Epilepsy
What is Epilepsy?
Epilepsy is a long-term brain disease where a patient has repeated seizures. It is considered to involve approximately 3 people in every 100 patients with seizures. Having only one seizure is not considered to be epilepsy almost half the patients who have one seizure never have another seizure.
Epilepsy is not one single disease. There is a range of various diseases that can generate seizures. Seizures generally stay 1 to 3 minutes. If a person has a seizure that stays for more than 5 minutes, contact an ambulance.
Symptoms of Epilepsy
Because epilepsy is induced by abnormal movement in the brain, seizures can involve any function of your brain coordinates. Epilepsy signs and symptoms may contain:
- Temporary confusion
- A staring spell
- Stiff muscles
- Uncontrollable jerking motions of the upper and lower extremities
- Loss of consciousness or awareness
- Psychological symptoms like anxiety, fear, or deja vu ( associated with temporal lobe epilepsy )
Symptoms differ depending on the kind of seizure. In most circumstances, a patient with epilepsy will manage to have the same kind of seizure per time, so the symptoms will be equal from episode to episode.
Doctors or physicians normally categorize seizures as either focal or generalized, establishing how and where the irregular brain activity starts.
Causes of Epilepsy
Epilepsy has no identifiable reason in almost half the patients with the disease. In the further half, the disease may be traced to different factors, including:
Genetic influence. Some varieties of epilepsy, which are classified by the variety of seizures you feel or the region of the brain that is involved, run in families. In these circumstances, there’s likely a genetic influence.
Investigators have connected some varieties of epilepsy to precise genes, but for most patients, genes are just a portion of the reason for epilepsy. Specific genes may make a patient more sensitive to environmental situations that activate seizures.
Head trauma. Head trauma as an outcome of a car accident or further traumatic injury can generate epilepsy.
Brain abnormalities. Abnormalities in the brain, involving brain tumors or vascular malformations like arteriovenous malformations (AVMs) and cavernous malformations, can generate epilepsy. Stroke is the greatest reason for epilepsy in grown-ups older than age 35.
Infections. HIV, Meningitis, viral encephalitis, and some parasitic infections can generate epilepsy.
Prenatal injury. Before birth, infants are sensitive to brain injury that could be induced by several factors, like an infection in the mother, inadequate nutrition, or oxygen shortages. This brain injury can result in epilepsy or cerebral palsy.
Developmental disorders. Epilepsy can occasionally be associated with developmental diseases, such as autism.
Risk factors
Specific factors may raise your risk of epilepsy:
Age. The beginning of epilepsy is most familiar in kids and older grown-ups, but the disease can happen at any age.
Family history. If you have a family record of epilepsy, you may be at a raised risk of developing a seizure condition.
Head injuries. Head damages are liable for some patients with epilepsy. You can decrease your risk by wearing a seat strap while riding in a car and by wearing a helmet while skiing, bicycling, riding a motorcycle, or engaging in further exercises with a high risk of head damage.
Stroke and further vascular conditions. Stroke and further blood vessel (vascular) conditions can conduct brain damage that may activate epilepsy. You can bring several measures to decrease your risk of these conditions, involving restricting your intake of alcohol and avoiding cigarettes, consuming a healthy diet, and exercising daily.
Dementia. Dementia can raise the risk of epilepsy in older grown-ups.
Brain infections. Infections like meningitis, which generates inflammation in your brain or spinal cord, can raise your risk.
Seizures in childhood. Elevated fevers in childhood can occasionally be associated with seizures. Kids who have seizures due to high fevers normally won’t produce epilepsy. The risk of epilepsy raises if a kid has a long fever-associated seizure, another nervous system disease, or a family record of epilepsy.
Diagnosis
To diagnose your disease, your doctor or physician will check your symptoms and medical record. Your doctor or physician may order several examinations to diagnose epilepsy and specify the reason for seizures. Your evaluation may contain:
A neurological examination. Your doctor or physician may test your motor capabilities, behavior, mental function, and further locations to diagnose your disease and determine the variety of epilepsy you may have.
