Narcolepsy: What It Is, Causes, Symptoms & Treatment
Narcolepsy is a disease where your brain can’t control your capacity to sleep or stay awake. Individuals with this disorder usually fall asleep during the day, along with other symptoms. While this condition is serious and disruptive, it usually reacts well to medicine. With care and precautions, is possible to control this condition and adapt to its effects.
What is Narcolepsy?
Narcolepsy is a sleep disorder that causes an almost overwhelming impulse to suddenly fall asleep throughout the day. Although uncommon, this ailment is well-known due to its symptoms and how they manifest. While narcolepsy is typically curable, it can still seriously impair your social life, career, and quality of life.
Cataplexy (KAT-uh-plek-see), a sudden reduction of muscular tone, is another side effect of narcolepsy sometimes. Strong emotions, particularly laughing, can cause this. Two categories exist for narcolepsy. Cataplexy is a common symptom of type 1 narcolepsy. Type 2 narcolepsy is more common in those without cataplexy. There is no known treatment for narcolepsy, this is a permanent condition. However, medications and alterations in lifestyle can aid in symptom management. Those who have the support of their friends, family, employers, and teachers can manage the disease.
Narcolepsy epidemiology
Narcolepsy affects about 1 in 2,000 persons. But because daytime sleepiness is a symptom of many other diseases, experts estimate that only about half of those who have it are diagnosed. It is believed that both genders are affected by the disease at approximately the same rate. However, some research indicates that men and individuals classified as male at birth are more prone to experience it.
Causes of Narcolepsy
The exact cause of narcolepsy is not clear to professionals. They believe that it involves several factors that work in combination to induce brain issues and impair REM sleep. Much evidence suggests that narcolepsy runs in families. Scientists believe this disorder is caused by a decrease in hypocretin. A hypocretin also known as an orexin, is involved in controlling appetite and sleep patterns.
Researchers are getting nearer to identifying the genes responsible for the illness. Your brain’s synthesis of substances that may indicate sleep and waking cycles is regulated by these genes.
Some specialists believe that a substance called hypocretin is not easily produced by your brain, which may be the cause of narcolepsy. Additionally, abnormalities have been discovered in brain regions that regulate REM sleep.
The specific form of narcolepsy determines the causes of the condition. All of them, though, are connected to the hypothalamus, a particular region of the brain that aids in controlling your wake and sleep cycles.
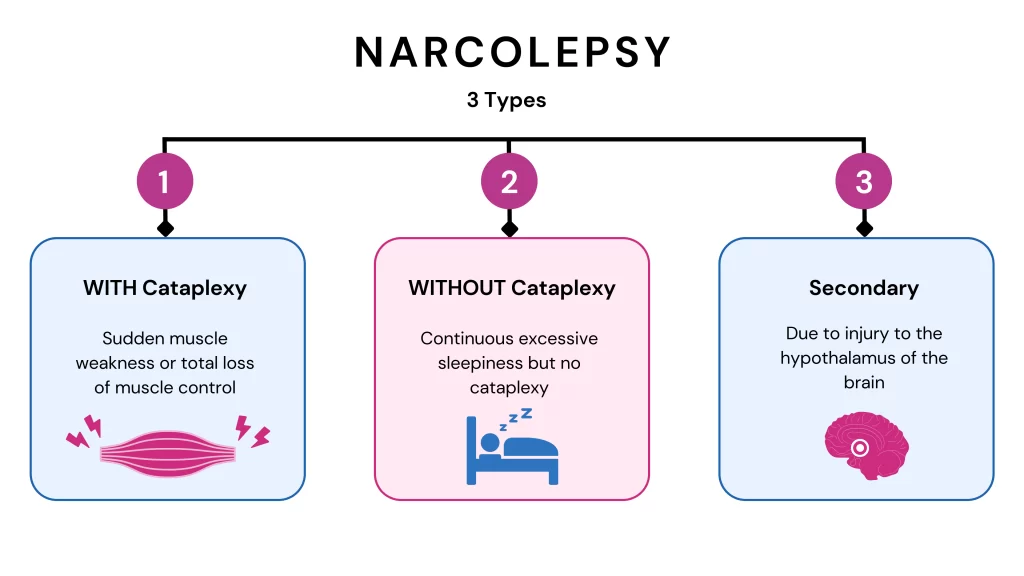
There are three types of narcolepsy:
Type 1 narcolepsy
Researchers identified a class of chemical molecules called orexins in 1998. These neurons, or brain cells, employ these molecules for communication. Your ability to stay awake is mostly dependent on the neurons in the hypothalamus, a region of the brain that contains orexin-using neurons.
