyeball. It then ends on the eyeball’s medial side, approximately 5 millimeters posterior to the corneoscleral junction. The inserted muscle fibers of the medial rectus pierce the facial sheath of the eyeball (Tenon’s capsule), which in turn reflects back and creates a thin facial sleeve around that muscle’s tendon. This sleeve gives off an expansion called the medial check ligament that makes contact with the medial rectus muscle with the medial wall of the orbit.
Relations:
Medial rectus muscle courses are cushioned in the periorbital fat tissue, superior to the floor of the orbit and inferior (below) to the superior oblique muscle, ophthalmic artery, and nasociliary nerve. The lateral surface of this muscle circles a triangular space between the posteromedial surface of the eye and the optic nerve. The inferior branch of the oculomotor nerve travels this space in order to reach and pierce the lateral surface of the muscle.
Nerve supply:
The medial rectus muscle is innervated/supplied by the inferior division of the oculomotor nerve 3rd Cranial nerve). A branch of it enters the muscle approx about two-fifths of its length. It usually divides into two small branches, occasionally three. These further subdivisions become smaller down the length of the muscle until they become invisible to standard staining around 17 mm from the insertion of the muscle.
Structure:
The medial rectus muscle shares an origin with several other extrinsic eye muscles and the common musculotendinous ring. It ends (inserts) on the anteromedial surface of the eye. This insertion has a width of about 11 mm.
Function of Medial Rectus Muscle:
When contracting the muscle of the eye each medial rectus muscle adducts the eyeball, i.e. pulls the eye medially. This movement is important in two types of ocular movements; conjugate and disconjugate.
Conjugate movements happen when both eyeballs move in the same direction. The medial rectus muscle takes part in conjugate motions of the eye in a horizontal plane (i.e. left and right), working together with the lateral rectus. For guiding the gaze to one side, medial and lateral recti have to function synchronously;
The Ipsilateral (same side) medial rectus relaxes the ipsilateral lateral rectus contracts. This sequence pulls the ipsilateral eye toward the direction wished for.
The contralateral (opposite) medial rectus contracts, contralateral lateral rectus relaxes. This sequence pulls the opposite eye toward the desired direction.
As the lateral rectus is supplied by the abducens nerve (CN VI), the synchrony between these muscles is entrenched by the medial longitudinal fasciculus that connects the oculomotor and abducens nuclei.
Disconjugate motions are when the eyeballs converge or diverge from the midline. When both medial recti muscles contract, they converge the eyeballs toward the midline. Convergence is a part of the accommodation reflex when the eyes adjust to see a close object.
Embryology:
The mesenchyme of the head, including the orbit and its structures, originates primarily from two precursors, mesoderm, and neural crest cells. The extraocular muscles arise from the mesoderm, but the satellite and connective tissue of the muscle originates from neural crest cells. Most of the remaining connective tissue of the orbit also is came from neural crest cells.
Blood Supply and Lymphatics:
The medial rectus receives blood from the inferior muscular branch of the ophthalmic artery. The main blood supply for all of the extraocular muscles is the muscular branches of the ophthalmic artery. The two branches of that are the inferior muscular branch and the superior muscular branch. The larger inferior muscular branch supplies the medial rectus, inferior rectus, and inferior oblique. The superior muscular branch gives branch to the lateral rectus, superior rectus, superior oblique and levator palpebrae superioris. Additionally, the lateral rectus muscle obtains some blood supply from the lacrimal artery.
Venous drainage is similar to the arterial system and empties into the superior orbital vein and inferior orbital vein. Usually, there are a total of four vortex veins, and these veins are found at the lateral and medial sides of the superior and inferior rectus muscles.