Blood tests. Your doctor or physician may carry a blood sample to inspect for signs of infections, genetic diseases, or further conditions that may be associated with seizures.
Your doctor may also recommend examinations to see brain abnormalities, like:
Electroencephalogram (EEG). This is the most familiar examination used to analyze epilepsy. In this examination, electrodes are connected to your scalp with a paste-like substance or cap. The electrodes document the electrical movement of your brain.
If you have epilepsy, it’s familiar to have differences in your normal design of brain waves, even when you’re not keeping a seizure. Your doctor or physician may observe you on video when performing an EEG while you’re awake or asleep, to document any seizures you experience. Documenting the seizures may assist the doctor or physician choose what variety of seizures you’re having or rule out further diseases.
The examination may be done in a doctor’s or physician’s office or the hospital. If proper, you may even have a mobile EEG, which you wear at home while the EEG documents seizure movement over a few days.
Your doctor or physician may give you instructions to accomplish something that will generate seizures, like obtaining short sleep before the examination.
High-density EEG. In a variation of an EEG examination, your doctor may suggest high-density EEG, which spaces electrodes near conventional EEG around half a centimeter separated. High-density EEG may assist your doctor more specifically decide which regions of your brain are involved in seizures.
Computerized tomography (CT) scan. A CT scan utilizes X-rays to receive cross-sectional pictures of your brain. CT scans can show abnormalities in the form of your brain that might be generating your seizures, like bleeding, tumors, and cysts.
Magnetic resonance imaging (MRI). An MRI utilizes strong magnets and radio waves to develop a precise picture of your brain. Your doctor may be capable to notice lesions or abnormalities in your brain that could be generating your seizures.
Functional MRI (fMRI). A functional MRI estimates the differences in blood flow that happen when precise regions of your brain are functioning. Doctors may utilize an fMRI before surgery to determine the precise areas of critical functions, like speech and motion, so that surgeons can avoid damaging those sites while operating.
Positron emission tomography (PET). PET scans use a tiny portion of low-dose radioactive material that’s injected into a vein to assist visualize the metabolic movement of the brain and see abnormalities. Regions of the brain with low metabolism may show where seizures happen.
Single-photon emission computerized tomography (SPECT). This variety of examinations is used especially if you’ve had an MRI and EEG that didn’t pinpoint the area in your brain where the seizures are creating.
A SPECT test uses a tiny portion of low-dose radioactive material that’s injected into a vein to form a detailed, 3D map of the blood flow movement in your brain during seizures. Regions of higher than normal blood flow during a seizure may suggest where seizures happen.
Doctors may also perform a form of a SPECT test known as subtraction ictal SPECT coregistered to MRI (SISCOM), which may deliver even more-detailed outcomes by overlapping the SPECT outcomes with a person’s brain MRI.
Neuropsychological tests. In these examinations, doctors evaluate your thinking, memory, and speech talents. The test outcomes assist doctors to specify which regions of your brain are involved.
Along with your examination outcomes, your doctor may use a mixture of analysis methods to assist pinpoint where in the brain seizures begin:
Statistical parametric mapping (SPM). SPM is a form of comparing regions of the brain that have raised blood flow during seizures to normal brains, which can provide doctors with an opinion of where seizures start.
Electrical source imaging (ESI). ESI is a method that accepts EEG information and projects it onto an MRI of the brain to guide doctors to where seizures are happening.
Magnetoencephalography (MEG). MEG estimates the magnetic fields created by brain movement to determine potential locations of seizure start.
A proper diagnosis of your seizure variety and where seizures start provides you with the best option for discovering a useful therapy.
Treatment of Epilepsy
Doctors normally start by managing epilepsy with a drug. If drugs don’t treat the disease, doctors may suggest surgery or another variety of therapy.
