Seizures
What are Seizures?
A seizure is a medical situation where you have a temporary, unstoppable surge of electrical activity in your brain. When that occurs, the involved brain cells uncontrollably fire signals to others near them. This type of electrical activity overloads the involved regions of your brain.
That overload can generate a broad range of symptoms or outcomes. The feasible symptoms contain abnormal sensations, passing out, and uncontrolled muscle motions. Treatment choices, depending on seizure variety, contain drugs, surgeries, and certain diet modifications.
The phrase seizure arrives from the antique view in multiple cultures that seizures were a sign of possession by a bad spirit or demon. Yet, the modern drug has exposed the truth: Everyone can have seizures, and some people can have them more effortlessly than further people.
Epidemiology
About 81% of patients will feel an epileptic seizure during their lifetime. In grown-ups, the risk of a seizure repeating within the five years following a new-onset attack is 35%, and the risk increases to 75% in a patient who has had a second seizure. In kids, the risk of a seizure repeating within the five years following a single unprovoked seizure is approximately 50%, and the risk increases to approximately 80% after two unprovoked seizures. In the United States in 2011, seizures resulted in a calculated 1.6 million emergency department visits, about 400,000 of these visits were for new-onset seizures. The precise incidence of epileptic seizures in low-income and middle-income countries is unfamiliar, yet, it likely exceeds that in high-income nations. This may be due to raised risks of birth injuries, traffic accidents, malaria, and further parasitic infections
What is the difference between seizures and epilepsy?
Understanding the difference between seizures and epilepsy begins with knowing seizures fall into two main classes relying on why they occur.
Provoked seizures: These occur because of further situations or events (alcohol or medication withdrawal, high fevers, low blood sugar). Provoked seizures make up approximately 25% to 30% of all seizures.
Unprovoked seizures: These aren’t symptoms of a recent medical disease or circumstance and happen when a patient’s brain can more efficiently create spontaneous seizures. This also contains seizures that occur more than seven days after a precise cause (such as head damage or stroke).
Epilepsy is a brain disease that places you at risk of having random, unprovoked seizures. Healthcare providers or doctors analyze it when you have at least two unprovoked seizures, or you have a single unprovoked seizure and have an elevated risk of having at least one more in the subsequent 10 years. Owning a single unprovoked seizure raises the odds of owning another. Provoked seizures aren’t adequate for a provider or doctor to analyze you with epilepsy.
Seizure Phases
Seizures bring on many various forms and have a start (prodrome and aura), middle (ictal), and end (post-ictal) phase. These stages are explained beneath.
The three seizure stages are described as:
Beginning phase ( Prodrome stage )
During the prodromal phase, some patients can tell when a seizure is on its path. They may see some early symptoms hours or even days before the seizure begins. Not all patients feel this phase. Some typical signs can contain:
- Mood changes
- Anxiety
- Feeling lightheaded
- Problem in sleeping
- A problem in staying focused
- Behavior changes.
- Aura
Auras are typically considered an early portion of the seizure. Symptoms of an aura may contain:
- Dj vu (a sense that something has occurred before when in reality it hasn’t)
- Jamais vu (a sense that you’re noticing something you know nicely for the first time)
- Odd smells, sounds, or tastes
- Dizziness
- Vision problems
- Numbness or pins and needles in regions of the body
- Nausea
- Headache
- Panic
- Feelings of intense fear
Occasionally a patient may have an aura that doesn’t progress to evolve into a more extreme or prolonged seizure. Some patient doesn’t feel an aura at all, and their seizure has no early warning signs.
Middle (ictal) phase
The middle (ictal) phase of a seizure is known as the ictal stage. It’s the moment from the first sign to the end of the seizure activity. It is during this time that intense electrical action is happening in the brain. Some typical signs of this stage contain:
- Loss of awareness
- Memory lapse
- Feeling confused
- Difficulty hearing
- Odd smells, sounds, or tastes
- A problem in speaking or saying strange words
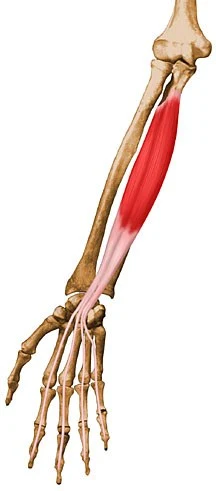
- Twitching
- Loss of muscle control
- Repeated motions (like as lip smacking or chewing)
- Body convulsions
- Racing heart
- Trouble breathing
Ending (post-ictal) phase
The final post-ictal phase happens after the active (ictal) portion of the seizure. This is the recovery phase and during this stage, any physical after-effects of the seizure are felt. The kind of seizure and the portion of the brain affected will specify how long it carries for a patient to return to their normal self.