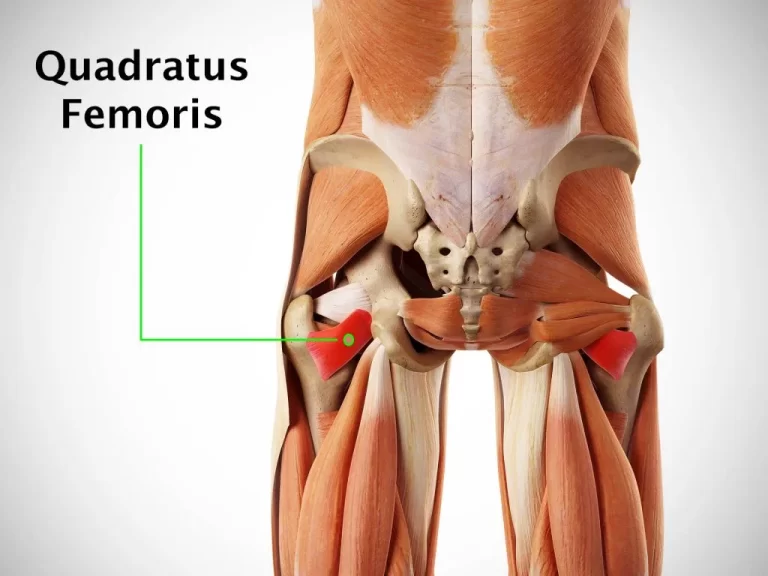
Muscles:
The medial rectus and the lateral rectus muscle make up the horizontal rectus muscles. The superior and inferior rectus muscles together form the vertical rectus muscles. Each of the rectus muscles arises posteriorly at the Annulus of Zinn and courses anteriorly. The medial rectus elongates along the medial orbital wall. Each of the rectus muscles inserts on the globe at different distances from the limbus, and the curved line drawn along the insertion points makes a spiral that is also known as the Spiral of Tillaux. Starting at the medial part of the globe, the medial rectus inserts at 5.5 mm from the limbus, the inferior rectus inserts at 6.5 mm from the limbus, the lateral rectus inserts at about 6.9 mm from the limbus, and the superior rectus at about 7.7 mm from the limbus.
The medial rectus is 10.3 mm in width at its insertion on the globe. The tendon is 3.7 mm, measured from the originating point. The entire length of the muscle is about 40.8 mm.
These muscles and their insertions have anatomical and surgical considerations which will be discussed after.
Extraocular muscles have a huge ratio of nerve fibers to skeletal muscle fibers. The ratio is 1:3 to 1:5, compared to other skeletal muscles which are 1:50 to 1:125. Extraocular muscles are a specialized type of skeletal muscle with a variety of fiber types, including both slow tonic types which resist fatigue, and also saccadic (rapid) type muscle fibers.
Physiologic Variants of Medial Rectus Muscle:
The size of the medial rectus muscle, as well as its insertion point on the globe from the limbus and other anatomical measurements, may vary largely from one individual to the next. The numbers described in this article show average distances.
Congenital differences in the extraocular muscles can cause ocular misalignment. See the Clinical Significance section for more details belonging to strabismus.
Surgical Considerations:
The nerves of the rectus muscles and superior oblique muscles end in the muscles at one-third the distance from the origin to the insertion. This makes injury to these nerves during anterior segment surgery problematic, but not impossible. Additionally, instruments that are advanced 26 mm posterior to the medial rectus muscle insertions can cause injury to this nerve.
Blood vessels may be compromised during operations of the medial rectus muscle. The vessels which give supply blood to the extraocular muscles also closely supply to the temporal half of the anterior segment of the eye. The majority of the nasal half of the anterior segment circulation also comes from blood vessels that supply the extraocular muscles. Therefore, care must be taken during surgery of the medial rectus or other extraocular muscles to avoid lacking this blood supply.
There are fascial layers to consider in the orbit which deal with the medial rectus.
Tenon’s capsule is an elastic connective tissue that gives attachment to the optic nerve posteriorly and is pierced by all of the extraocular muscles except the levator palpebrae superioris. When surgery is done, care must be taken not to compromise Tenon’s capsule 10 mm posterior to the limbus. Otherwise, adipose tissue may prolapse and will cause adhesions which could limit extraocular movement.
There are other complications that may result from medial rectus surgery, which also may result from other rectus muscle surgery. Unsatisfactory alignment is the most common complication and that may need additional surgery to correct this. Refractive changes may happen when two rectus muscles of one eye are operated on, and this might resolve over months. Other possible surgical complications include diplopia and perforation of the sclera, as also postoperative infections. Although uncommon, serious infections might result after strabismus surgery, including pre-septal or orbital cellulitis and endophthalmitis.