Medication
Most patients with epilepsy can evolve seizure-free by bringing one anti-seizure drug, which is also known as an anti-epileptic drug. Others may be capable to reduce the frequency and intensity of their seizures by bringing a variety of drugs.
Many kids with epilepsy who aren’t feeling epilepsy symptoms can finally discontinue drugs and live a seizure-free life. Many grown-ups can stop drugs after two or more years without seizures. Your doctor will inform you regarding the proper time to stop bringing drugs.
Discovering the right drug and dosage can be difficult. Your doctor will evaluate the frequency of seizures, your situation, your age, and further aspects when selecting which drug to define. Your doctor will also examine any further drugs you may be carrying, to confirm the anti-epileptic drugs won’t interact with them.
Your doctor probably will first define a single drug at a fairly low dosage and may raise the dosage slowly until your seizures are well maintained.
There are more than 20 various varieties of anti-seizure drugs available. The drug that your doctor decides to manage your epilepsy relies on the kind of seizures you have, as nicely as further factors like your age and further health diseases.
These drugs may have some side effects. Mild side effects contain:
- Fatigue
- Dizziness
- Weight gain
- Loss of bone density
- Skin rashes
- Loss of coordination
- Speech issues
- Memory and thinking issues
More severe but rare side effects contain:
- Depression
- Suicidal thoughts and behaviors
- Severe rash
- Inflammation of specific organs, like your liver
To perform the best seizure control likely with drugs, follow these actions:
Bring drugs exactly as specified.
Always contact your doctor before changing to a generic version of your drug or bringing further prescription drugs, over-the-counter medicines, or herbal remedies.
Never stop bringing your drug without speaking to your doctor.
Tell your doctor directly if you see new or raised feelings of suicidal ideas, depression, or unusual differences in your mood or behaviors.
Inform your doctor if you have migraines. Doctors may specify one of the anti-epileptic drugs that can control your migraines and manage epilepsy.
At least half of the patients recently analyzed with epilepsy will evolve seizure-free with their first drug. If anti-epileptic drugs don’t deliver satisfactory outcomes, your doctor may recommend surgery or further treatments. You’ll have routine follow-up meetings with your doctor to assess your situation and drugs.
Physiotherapy treatment in Epilepsy
The goals of physiotherapy
- To form strength sufficiently to defend one head upright
- To have balance and motor control to keep their trunk at the midline
- To use many various muscle groups
- To assist required movement in their trunk and extremities
The physiotherapists document short-term goals for per of the things on the issue list that require to be covered to assist the person gain the long-term goals
- To understand what the person is fine at and does well
- To concentrate on what he or she is skilled at doing instead of what they or can’t do
- To familiarize and supply awareness to prevent damages
- For instance, suggestion on certain swimming tools to control drowning if he/she brings seizures in the pool
- Padding out sharp edges in the house to control injury if dropped on
Physiotherapy treatment for a recovered fracture consists of boosting muscles that have obtained weak from being immobilized and stretching muscles that are rigid owing to being in the cast for a prolonged period.
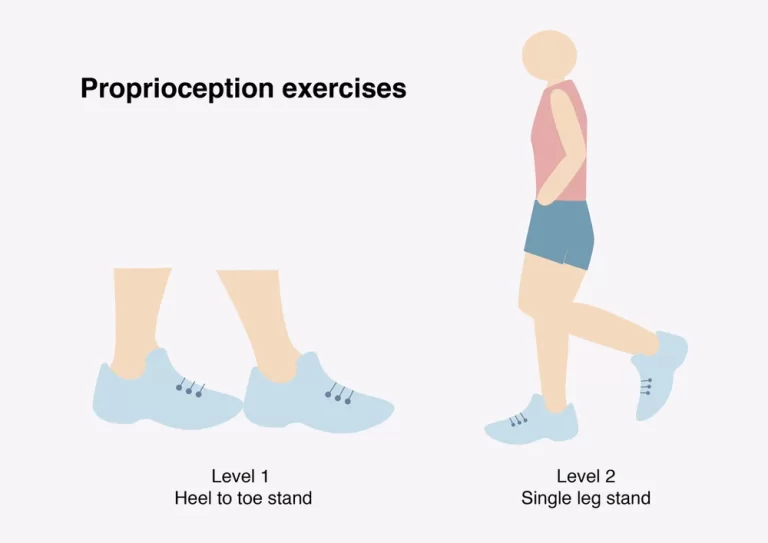
Patients with epilepsy should contain activity as a complementary treatment not only for seizure management but also for non-seizure diseases like physical health promotion and psychosocial adjustment and progress in mental condition. Patients with epilepsy should be motivated to activity and actions should be created to remove any obstacles to exercise. To achieve these purposes, the support of health authorities, sports educators, social workers, and campaigns to tell and stimulate people to evolve more involved are required.