Some typical signs of this stage contain:
- Confusion
- Lack of consciousness
- Tiredness (fatigue)
- Exhaustion
- Headache
- Loss of bladder or bowel control
- Fear and anxiety
- Frustration
- Shame or embarrassment
- Thirst
- Nausea
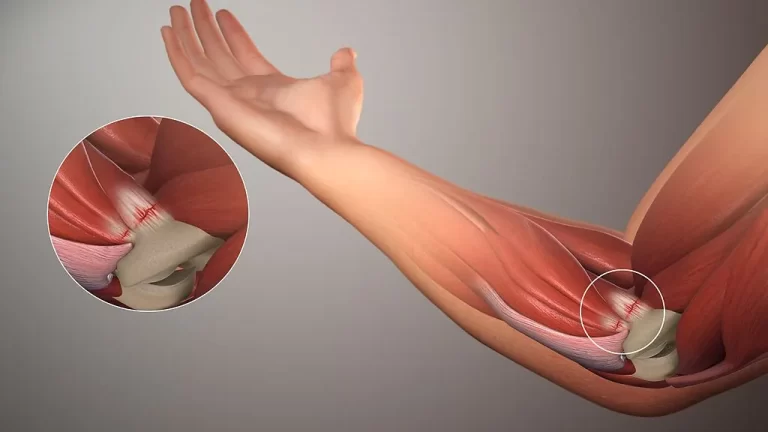
- Sore muscles
- Weakness in regions of the body
- Injury (cuts, head, broken bones)
Once the seizure is over, some patients may recall having one, recall regions of it, or not recognize it at all.
Types of Seizures
Focal seizures
Focal seizures outcome from abnormal electrical activity in one region of your brain. Focal seizures can be done with or without loss of consciousness:
Focal seizures with impaired awareness. These seizures affect an alteration or loss of consciousness or awareness that senses like being in a dream. You may appear awake, but you gaze into space and do not react normally to your atmosphere or you conduct repetitive motions. These may contain mouth motions, hand rubbing, recounting specific words, or walking in loops. You may not recognize the seizure or even know that it happened.
Focal seizures without loss of consciousness. These seizures may change emotions or alter the way things smell, look, taste, feel, or sound, but you don’t fail consciousness. You may suddenly sense joy, anger, or sadness. Some patients have nausea or unusual emotions that are hard to explain. These seizures may also result in problems in speaking, involuntary jerking of a body region, like an arm or a leg, and spontaneous sensory symptoms like dizziness, tingling and noticing flashing lights.
Symptoms of focal seizures may be confused with further neurological diseases, like narcolepsy, migraine, or mental illness.
Generalized seizures
Seizures that seem to affect all regions of the brain are known as generalized seizures. Various kinds of generalized seizures contain:
Absence seizures. Absence seizures, previously called petit mal seizures, frequently happen in kids and are indicated by staring into space or by subtle body motions, like eye blinking or lip smacking. They generally stay for five to 10 seconds but may occur up to hundreds of times per day. These seizures may appear in clusters and generate a brief loss of attention.
Tonic seizures. Tonic seizures induce stiffening of your muscles. These seizures generally involve muscles in your arms, back, and legs and may induce you to lose consciousness and fall to the bottom.
Atonic seizures. Atonic seizures also called drop seizures, generate a loss of muscle control, which may induce you to suddenly collapse, fall or lower your head.
Clonic seizures. Clonic seizures are associated with reprised or rhythmic, jerking muscle motions. These seizures generally involve the face, neck, and arms on both sides of the body.
Myoclonic seizures. Myoclonic seizures generally seem like sudden brief jerks or cramps of your arms and legs. There is seldom no loss of consciousness.
Tonic-clonic seizures. Tonic-clonic seizures, earlier called grand mal seizures, are the most dramatic kind of epileptic seizure and can generate a short loss of consciousness, body stiffening and shaking, and occasionally loss of bladder management or biting your tongue. They may stay for several minutes.