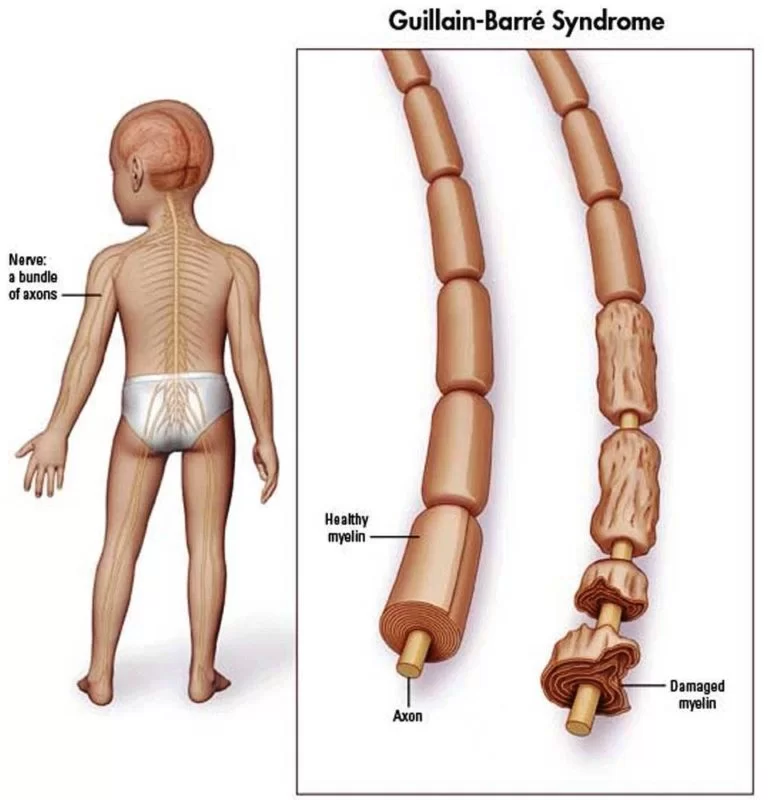
The neuronal substance orexin, also known as hypocretins, is often found in the cerebrospinal fluid (CSF), a thin fluid layer that surrounds and cushions your brain and spinal cord. On the other hand, individuals with narcolepsy have very low, or undetectable, CSF levels of orexin. This indicates that the orexin-producing cells have either been killed or have ceased to function.
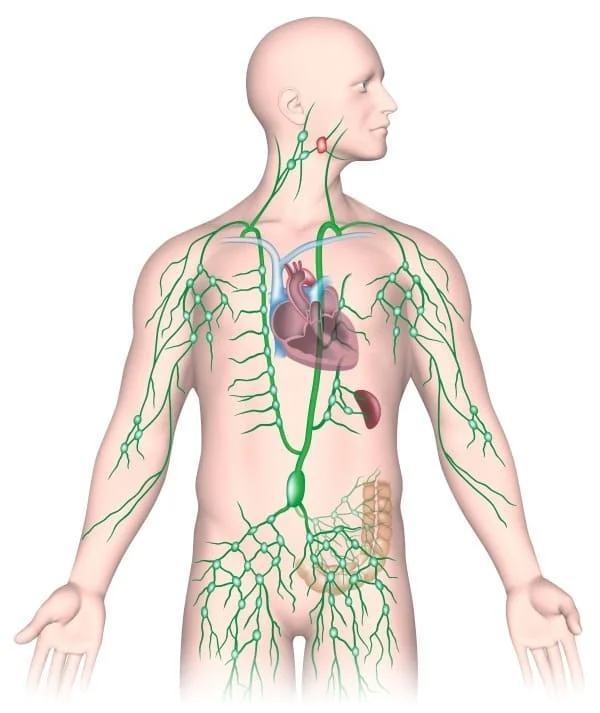
An autoimmune problem is most likely the cause of those neurons’ demise, according to other studies. This implies that either the orexins themselves, the neurons that produce and utilize them, or both, are targeted by your immune system.