Exercise enhances energy, fitness, and mood and reduces stress.
Enhancing general health and well-being in this way can assist decrease seizures and the effect of epilepsy for some patients. It also creates patients to feel more in command of their health.
Exercise discharges feel-good hormones into the brain, assists to maintain the muscles active, decreases fat levels in the body, and improves oxygen flow to the brain. It can also improve bone density
The neuroprotective and antiepileptogenic measures of activity boost the role of activity intervention as complementary nonpharmacological therapy for epilepsy
Surgery
When drugs fail to deliver sufficient control over seizures, surgery may be a choice. With epilepsy surgery, a surgeon extracts the region of your brain that’s generating seizures.
Doctors generally conduct surgery when examinations show that:
Your seizures develop in a little, well-defined region of your brain
The region in your brain to be performed on doesn’t interrupt vital functions like language, speech, vision, motor function, or hearing
For some kinds of epilepsy, minimally invasive techniques like MRI-guided stereotactic laser ablation may deliver useful therapy when an open method may be too risky. In these methods, doctors or surgeons direct a thermal laser probe at the precise location in the brain generating seizures to kill that tissue to better manage the seizures.
Although many patients continue to require some drug to assist prevent seizures after successful surgery, you may be capable to carry fewer medications and decrease your dosages.
In a tiny number of patients, surgery for epilepsy can induce complications like ever altering your thought (cognitive) capabilities. Speak to your surgeon regarding his or her feelings, victory rates, and difficulty rates with the method you’re considering.
Apart from drugs and surgery, these potential treatments suggest an alternative for managing epilepsy:
Vagus nerve stimulation. In vagus nerve stimulation, doctors or surgeons plant a machine known as a vagus nerve stimulator under the skin of your chest, parallel to a heart pacemaker. Wires from the stimulator are joined to the vagus nerve in your neck.
The battery-powered machine transmits bursts of electrical energy via the vagus nerve and to your brain. It’s not obvious how this interferes with seizures, but the machine can generally decrease seizures by 20-40%.
Most patients still require to carry the anti-epileptic drug, although some patients may be capable to lower their drug dose. You may feel side effects from vagus nerve stimulation, like hoarse voice, throat pain, shortness of breath, or coughing.
Ketogenic diet. Some kids with epilepsy have been capable to decrease their seizures by obeying a severe diet that’s high in fats and low in carbohydrates.
In this diet, known as a ketogenic diet, the body breaks down fats rather than carbohydrates for energy. After a few years, some kids may be capable to quit the ketogenic diet under close maintenance of their doctors and stay seizure-free.
Confer a doctor if you or your kid is handling a ketogenic diet. It’s essential to make certain that your kid doesn’t evolve malnourished when following the diet.
Side effects of a ketogenic diet may contain constipation, dehydration, delayed growth because of nutritional shortages, and a buildup of uric acid in the blood, which can generate kidney stones. These side effects are unusual if the diet is correctly and medically managed.
Obeying a ketogenic diet can be a challenge. Low-glycemic index and modified Atkins diets show less restrictive options that may still deliver some help for seizure management.