Clinical Significance:
The function of the medial rectus muscle can be examined along with the other extraocular muscles during the clinical exam. The movement of the extraocular muscles can be assessed by having the patient watch in nine directions. Starting with the primary gaze, followed by the secondary positions (as up, down, left, and right) and the tertiary positions (as up and right, up and left, down and right, down and left). The clinician can test these positions by having the patient follow the clinician’s finger and trace a huge letter “H” in the air.
Further tests of ocular alignment can be tested further by various methods, including cover tests, corneal light reflexes, dissimilar image tests, and unsimilar target tests. Since many patients with extraocular muscle abnormalities are young children, the clinician may need to employ various clever means such as using toys or other objects to exhibit the cooperation of the child.
Strabismus, or ocular misalignment, can be happened by abnormalities in binocular vision or abnormalities of neuromuscular control. Weakness, injury, or paralysis which involves the medial rectus muscle can be involved in strabismus. Though multiple conditions exist, only a few are shown here.
The prefix “eso” belongs to a condition where the eye is rotated so the cornea deviates nasally and the fovea is rotated temporally. Esotropia belongs to an esodeviation that is constant. Incomitant deviation happens when the abnormality changes with the direction of the gaze or the fixating eye. Therefore, incomitant esotropia is an eye that is deviated nasally and changes depending on gaze or fixation. Medial rectus muscle restriction or compression might cause incomitant esotropia. Some various conditions may cause this such as thyroid myopathy, medial orbital wall fracture, Duane syndrome, or post-surgical excessively resected medial rectus muscle.
Other Issues:
A-pattern and V-pattern deviations are horizontal; rectus muscles can be vertically turned to correct A-pattern and V-pattern deviations. In A-pattern deviations, the medial rectus muscle is turned superiorly along with the globe towards the location of the deviation. In V-pattern deviations, the medial rectus is turned down to the deviation. This makes weakens that muscle in the direction of gaze when the muscle is moved. Full treatment plans for all these disorders depend on the function of all the other extraocular muscles, most notably the superior and inferior obliques, and examination of over or under-action is crucial.
Interesting information related to Medial Rectus Muscle:
The medial rectus muscle is part of a group of skeletal muscles which is also called the extraocular muscles of the eye.
Extraocular muscle disorders, such as extraocular muscle palsy, can cause each person to experience symptoms of visual confusion, vertigo, oscillating or rapid image movement, or double vision. Extraocular muscle palsy is also caused by stroke, or trauma, or can be present at birth. A traumatic event, or genetics, may cause oculomotor nerve injury, causing the eye to move outward and downward with the inability to turn inward or upward.
Trauma to the eye and nose region of the face may cause swelling in or tear to the medial rectus muscle. Common symptoms of this palsy may include double vision, periorbital edema, and limited adduction or abduction of the eye. In many cases, NSAIDs, such as ibuprofen, will treat and exclude the issues that occur with medial rectus injuries, but in serious cases, surgery may be required.
Related pathology:
Oculomotor nerve palsy :
Oculomotor nerve palsies, or third nerve palsies, results in the weakness of muscles innervated by the oculomotor nerve, which are namely the superior rectus, inferior rectus, medial rectus, inferior oblique, and levator palpebrae superioris muscles.
Terminology
If the pupil is normal-sized and also is reactive to light, it is called a pupil-sparing third nerve palsy; conversely, if the pupil is enlarged and non-reactive, then it is called a non-pupil-sparing third nerve palsy.
Classically, patients present with diplopia and physical exam findings on the same side of the oculomotor nerve (CN III) lesion:
“down and out” ocular alignment
abduction, slight depression, and also intorsion (due to paralysis of adduction, elevation, and depression)
complete ptosis
It is due to neuropathy affecting levator palpebrae superioris
+/- enlarged unreactive pupil
if present, suggests compression of CN III because the parasympathetic pupillary fibers are located on the peripherally of the nerve and are more likely to get affected by external compression.
Treatment and prognosis
In post-traumatic oculomotor nerve palsy, gaze movement training and steroid injections might be helpful.