The immune system is impacted by a particular genetic mutation (HLA-DQB1*06:02) that affects 90% to 95% of individuals with type 1 narcolepsy. But this mutation is also present in roughly 25% of the population, who do not have narcolepsy. Because of this, specialists don’t often check for this mutation, and they don’t know what function it serves. Additionally, there is evidence that narcolepsy runs in families, as having a first-degree relative (a parent, sibling, or child) who has the disorder increases your chance of getting it.
On the other hand, some viral and bacterial infections—particularly those caused by strep throat bacteria and H1N1 influenza strains—can also result in type 1 narcolepsy in humans. Experts believe that’s because immune system alterations and malfunctions can occasionally be brought on by infections.
Type 2 narcolepsy
Type 2 narcolepsy is not well understood by professionals, but type 1 narcolepsy’s causes are largely understood. The exact cause of type 2 narcolepsy is still a mystery to experts. However, they believe it occurs for related causes. These include an issue with the way orexin moves through your brain or a less severe loss of the neurons that use it.
Secondary narcolepsy
In rare instances, hypothalamic injury might result in narcolepsy. This form of damage can result from strokes, brain tumors, concussions, traumatic brain injuries, and other diseases.
Additionally, narcolepsy may manifest as a trait that is associated with other illnesses. As instances of this, focus on:
- Autosomal dominant deafness, narcolepsy, and cerebellar ataxia (ADCADN).
- Type 2 diabetes, obesity, and autosomal dominant narcolepsy.
What are the symptoms of narcolepsy?

The majority of narcolepsy don’t have all four of the condition’s primary symptoms. The following four symptoms are present:
- Excessive daytime sleepiness. This is a symptom that all narcolepsy experience. Experts and those who suffer from narcolepsy frequently refer to episodes as “sleep attacks.”
- Sudden muscle weakness (cataplexy). Your body may only experience minor side effects or slight muscle weakness as a result of this.
- Sleep-related hallucinations. These occur immediately before or just after going to sleep.
- Sleep paralysis. This symptom causes you to wake up only partially or not at all, but you will constantly be immobile.
More about cataplexy
Narcolepsy is classified into two primary categories, and the presence or absence of cataplexy distinguishes between them. There are two categories:
- Narcolepsy type 1: In this kind, cataplexy is present. Type 1 narcolepsy impacts about 20% of cases.
- Narcolepsy type 2: Cataplexy doesn’t happen in this form. Approximately 80% of occurrences of narcolepsy are type 2.
Normally, your brain blocks your ability to control most of your muscles to prevent you from enacting your dreams. The sudden weakening of muscles experienced by those who suffer cataplexy is comparable to the blockage of movement that occurs during REM sleep.
Only one side of your body or your face and neck (e.g., your jaw lowering involuntarily) may be affected by mild cataplexy. You may sustain injuries if you slump to the ground due to severe cataplexy. These sessions often last a few minutes, but during that period you might not be able to move or speak at all.
Another interesting thing about cataplexy is that it is triggered by specific emotions. Cataplexy is most commonly caused by positive emotions, including laughing, joke-telling, and other humor-related behaviors. Cataplexy can also be brought on by surprise, fear, or anger, though it is less likely to happen.
Cataplexy may appear in slightly different ways in younger individuals and those whose symptoms have only recently begun. For them, cataplexy can appear as sudden, uncontrollably clenching or grimacing their faces, protruding their tongues, or experiencing a loss of muscular tone throughout their body, which causes their limbs to feel “floppy” and their muscles to feel soft.
More about sleep paralysis
To prevent you from enacting your dreams, your brain turns off your ability to regulate your muscles, but this should stop when you wake up. Your body doesn’t regain muscle control as it should, though, if you suffer sleep paralysis. The only things you can still do are breathe and move your eyes, but not speak or move the rest of your body.