Symptoms of Seizures
With a seizure, signs, and symptoms can vary from mild to severe and differ depending on the variety of seizures. Seizure signs and symptoms may contain:
Occasionally symptoms happen before the seizure carries place. These can contain:
- a sudden feeling of fear or anxiousness
- a feeling of being ill in your stomach
- dizziness
- a change in vision
- a jerky motion of the arms and legs that may generate you to drop items
- an out-of-body sensation
- a headache
- deja vu
Signs that suggest a seizure is in progress contain:
- losing consciousness, observed by confusion
- having uncontrollable muscle spasms
- drooling or frothing at the mouth
- falling
- having a weird taste in your mouth
- clenching your teeth
- biting your tongue
- having sudden, rapid eye motions
- making unusual noises, like as grunting
- losing control of the bladder or bowel role
- having sudden mood alter
Generalized seizures
The main varieties of generalized seizures are:
Tonic-clonic seizures.
Absence seizures.
Tonic-clonic seizures
Formerly called grand mal seizures (French for great illness), tonic-clonic seizures are generally the most recognizable. They occur in the following stages:
Tonic (generally 10 – 30 seconds): During this stage, you pass out as all your muscles taut up. Falls and damages are typical.
Clonic (generally 30 60 seconds, but occasionally longer): This stage includes uncontrolled convulsions (muscle motions).
Post-seizure recovery (up to 30 minutes): During this stage, you wake up and return to how you were before the seizure. Confusion and muscle pains are typical.
Absence seizures
Formerly called petit mal (French for little illness) seizures, these are most familiar in kids. Absence seizures frequently look like spacing out, daydreaming, or staring off into the length (a thousand-yard stare). These seizures end fast with no healing period required.
Absence seizures are short-lived but you can have dozens or even hundreds of duration in a day. They’re effortlessly mistaken for distraction or a sign of an understanding disability.
Other types of generalized seizures
Generalized seizures can occur in different ways that have similarities to that overhead:
Tonic seizures. Like a tonic-clonic seizure, but there’s no clonic stage. Patients pass out during these and tense up but don’t have convulsions.
Clonic seizures. Also, like a tonic-clonic seizure, but there’s no tonic stage. During these, patients pass out and go directly into convulsions without their muscles tightening up.
Atonic seizures. These are also called drop episodes. During an atonic seizure, someones lose control of muscles in their body, generating them to drop to the bottom suddenly. There’s an increased risk of damage from falling during these. This type of seizure is most familiar with Lennox-Gastaut syndrome, an extreme form of youth epilepsy.
Myoclonic seizures. These include a sharp jerk or twitch that involves one muscle or a bunch of connected muscles. When it involves your leg while standings, it can generate you to fall. (NOTE: While these are equal to a myoclonic jerk, which is a sudden muscle cramp as you’re falling asleep, they aren’t the exact thing. Myoclonic jerks that occur as you fall asleep are normal and aren’t a symptom of seizures or epilepsy.)
Focal seizures
Focal seizures involve a smaller region of your brain and remain in one hemisphere. These are also called partial seizures, and auras when they happen come before these. Symptoms like as uncontrolled muscle motions may spread to various locations on one side of your body, like from one side of your face to the hand or foot on the exact side.
Focal seizures contain the next subtypes:
Simple focal seizures. Occasionally called simple partial seizures, you’re conscious of these when they occur. With this type of seizure, the aura is the seizure itself and not only a warning signal.
Complex focal seizures. These are occasionally called complex partial seizures. These disrupt your awareness of what’s occurring to or near you.
Auras as warning signs
When a focal seizure circulates to the further side of your brain, it can shift into a generalized tonic-clonic seizure. If you’ve had a seizure in history, or you understand you have epilepsy, you should manage an aura like a warning sign. To save yourself, you can do the next:
Create yourself as safe as possible. Sit or lie down so you don’t drop and damage yourself. You should also quit what you’re doing if it’s something like driving or using weighty machinery or devices.
Contact somebody you trust to assist you. Inform them where you are and how to see you.
If you can communicate with somebody you know, tell somebody in your immediate surroundings who is in a situation of responsibility or power that you believe you’re close to having a seizure. An instance of this is describing a teacher or a store employee, a police officer, or a security guard.
Causes of Seizures
Nerve cells (neurons) in the brain form, send and accept electrical stimulations, which permit the brain’s nerve cells to express. Anything that disrupts these transmission tracks can lead to a seizure. Some kinds of seizure diseases may be induced by genetic mutations.
Seizures can occur for many various reasons. These contain:
Aneurysms.
Brain tumors (involving cancer).
Cerebral hypoxia (lack of oxygen).
Extreme concussion and traumatic brain injury.
Degenerative brain conditions such as Alzheimers condition or frontotemporal dementia.