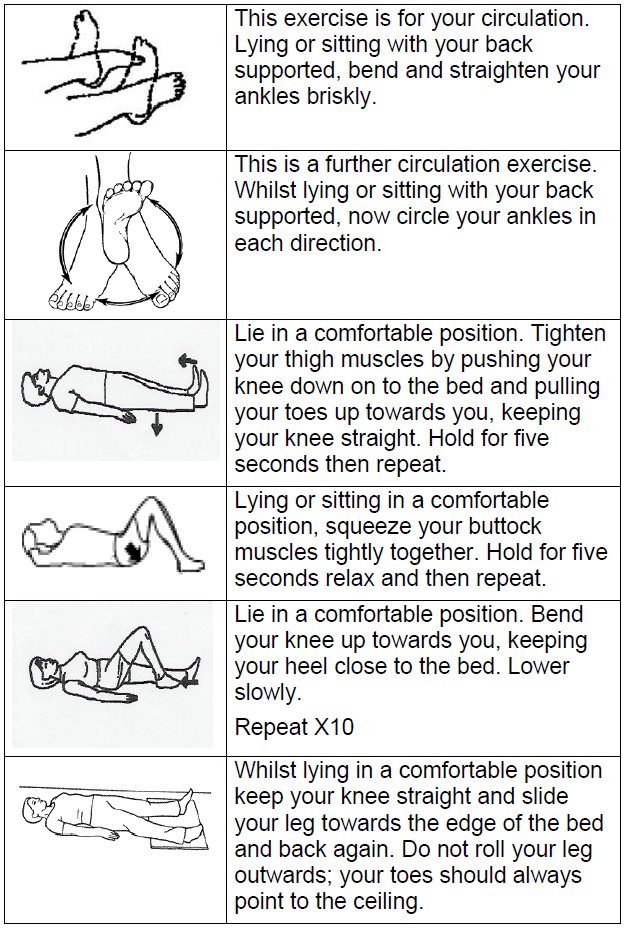
Medial Rectus Muscle exercises :
Eye circles
Keep your eyes open and rotate your eyes in a clockwise direction. If this movement is uncomfortable, then close your eyes to do this exercise. Circle your eyes around fifteen to twenty times. Repeat this circling in the counter-clockwise direction. Repeat this exercise around three times a day.
Eye contractions
Begin this exercise by closing the eyes as tight as possible and holding or staying in that position for four seconds. Now open your eyes and blink as quickly as possible fifteen times. Repeat these exercises around five times a day.
FAQs
What happens if the medial rectus is damaged?
Injury to the eye and the nose area of the face may cause swelling or a tear to the medial rectus. The most common symptoms may include double vision, periorbital edema, limited adduction or abduction of the eye
What is the function of the medial rectus?
The medial rectus is an adductor muscle, and functions along with the lateral rectus which does abduction of the eye. These two muscles allow the eyes side-to-side movements. With the head watching straight and the eyes watching straight ahead, the eyes are said to be in primary gaze.
What are the treatment options for medial rectus recession?
Common treatment generally includes weakening the medial rectus muscle to allow the eye to reach a normal position. Jampolsky suggested that the medial rectus recession of both eyes was important to correct the condition.
How can you distinguish between the medial and lateral rectus?
The medial rectus, or nose-side, muscles turn the eyes inwardly; when functioning simultaneously, they converge, or overlap, the eyes. The lateral rectus, or temple-side, muscles turn the eyes outwardly; when they perform simultaneously, they diverge or splay apart, the eyes.
How long does it take the rectus muscle to heal?
The important healing time for a muscle tear is approximately 3–6 weeks for total recovery, but it is dependent on the extent of the lesion.
Why Medial Rectus is called the Muscle of Marriage?
The medial rectus muscle is humorously referred to as the “muscle of marriage” because it is responsible for adduction, which is the movement of the eye towards the nose. This action is crucial for maintaining proper eye alignment and ensuring that both eyes are looking at the same point, a concept similar to how a successful marriage requires both partners to be aligned and focused on the same goals. This term is often used in a light-hearted, metaphorical way in anatomy and physiology discussions.



3 Comments