A common side effect of sleep paralysis is hallucinations, which are frequently quite vivid and scary. Thankfully, the duration of sleep paralysis is typically quite brief, ranging only a few minutes at most (although individuals experiencing it frequently report feeling this way).
Other symptoms
Apart from the four primary symptoms, individuals with narcolepsy frequently exhibit other symptoms or behaviors. Among the most prevalent or obvious behaviors are some of the following:
- Automatic movements. Narcolepsy patients frequently experience sleeplessness but may still move certain body parts, such as their hands.
- Amnesia or forgetfulness. People who suffer from this illness frequently lose memory of their activities just before going to sleep.
- Sudden outbursts around sleep attacks. Individuals suffering from narcolepsy may exhibit sudden outbreaks of speech, typically uttering meaningless or irrelevant words or phrases about their surroundings. This may shock a person suffering from narcolepsy back to full consciousness, although the majority of those who do this also don’t recall doing it.
Narcolepsy risk factors
One of the risk factors for narcolepsy is your age. Although it can appear at any age, narcolepsy typically first manifests between the ages of 15 and 25. The likelihood of developing narcolepsy increases by 20 to 40 times if there is a family history of the condition.
How does narcolepsy affect my body?
It is helpful to have a better understanding of the human sleep cycle to understand narcolepsy. The stages involved in that cycle are as follows:
- Stage 1: Light sleep. This short stage begins right after you fall asleep and accounts for about 5% of your total sleep time.
- Stage 2: Deeper sleep. This stage is deeper and makes up about 45% to 50% of all the time you spend sleeping (this number goes up as you get older).
- Stage 3: Slow wave sleep. This stage makes up about 25% of the time you spend sleeping (this number goes down with age). Stage 3 sleep is extremely difficult to wake up from, and waking up straight from it typically results in “sleep inertia,” a condition characterized by “mental fog” and weak thinking. Additionally, sleepwalking and sleeptalking usually occur during this period.
- REM sleep: This is the dream stage. You can notice movement beneath the eyelids of someone who is experiencing Rapid eye movement sleep.
When you go to sleep in the absence of narcolepsy, you usually go from stage 1 to stage 2 and 3. You will alternate between these phases until you finally enter REM sleep and begin to dream. You enter a fresh cycle and return to either stage 1 or stage 2 following the first REM cycle. Usually, a cycle lasts 90 minutes, then another one starts. Assuming they obtain eight hours of sleep, most people have four or five cycles every night.
That is not how your sleep cycle functions if you have narcolepsy. Instead, as soon as you fall asleep, you’ll enter the REM period. You’ll sleep for the remainder of the night in little bursts, frequently without experiencing the usual sleep cycle.
You will feel quite drowsy throughout the day if you have narcolepsy, regardless of how well you sleep at night. These naps throughout the day are also brief—about 15 to 30 minutes—but it’s usually tough to resist the impulse to fall asleep. You’ll feel refreshed and prepared to carry on with your previous activities once you wake up. But the reason narcolepsy is so disruptive is because this occurs multiple times a day.
How is narcolepsy diagnosed?
Based on your symptoms, a medical professional may detect narcolepsy in you. However, several other brain and sleep-related disorders have symptoms with narcolepsy. As a result, the diagnosis of narcolepsy can only be made by specialized diagnostic testing.
An attending physician will first ensure that you are getting adequate sleep before proceeding with the majority of the primary narcolepsy testing. This typically entails using straightforward tracking techniques, such as actigraphy, to monitor your sleep-wake cycles. This usually involves tracking movement patterns (e.g., when you’re sleeping vs. when you’re up and moving around while awake) using a watch-like device that you wear on your wrist.
What tests will be done to diagnose narcolepsy?
Some possible tests for diagnosing narcolepsy include:
- Sleep study (polysomnogram).
- Multiple sleep latency test (MSLT).
- Maintenance of wakefulness test.
- Spinal tap (lumbar puncture).
A sleep study (polysomnogram)
Multiple kinds of sensors are used in a sleep study to monitor your sleeping patterns. Electroencephalogram (EEG) sensors are a crucial component of complete sleep research, also called a polysomnogram. These sensors monitor your brain waves, which enables medical professionals to determine your current sleep state minute by minute.