Medicines and alcohol (this contains prescription drugs, recreational medications, and even caffeine).
Medication or alcohol withdrawal.
Eclampsia (a state where high blood pressure can induce seizures in a pregnant person).
Electrolyte issues, particularly low sodium (hyponatremia), calcium, or magnesium.
Fevers, particularly high ones (read more about febrile seizures, involving what to do for a loved one or kid who has one, they’re very familiar in kids, and having these barely raises the risk of having seizures or epilepsy later in life).
Sensitivity to flashing or flickering light.
Genetic conditions (situations you have at birth that you inherited from one or both parents).
Hormone-related changes. For instance, catamenial epilepsy can involve a person with a menstrual cycle, causing seizures to occur more frequently at certain issues in the cycle.
Infections (particularly encephalitis or meningitis). Infections can occur because of bacteria, viruses, parasites, or fungi.
Inflammation from autoimmune diseases (where your immune system harms your brain).
Metabolic issues, particularly high blood sugar (hyperglycemia) or low blood sugar (hypoglycemia).
Mental health issues (called psychogenic seizures) such as conversion conditions.
Issues with your brain structure (particularly ones you’ve had since birth).
Sepsis.
Strokes or transient ischemic attacks (TIAs).
Toxins and poisons (like carbon monoxide poisoning or serious metal poisoning).
What are the types of seizures that affect children?
Kids can have seizures for any of the above causes. Fevers are one of the most familiar reasons for youth seizures. Further causes contain:
Juvenile myoclonic epilepsy. This disease generally begins in the mid-teenage years. The main symptom of this kind of epilepsy is having one or more myoclonic seizures on both sides. These generally occur after waking up in the morning and are more probable to lack of sleep. Tonic-clonic and absence seizures are also feasible.
Lennox-Gastaut syndrome. This extreme form of youth epilepsy induces multiple kinds of seizures and brain harm. Developmental delays are also familiar. It has an elevated injury risk because it generally generates atonic seizures (“drop attacks”).
What are the effects of seizures?
Living with epilepsy and feeling recounted seizures can have both short- and long-term outcomes. These can vary from a drop in quality of life to raised risks of mental health diseases.
Short-term effects
Some seizures can induce you to lose complete control of your body. This can guide to falls and other motions that can result in damage.
Patients with epilepsy generally have more physical problems, like bruising and fractures, than a patient without the disease.
Being prone to seizures may also involve your grade of life. For instance, you may no longer be capable to drive. You may like to avoid problems where a seizure could generate severe damage, like swimming or traveling alone.
It’s essential to wear a medical tag bracelet that suggests to emergency responders that you have epilepsy.
Long-term effects
If you don’t get therapy for seizures, their symptoms can evolve more harmful and progressively last longer. Lengthy seizures can guide to coma or death.
While death as a natural result of seizures is irregular, the risk of premature death in a patient with epilepsy is up to three times higher than in all-around people.
Living with epilepsy and seizures can even affect your mental fitness. Patients with epilepsy have a more elevated rate of bipolar disease and depression than a patient without the disease.
Differential Diagnosis
Spells comparing seizures stem from many other processes. One essential differentiation is between a syncopal occasion and a seizure. Both circumstances have an abrupt start, but a syncopal event frequently has a provocative reason, the loss of consciousness is fast, and the return to complete consciousness is fast without a confusional condition. Incontinence may be current with either kind of event. At moments syncope is associated with motor motions mimicking a seizure.
Another distinction frequently affects distinguishing seizures from psychogenic nonepileptic seizures. Please notice that branch for further data.
A partial seizure mimics next:
- Syncope, convulsive syncope
- Psychogenic nonepileptic seizures
- Convulsive concussion
- Movement disorders
- Sleep-related movements
- Convulsive concussion
Diagnosis
History
Persons who have had a seizure should be questioned regarding unique sensations, offering an aura and thus a seizure, and almost typical seizure presentations. Persons generally do not recall generalized-onset outbreaks, so a report of the outbreak itself must be received from witnesses.
Representations of different diseases, like sudden global brain ischemia (for eg, due to ventricular arrhythmia), can reach those of a seizure, involving loss of consciousness and some myoclonic jerks.
A record should contain information regarding the first and any next seizures (for eg, frequency, duration, sequential evolution, the longest and shortest gap between aura, seizures, postictal state, and precipitating factors). All persons should be questioned regarding risk factors for seizures:
- Previous head trauma or CNS infection
- Known neurologic conditions
- Medication use or withdrawal, especially from recreational medicines
- Alcohol withdrawal
- Nonadherence to antiseizure medications
- Family record of seizures or neurologic diseases
Persons should also be questioned about rare triggers (for eg, flashing lights, repetitive sounds, video games, touching specific regions of the body) and regarding sleep deprivation, which can reduce the seizure threshold.
Physical examination
In persons who have a bitten tongue, failed consciousness, incontinence (for eg, urine or feces in clothing), or extended confusion after the loss of consciousness means seizure.
In pseudoseizures, generalized muscular movement and lack of reaction to verbal stimulations may at first glance indicate generalized tonic-clonic seizures. Yet, pseudoseizures can generally be determined from true seizures by clinical features:
Pseudoseizures frequently last longer (a few minutes or more).
Postictal confusion plants to be absent.
Familiar tonic phase movement, observed by the clonic stage, generally does not happen.
The progression of muscular action does not conform to true seizure ways (for eg, pseudoseizure motions may contain jerks moving from one side to the different and back and activated pelvic thrusting).
Intensity may wax and wane.
Vital signs, involving temperature, generally stay normal.
Persons frequently actively resist passive eye-opening.
Physical study rarely shows the reason when seizures are idiopathic but may supply hints when seizures are symptomatic
Lab test
EEG brain activity
EEG brain activity
High-density EEG
CT scan
Pinpointing seizure location
After a seizure, your doctor or physician will review your symptoms and medical record. Your doctor or physician may request several examinations to define the reason for your seizure and estimate how probable it is that you’ll have another one.
Tests may contain:
A neurological exam. Your doctor or physician may estimate your behavior, motor capabilities, and mental function to decide if you have an issue with your brain and nervous system.
Blood tests. Your doctor or physician may bring a blood specimen to study your blood sugar levels and examine for signs of infections, genetic diseases, or electrolyte imbalances.
Lumbar puncture. If your doctor or physician doubts an infection is the reason for a seizure, you may require to have a specimen of cerebrospinal fluid dismissed for testing.
An electroencephalogram (EEG). In this examination, doctors or physicians connect electrodes to your scalp with a paste-like essence. The electrodes register the electrical activity of your brain, which displays as wavy stripes on an EEG recording. The EEG may indicate a way that tells doctors or physicians whether a seizure is probable to happen again. EEG testing may also assist your doctor or physician exclude further situations that simulate epilepsy as a cause for your seizure. Relying on the details of your seizures, this examination may be accomplished at an outpatient visit in the clinic, overnight at a house with an ambulatory instrument, or over a rare night in the hospital.
Imaging tests may contain:
Magnetic resonance imaging (MRI). An MRI scan utilizes powerful magnets and radio waves to produce a precise picture of your brain. Your doctor or physician may be capable to notice lesions or abnormalities in your brain that could guide to seizures.
Computerized tomography (CT). A CT scan utilizes X-rays to bring cross-sectional pictures of your brain. CT scans can show irregularities in your brain that might induce a seizure, like bleeding, tumors, and cysts.
Positron emission tomography (PET). A PET scan utilizes a small quantity of low-dose radioactive textile that’s injected into a vein to assist imagine active regions of the brain and see abnormalities.
Single-photon emission computerized tomography (SPECT). A SPECT examination uses a small quantity of low-dose radioactive material that’s injected into a vein to make a precise, 3D map of the blood flow activity in your brain that occurs during a seizure. Doctors or physicians may also perform a type of SPECT test known as subtraction ictal SPECT coregistered with MRI (SISCOM), which may deliver even more-precise outcomes. This examination is generally done in a hospital with overnight EEG recording
Treatment of Seizures
Device placement in vagus nerve stimulation
Vagus nerve stimulation
Not everyone who has one seizure will have another one, and because a seizure can be an isolated happening, your doctor or physician may not choose to begin therapy until you’ve had more than one.
The optimal plan in seizure therapy is to discover the best feasible treatment to stop seizures, with the fewest side outcomes.
Medication
Therapy for seizures frequently includes the use of anti-seizure drugs. There are many various choices for an anti-seizure drug. One of the more recent drugs authorized by the Food and Drug Administration, cannabidiol (Epidiolex), emanated from marijuana. It’s agreed to manage individual seizures in kids aged 2 and older.
The purpose of a drug is to find the drug that functions best for you and that generates the fewest side outcomes. In some patients, your doctor or physician might suggest more than one drug.