Narcolepsy sufferers sleep abnormally quickly and enter the REM stage of sleep, making a sleep study useful in diagnosing the disorder. Additionally, the sleep study will be able to identify and document the intervals of wakefulness that will interrupt their sleep.
The fact that excessive daytime sleepiness is also a primary sign of sleep apnea underscores the importance of a sleep study. Sleep apnea can be ruled out using a sleep study.
Multiple sleep latency test
This exam assesses your propensity for daytime sleepiness. During this test, timed naps are allowed for a predetermined length of time. This test can help determine whether you have excessive daytime sleepiness, which is one of the required signs of narcolepsy. Usually, this assessment is given the day following an overnight sleep study.
Maintenance of wakefulness test
This test evaluates your capacity to remain awake during the day in situations where it would be easy to fall asleep. It is uncommon in narcolepsy testing, but it may be useful in ruling out other diseases. Evaluating the effectiveness of stimulant therapy is also beneficial.
Spinal tap (lumbar puncture)
If your CSF has low amounts of orexin, this test can help identify them. Diagnosing type 1 narcolepsy is essential. Even if cataplexy is not presently a symptom of narcolepsy, low orexin levels can indicate that it may develop in the future. Sadly, orexin levels are unaffected in individuals with type 2 narcolepsy, thus this test isn’t always helpful in making the diagnosis.
Other tests
For those with narcolepsy, many other tests are also frequently done. Experiencing cataplexy as a symptom is one reason this could occur. There are various other motor (movement-related) symptoms of brain diseases that are comparable to cataplexy, including atonic seizures (sometimes called drop attacks).
It may therefore take longer for medical professionals to identify and diagnose narcolepsy because they may initially test for more serious disorders like seizures and epilepsy. Other tests may also be necessary, and the best person to advise you on which tests to get and why is your healthcare professional.
Management and Treatment
You can treat narcolepsy, but it cannot be cured. Most treatments begin with medication, but lifestyle and daily routine modifications can also be beneficial. Treatment for narcolepsy usually has a good effect, which helps reduce the disturbances that the condition can bring.
What drugs or therapies are used for the treatment of narcolepsy?
The primary approach to treating narcolepsy is medication. Although some drugs also target other symptoms, the majority of treatments target excessive daytime sleepiness. The following medications can be used to treat this disease:
- Wakefulness medications. Typically, these are the initial courses of therapy. Modafinil and armodafinil are two such medications. These drugs act on your neural system, which can reduce the intensity or frequency of excessive daytime sleepiness.
- Amphetamines and amphetamine-like stimulants. medication such as amphetamine/dextroamphetamine combinations (better known by the brand name Adderall®) or methylphenidate (better known under numerous trade names, including Ritalin®, Concerta®, or Qullivant®).
- Antidepressants. drugs such as tricyclic antidepressants like protriptyline or clomipramine, serotonin-norepinephrine reuptake inhibitors (SNRIs) like venlafaxine (commonly known under the trade name Effexor®), selective serotonin reuptake inhibitors (SSRIs) like fluoxetine (better known under the trade name Prozac®).
- Sodium oxy-bate. This medication reduces your incidence of cataplexy and helps you sleep. Even though most nations strictly regulate this medication due to its side effects, type 1 narcolepsy is nevertheless commonly treated with it.
- Histamine-affecting drugs. Pitolisant, a histamine receptor antagonist, is a prime example of this class of medication. Drugs known as receptor antagonists prevent certain molecules in your body from adhering to cells. That causes the cells to function more slowly or not at all.
While there are several ways to treat narcolepsy in adults, there are very few methods available to treat the condition in children. You can get the greatest information about available treatments and recommended courses of action from your child’s pediatrician or other specialised physician.
Complications and side effects of narcolepsy treatment
It is more common for pharmaceuticals that treat narcolepsy or its symptoms to interact with other medications. Medication containing stimulants of any kind can lead to problems such as hypertension (high blood pressure) and arrhythmias (abnormal heart rhythms). Sodium oxybate in particular should never be mixed with alcohol or other medications that impair the function of your central nervous system.
Generally speaking, the best person to advise you about potential side effects, problems, or drug interactions is your healthcare professional. They can adjust the material based on your unique case and circumstances, taking into consideration your medical history and unique set of circumstances.