Seeing the right drug and dosage can be difficult. You may require to attempt several various drugs to see which best holds your seizures with the fewest side results. Side effects may contain dizziness, weight gain, fatigue, and mood shifts. More-serious side results can induce harm to the liver or bone marrow.
Your doctor or physician will evaluate your situation, your frequency of seizures, your age, and further factors when deciding which drug to define. Your doctor or physician will also check any other drugs you may be assuming, to confirm that the anti-epileptic drugs won’t interact with them.
Dietary therapy
Following a diet that’s elevated in fat and very low in carbohydrates, called a ketogenic diet, can enhance seizure control. The ketogenic diet is very tough and can be Harding to pursue, as there is a restricted range of foods permitted. Variations on a high-fat, low-carbohydrate diet, like the low glycemic index and modified Atkins diets, though less useful, aren’t as restrictive as the ketogenic diet and may deliver advantages. These altered diets are still being analyzed.
Surgery
If different therapies aren’t useful, surgery may be a choice. Surgery plans to prevent seizures from occurring. Surgery functions best for a patient who has seizures that always arise in the same location in the brain. There are several kinds of surgery, involving:
Lobectomy (laminectomy). Surgeons or doctors find and remove the location of your brain where seizures start.
Multiple subpial transections. This kind of surgery includes making several cuts in regions of the brain to control seizures. It’s generally done when the region of the brain where seizures begin can’t be safely extracted.
Corpus callosotomy. This surgery cuts the network of relations between the neurons of the right and left halves of the brain. This is utilized to manage seizures that begin in one half of the brain and journey to the further half. Yet, even after surgery, seizures may still happen on the side of the brain where they began.
Hemispherectomy (hemispherectomy). This surgery extracts half of the outermost layer of the brain. This is an intense kind of surgery that is only used when drugs aren’t useful in controlling seizures and seizures involve only half of the brain. Many daily functional capabilities may be lost after this surgery, but kids can frequently heal those capabilities with effective rehabilitation.
Thermal ablation (laser interstitial thermal therapy). This small invasive surgical approach focuses highly concentrated energy at a precise mark in the brain where seizures start and destroy the brain cells that induce seizures.
Electrical stimulation
Other processes that may offer seizure relief contain:
Vagus nerve stimulation. A machine implanted beneath the skin of your chest facilitates the vagus nerve in your neck, transmitting signs to your brain that inhibit seizures. With vagus nerve stimulation, you may still require to bring drugs, but you may be capable to reduce the dose.
Responsive neurostimulation. During responsive neurostimulation, a machine planted on the cover of your brain or within brain tissue can notice seizure activity and provide electrical stimulation to the detected region to prevent the seizure.
Deep brain stimulation. Doctors or physicians implant electrodes within specific regions of your brain to create electrical impulses that control abnormal brain activity. The electrodes connect to a pacemaker-like machine put under the skin of your chest, which holds the quantity of stimulation delivered.
Physiotherapy treatment
Activity can reduce the possibility of a seizure.
Activity is a great method to lower stress.
Decreasing stress can reduce the possibility of having a seizure.
If you have seizures, you can still do activity and remain secure.
Activity with a patient who knows about your seizures.
Make sure your activity members understand what to do if you have a seizure.
Wear a bracelet or necklace with details regarding your seizures.
Exercise in a safe location.
Make sure that there is an asset nearby if you carry a seizure.
Exercise on soft textures such as grass or mats.
Wear knee and elbow protectors.
Be careful while swimming.
Never swim independently.
Go with suitable swimmers who can assist you if you have a seizure.
Ever wear a life vest
Inform a lifeguard regarding your seizures.
Be careful while playing sports.
If you play sports such as football or hockey, wear a helmet.
Be careful while biking, hiking, or running.
Remain out from busy roads and difficult trails.
Wear a helmet, elbow protectors, and knee protectors.
Let the different patients know where you are going.
Even though exercise is good, it can start a seizure.
Don’t get exhausted – assume breaks frequently
Don’t activity when it’s extremely hot.
Don’t reach overheated.
Consume lots of water.
Get a quantity of sleep.
Eat nutritious foods.
Physical activity enhances energy, fitness, and mood and even reduces stress. Enhancing overall fitness and well-being in this route can assist to decrease seizures.
It can also assist the patient feel more in control of their health.
It also assists the release of feel-good hormones into the brain, supports muscles active, decreases fat levels in the body, and raises oxygen flow to the brain.
It can also raise bone density.
Research indicated that routine sessions of aerobic activity (for instance walking, running, cycling swimming) for 60 minutes, twice a week, for 15 weeks can result in a considerable decrease in the number of seizures they had.
Consume water, light fruit juice, or squash while exercising to assist substitute the fluids and body. Do not do activities directly after a meal.
Team sports or group activities like walking or gardening groups can even be a fine course for improving self-confidence.
Making new friends may assist with any emotions of isolation.
Most sports, involving contact sports such as hockey, football, basketball, and rugby, have not been displayed to raise the possibility of a person having a seizure, but contact sports arrive with a raised risk of head injuries, which could involve a patient with a record of epilepsy. Defensive sports headgear assists to decrease this risk.
Pregnancy and seizures
Females who’ve had prior seizures generally can have fit pregnancies. Birth deficiencies connected to specific drugs can occasionally happen.
In special, valproic acid one possible drug for generalized seizures has been associated with cognitive deficiencies and neural tube defects, like spina bifida. The American Academy of Neurology suggests that females avoid using valproic acid during pregnancy because of the dangers to their babies. Concern these risks with your doctor or physician. Because of the hazard of birth defects and because pregnancy can change drug levels, preconception planning is especially essential for females who’ve had seizures.
In some possibilities, it may be suitable to alter the dose of the seizure drug before or during pregnancy. Females should function closely with their doctors or physician before evolving pregnant to be on the lowest required dose of the safest seizure drug that is useful for seizure management.
Contraception and anti-seizure medications
Some anti-seizure drugs can change the significance of birth management (oral contraceptive) drugs. If contraception is an elevated focus, check with your doctor or physician to assess whether your drug interacts with your oral contraceptive and if different states of contraception require to be evaluated.
Lifestyle and home remedies
Here are some actions you can bring to assist with seizure management:
Take medication correctly. Don’t change the dosage before speaking to your doctor or physician. If you sense that your drug should be altered, consult it with your doctor or physician.
Get enough sleep. Lack of sleep can activate seizures. Be certain to get sufficient rest every night.
Wear a medical alert bracelet. This will assist emergency personnel know how to manage you perfectly if you have another seizure.
Be active. Exercising and being busy may assist to hold you physically healthy and ease the sadness. Make sure to drink sufficient water and rest if you obtain tired during the activity.
Make healthy life choices. Managing stress, restricting alcoholic drinks, and avoiding cigarettes are all elements of a fit lifestyle.
Personal safety
Seizures don’t generally result in severe injury, but if you have recurrent seizures, the damage is a chance. These measures can assist you to avoid damage during a seizure:
Take care near the water. Don’t swim independently or calm in a boat without somebody nearby.
Wear a helmet for safety during exercises like bike riding or sports participation.
Carry showers rather than baths, unless somebody is around you.
Modify your furnishings. Pad harsh corners, buy furniture with spherical edges, and select chairs that have arms to hold you from falling off of them. View carpet with dense padding to save you if you do fall.
Display seizure first-aid information in a location where the crowd can easily notice them. Contain any essential phone numbers there, too.
What should I do if someone with me has a seizure?
If you’re with somebody who’s having a seizure, there are several items you can do as a component of seizure first aid. Some Dos and Donts contain:
Dos
Make certain they can breathe. Reduce any clothing near the patient’s neck to make certain they’re breathing.
Move hazardous things out of them. This contains breakable things that might fall and damage them. If they wear glasses, carefully bring the glasses off and shift them out of reach.
Place them in the saving position. Bend the person on their side. This position assists to save a patient’s capability to breathe and maintains them from inhaling any fluid such as saliva or vomit.
Attempt to time the seizure as best you can. Informing a healthcare provider or doctor how long the seizure survived can be critical data. It can also assist you to know if you require to contact for emergency medical assistance.
Stay with them as they come out of the seizure and rescue. A patient who has a seizure frequently feels dizzy or scared as they wake up and return to regular. Asset reassures and relaxes them.
Make sure they’re fine once they wake up. If they have any damages after the seizure, study if they require medical supervision. If the patient hit their head or there’s a risk of damage to their neck, head, or back, the securest item to do is to get medical supervision and create sure there aren’t any severe damages that you can’t see.
Contact for assistance if the patient has status epilepticus. Call 911 (or your local trouble services digit) if the seizure stays more than five minutes or the patient has another seizure before healing from the first. Status epilepticus is a life-threatening medical trouble. You should also contact emergency assistance if they don’t begin to recover or are unresponsive for more than 10 to 15 minutes after the convulsions quit. That may be a sign of a seizure persisting in their brain actually though their body isn’t shaking any longer.