How can I manage my symptoms or take care of myself?
The attempt to self-diagnose and self-treat narcolepsy should be avoided. This is because the symptoms of this illness frequently coexist with other, more serious illnesses including hazardous diseases like epilepsy or sleep apnea. You should always contact a healthcare provider for a diagnosis and treatment of this problem because it can make some activities risky, like driving or swimming.
Who does narcolepsy affect?
People between the ages of 5 and 50 are typically diagnosed with narcolepsy by medical professionals. However, young adults in their late teens and early 20s are most likely to experience it. Men and those who were assigned male at birth (AMAB) are more likely to become narcoleptics.
How common is narcolepsy?
Narcolepsy is rare. According to available studies, it affects 25–50 persons globally for every 100,000 people. However, it can take years to diagnose this ailment, making it difficult to determine the exact number of affected individuals.
What is the expected time of recovery following therapy, and when will I feel better?
Many factors affect how long it takes for narcolepsy therapies to take effect, including the recovery period. If you’re wondering what to anticipate in your particular situation, such as when to expect drug effects or symptom changes, the best person to advise you on this is your healthcare provider.
Lifestyle and home remedies
The management of narcolepsy symptoms requires lifestyle modifications. You might gain advantages if you:
- Stick to a schedule. Every day, including the weekends, set up the same time to go to bed and wake up.
- Take naps. Plan on taking quick naps throughout the day at regular intervals. 20-minute naps during the day could be restorative. For one to three hours, they could decrease drowsiness. Some people might require lengthier naps.
- Avoid nicotine and alcohol. If you use these drugs, particularly at night, your symptoms can develop worse.
- Get regular exercise. At least four to five hours before going to bed, schedule moderate to regular activity. You might feel more awake throughout the day and get better sleep at night.
How can I prevent narcolepsy or lower my risk?
Most cases of narcolepsy are unexpected. It is therefore impossible to stop it from happening or lower your chance of getting it.
Prognosis
In most cases, narcolepsy is not harmful on its own, but the sudden, excessive desire to sleep can cause significant disruptions. Individuals suffering from this medical condition might not be able to drive (either permanently or temporarily, depending on their circumstances and symptoms).
While type 1 narcolepsy carries an increased risk of damage from falls when cataplexy is severe, narcolepsy is generally not harmful. Additionally, narcolepsy can make driving, using heavy machinery or power tools, swimming, and other activities risky.
Narcolepsy in children
The symptoms of narcolepsy often present difficulties for children. It can be challenging to focus in class, maintain social interactions, and engage in both school-related and extracurricular activities when you’re sleepy during the day.
Though narcolepsy is a medical problem nonetheless. As a result, narcoleptic children frequently have legal safeguards, and schools are required by law to make appropriate accommodations for them. Modifying class schedules, scheduling naps or relaxation intervals, and taking medication while in class are a few examples. You can navigate this and identify answers that will benefit your child with the assistance of other professionals or your child’s pediatrician.
Narcolepsy in working adults
Adult narcoleptics frequently enjoy legal protections due to their condition, similar to the protections provided for children attending schools. Narcolepsy is one of the medical conditions for which discrimination is illegal in the United States under the Americans with Disabilities Act.
Thanks to this legal protection, narcoleptics are frequently able to negotiate accommodations with their employers, allowing them to pursue a profession without having to give up treatment.
How long does narcolepsy last?
Narcolepsy is a lifetime disorder since once it develops, it cannot be cured. It doesn’t, however, get worse with time.
While narcolepsy by itself is not dangerous, it can make it difficult to go to specific locations or engage in specific activities. It can also cause disruptions to regular activities like working and attending school. While there are situations when treatment is ineffective, most narcolepsy cases improve with it. This implies that you can typically control this illness and minimize its impact on your life.
How do I take care of myself?
There are various things you may take to help control your narcolepsy and increase the efficacy of your therapies if you have it. The majority of these, which include the following activities, are related to maintaining appropriate sleep hygiene or changing your habits and schedule in various ways:
- Be consistent with your sleep habits. A sleep, routine will help you get better quality sleep.
- Make time for sleep. Select a bedtime that allows you to obtain the appropriate quantity of sleep for your age. Additionally, you ought to arrange some time for winding down and relaxing before bed.
- Don’t spend too much time on electronics or in bright light. When you expose your body to too much light right before bed, it can interfere with its normal sleep-wake cycles.
- Avoid consuming alcohol or caffeine, utilizing tobacco, or eating a dinner too close to bedtime. If you’re hungry right before bed, the best thing to do is have a little something to eat. whether you take some medications, you should abstain from alcohol completely (your healthcare practitioner can tell you whether they prescribe any of these for you). Additionally, experts strongly advise giving up all tobacco products, including vaping and smokeless tobacco.
- Be physically active. Getting regular exercise, even if it’s only a walk, can improve the quality of your sleep.
- Have a nap. People with narcolepsy will constantly feel better after taking a short nap. Once you’ve identified the times of day you feel the most tired, you can modify your schedule to include naps during those periods.
Avoid risky movements or take protection when you do them
- Narcolepsy can indeed cause catastrophic or even fatal car accidents. It would help if you never drove unless you have a special medical clearance from your doctor to protect you and everyone around you.
- Should you experience any signs of narcolepsy while operating a motor vehicle, you should stop driving and get in touch with your physician. Even if it is inconvenient in the best of circumstances, doing this is essential to preventing fatal or seriously life-altering repercussions from a car crash caused by nodding off while driving.
- In addition, there is a significant risk of narcolepsy during swimming. Wearing a life preserver is mandatory for anyone suffering from narcolepsy whether swimming or in any other type of boat or watercraft when it is advised. A fatal sleep attack in the water could result from not wearing a life preserver or lifejacket, which should be worn appropriately at all times.
When should I see my healthcare provider?
If you find yourself falling off unexpectedly, it’s a good idea to consult a doctor. These are all signs of various illnesses, not only narcolepsy, some of which are rather serious. For many of these disorders, there is a greater chance of complications or less successful treatment the longer you wait to receive a diagnosis and start treatment.
When should I go to the Emergency department?
If you suddenly fall or lose consciousness, you should go to a hospital or emergency room for treatment. This is a major sign of several illnesses, such as irregular heartbeats, heart attacks, and strokes. These ailments require emergency medical attention because they are medical crises. You run the danger of suffering injuries from falls if you collapse or faint unexpectedly.
You should always get medical attention if you have a possible injury to your head, neck, or any part of your back and spine. Any degree of spinal cord fracture or injury carries the risk of lasting harm, paralysis, or even death.
If you take any form of blood thinner and you fall, you should also get medical help, especially if you hit your head. You need to get medical attention to make sure you don’t have any injuries that could result in fatal complications since falls and injuries put you at risk for serious internal bleeding.
Conditions Similar to Narcolepsy
- Some narcoleptics also experience associated issues, such as: When you have periodic limb movement disorder (PLMD), your leg muscles frequently move during the night without conscious control.
- Sleep apnea: During sleep, you frequently stop and start breathing.
- Automatic behavior: You fall off while engaging in a routine task, such as talking, walking, or driving. While you sleep, you carry on with the task, and when you wake up, you have no recall of what you have done.
- Furthermore, narcolepsy-like symptoms can also be caused by a wide range of other disorders. This contributes to the difficulty in diagnosing narcolepsy.
- Moreover, several different illnesses may cause symptoms that resemble narcolepsy. This contributes to the difficulty in diagnosing narcolepsy.
- Daytime sleepiness can also be a symptom of other sleep disorders such as sleep apnea and insomnia. Depression and other mental health issues might also do this. It’s also possible to confuse narcolepsy with substance use disorders or epilepsy.
- Idiopathic hypersomnolence (IH), a related disorder, also causes daytime sleepiness. However, in contrast to those who suffer from narcolepsy, individuals with insomnia hypersomalopathy (IH) frequently sleep for ten to eleven hours at a time and struggle to wake up.
Complications of narcolepsy
- The complications associated with narcolepsy include:
- Depression and anxiety are common in narcoleptics, though it’s unknown if these are actual symptoms of the disease or just a result of how it affects their quality of life.