Dont
Don’t restrain them. You could damage the patient or get harmed yourself.
Don’t place anything in their mouth. There are many myths regarding seizures and epilepsy. One myth is that placing something in a patient’s mouth such as a belt or spoon can maintain them from swallowing or biting their tongue. Don’t accomplish this. You shouldn’t place anything into the mouth of somebody having a seizure. You could damage them or get harmed yourself.
Don’t panic. Stay quiet. If others near you are panicking, comfort them as nicely as you can. About 98% of seizures don’t stay more than five minutes.
Coping and support
If you’re living with a seizure disease, you may sense anxiety or worry regarding what your destiny holds. Anxiety can involve your mental fitness, so it’s essential to speak with your healthcare professional or doctor regarding your feelings and pursue ways you can find an asset.
At home
Your family partners can deliver much-required help. Inform them what you know regarding your seizure disease. Let them understand they can ask you queries, and be open to conversations regarding their concerns. Assist them to understand your situation by transmitting any educational materials or further resources that your health care specialist has provided you.
At work
Meet with your supervisor and speak regarding your seizure disease and how it impacts you. Discuss what you require from your supervisor or co-workers if a seizure occurs while at your job. Think conversing with your co-workers regarding seizure diseases you can broaden your help system and obtain acceptance and understanding.
You’re not alone
Recall, you don’t have to do it independently. Come out to family and friends. Request your health care professional or doctor regarding local support groups or join an online asset community. Don’t be scared to request assistance. Having a healthy asset system is essential to living in any medical situation.
Complications
Having a seizure can occasionally lead to events that are risky for you or others. You might be in danger of:
Falling. If you drop during a seizure, you can damage your head or break a bone.
Drowning. If you keep a seizure while swimming or bathing, you’re in danger of unexpected drowning.
Car accidents. A seizure that induces loss of either awareness or power can be difficult if you’re driving a car or operating other tools.
Pregnancy complications. Seizures during pregnancy pose risks to both mother and baby, and specific anti-epileptic drugs raise the risk of birth defects. If you have epilepsy and prepare to evolve pregnant, perform with your doctor or physician so that he or she can change your drugs and observe your pregnancy, as required.
Emotional health issues. Patients with seizures are more probable to have psychological issues, like depression and anxiety. Issues may be a consequence of problems dealing with the disease itself as well as drug side effects.
Prognosis
The prognosis of persons with seizures relies mainly on any underlying reason. Persons with seizures from remedial medical or toxicologic reasons should do nicely with the management of those problems.
In further persons with acute symptomatic seizures, the prediction is related to the condition procedure. Apparently, as a group, persons with neoplastic reasons for seizures or hypoxic brain damage will not cope well reached to many persons with metabolic reasons for seizures.
The prognosis of a person with a single unprovoked seizure has been nicely delineated. Unprovoked seizures, by meaning, have no established reason after clinical evaluation. If primary studies, involving proper imaging, laboratory work, and possibly EEG, are nondescript, calculations of the repetition rate of another unprovoked seizure within five years are between one-third and one-half. Yet, if there is a second or third unprovoked seizure, the chance of other seizures rises to around three-quarters.
FAQ
Can seizures be cured?
But unlike with further brain-related diseases, nearly two dozen drugs can successfully manage many patients of epilepsy. Although there is no treatment, these anti-seizure medications turn the condition into a chronic, but well-managed situation for many to the end where it hardly interrupts life.
Are seizures painful?
Naturally, the feeling of owning a seizure does not harmful. That’s because some seizures induce unconsciousness, so you’re unaware of what is occurring. Yet, you might keep a headache before or after a seizure.
Is seizure a serious condition?
A seizure that stays longer than five minutes is a medical crisis. Seizures are more familiar than you might believe. Seizures can occur in a closed head injury, after a stroke, an infection like meningitis, or another condition. For many duration, though, the reason for a seizure is unknown.
Is a seizure a mental disorder?
Epilepsy is not a mental disease. The vast prevalence of patients living with epilepsy has no cognitive or psychological issues. For most regions, psychological problems in epilepsy are restricted to patients with extreme and uncontrolled epilepsy.
What are the 4 types of seizures?
Tonic: Muscles in the body evolve rigidly. Atonic: Muscles in the body calm. Myoclonic: Brief jerking in regions of the body. Clonic: Duration of shaking or jerking regions on the body.



15 Comments