- Your social life might be impacted by excessive drowsiness and cataplexy. For instance, you could find it hard to stay awake at parties, or laughing causes you to lose your grip on your body.
- A slower metabolism or decreased activity levels may be the reason for the obesity that many narcoleptics experience. On average, adults with narcolepsy weigh 15–20% more than the normal population.
- Suicidal thoughts and actions may be more common in narcoleptics, according to a 2017 research.
- You won’t always experience these issues if you have narcolepsy because of this.
- Managing symptoms and side effects of therapy in close collaboration with your healthcare team is one of the greatest methods to prevent or minimize narcolepsy consequences.
Note
A brain-related disorder called narcolepsy breaks off your body’s normal sleep/wake cycles. Although this illness doesn’t normally pose a direct threat, there are times when it might. It’s a condition that can also drastically interfere with daily activities, routines, and life. Driving and working are two common activities that many people with this illness may find difficult.
Thankfully, narcolepsy is curable, and most patients experience at least some improvement with treatment. Changing sleep-related habits might also be beneficial. Although narcolepsy symptoms cannot always be avoided, many people can control the illness and adjust to most, if not all, of its effects.
FAQ
What is the primary reason behind narcolepsy?
One brain molecule that controls sleep, termed hypocretin (sometimes called orexin), is suspected to be deficient in many narcolepsy patients. It is believed that the immune system accidentally damaged the areas of the brain responsible for producing hypocretin, causing the deficit.
Which five symptoms are related to narcolepsy?
excessive tiredness during the day. Individuals who suffer from narcolepsy often nod off without warning.
sudden onset of muscular atrophy. We refer to this disorder as cataplexy.
sleep paralysis: One of the most typical signs of narcolepsy is sleep paralysis.
Hallucinations.
Transitions in rapid eye movement (REM) sleep.
Which are the two narcolepsy triggers?
Hormonal changes that can happen during puberty or menopause are among the things that have been proposed as potential narcolepsy triggers. significant psychological strain. an illness, such as the swine flu, or the vaccine used to prevent it (Pandemrix)
What are narcolepsy’s early warning indicators?
excessive drowsiness during the day. The initial indication of narcolepsy is typically excessive daytime sleepiness.
Attacks of sleep. People who have narcolepsy also frequently experience sleep attacks, which are episodes of sudden and unexpected falling asleep.
Cataplexy.
Sleep paralysis.
Other symptoms.
What is narcolepsy’s initial stage?
One of the main early indicators of narcolepsy is excessive daytime drowsiness, which is defined as persistently tired during the day regardless of how much sleep you got the night before. However, many people who experience significant weariness during the day may not realize they have narcolepsy.
What is the home test method for narcolepsy?
Narcolepsy testing cannot be done at home. Because it does not have the required tracking of brain activity, or view source. When diagnosing narcolepsy, the PSG and MSLT values can be very important.
Is narcolepsy detectable by blood test?
A blood genetic test called Human Leukocyte Antigen is another typical test that Harvard Sleep Specialists run for narcolepsy if they detect hypocretin insufficiency in addition to the mentioned tests.
Are there any risks associated with narcolepsy?
Your daily life can be significantly impacted by narcolepsy, which can also be dangerous because it can cause you to suddenly drop out while engaging in regular tasks like eating, working, or driving. Although narcolepsy cannot be cured, it can be managed with medication and good lifestyle choices.
References
- Professional, C. C. M. (n.d.-e). Narcolepsy. Cleveland Clinic. https://my.clevelandclinic.org/health/diseases/12147-narcolepsy
- Narcolepsy – Diagnosis and treatment – Mayo Clinic. (2023, January 14). https://www.mayoclinic.org/diseases-conditions/narcolepsy/diagnosis-treatment/drc-20375503
- WebMD Editorial Contributors. (2006, January 31). Narcolepsy: symptoms, causes, treatment. WebMD. https://www.webmd.com/sleep-disorders/narcolepsy
- Lights, V. (2022, March 6). Narcolepsy. Healthline. https://www.healthline.com/health/narcolepsy#complications
- Fnp, K. D. (2023, November 28). What to know about narcolepsy. https://www.medicalnewstoday.com/articles/155244#tests-and-diagnosis