Deep brain stimulation. In deep brain stimulation, surgeons plant electrodes into a precise region of your brain, normally your thalamus. The electrodes are attached to a generator planted in your chest. The generator regularly transmits electrical pulses to your brain at timed intervals and may decrease your seizures. Deep brain stimulation is frequently used for a patient whose seizures don’t obtain better with a drug.
Responsive neurostimulation. These implantable, pacemaker-like machines can assist greatly decrease how frequently seizures happen. These responsive stimulation machines examine brain activity patterns to see seizures as they create and deliver an electrical charge or medication to stop the seizure before it generates impairment. Investigation indicates that this treatment has few side effects and can deliver long-term seizure relief.
Potential future treatments
Investigators are investigating many potential new therapies for epilepsy, involving:
Continuous stimulation of the seizure beginning zone (subthreshold stimulation). Subthreshold stimulation continuous stimulation to a location of your brain below a level that’s physically noticeable seems to enhance seizure results and quality of life for some patients with seizures. Subthreshold stimulation assists stop a seizure before it occurs. This therapy method may work in a patient who has seizures that begin in a region of the brain that can’t be extracted because it would impact speech and motor roles (eloquent region). Or it might help a patient whose seizure features mean their possibilities of victorious therapy with responsive neurostimulation are low.
Minimally invasive surgery. New minimally invasive surgical methods, like MRI-guided concentrated ultrasound, conduct promise to manage seizures with rarer risks than conventional open-brain surgery for epilepsy.
Transcranial magnetic stimulation (TMS). Transcranial magnetic stimulation – TMS involves concentrating magnetic fields on regions of the brain where seizures happen to manage seizures without the requirement for surgery. It may be used for persons whose seizures happen close to the surface of the brain and are not prospects for surgery.
External trigeminal nerve stimulation. Equal to vagus nerve stimulation, this machine would stimulate precise nerves to decrease the frequency of seizures. But unlike vagus nerve stimulation, this machine would be worn externally so that no surgery to plant the machine is required. In analyses, external trigeminal nerve stimulation delivered progress in both seizure management and mood.
Lifestyle and home remedies
Understanding your disease can assist you to bring better management of it:
Bring your drug perfectly. Don’t change your dosage before speaking to your doctor. If you sense your drug should be altered, consult it with your doctor.
Obtain sufficient sleep. Lack of sleep can activate seizures. Be certain to get fine rest every night.
Wear a medical warning bracelet. This will assist emergency personnel to understand how to manage you perfectly.
Exercise. Exercising may assist to maintain you physically fit and ease depression. Make certain to drink sufficient water, and rest if you obtain tired during the activity.
In extra, make healthy life options, like managing stress, restricting alcoholic drinks, and avoiding cigarettes.
Complications of Epilepsy
Having a seizure at specific times can conduct in cases that are harmful to yourself or others.
Falling. If you drop during a seizure, you can harm your head or break a bone.
Drowning. If you have epilepsy, you’re 13-19 times more probable to drown while swimming or bathing than the rest of the people because of the chance of having a seizure while in the water.
Car accidents. A seizure that generates either loss of awareness or control can be harmful if you’re driving a car or using other tools.
Many conditions have driver’s license limitations connected to a driver’s capability to prevent seizures and impose a minimum quantity of time that a driver is seizure-free, varying from months to years, before being permitted to drive.
Pregnancy complications. Seizures during pregnancy pose risks to both mother and infant, and precise anti-epileptic drugs raise the risk of birth defects. If you have epilepsy and you’re thinking evolving pregnant, speak to your doctor as you prepare for your pregnancy.
Most females with epilepsy can evolve pregnantly and have healthy babies. You’ll require to be carefully observed throughout pregnancy, and drugs may require to be adjusted. You must work with your doctor to schedule your pregnancy.
Emotional health issues. Patients with epilepsy are more probable to have psychological issues, particularly anxiety, depression, and suicidal ideas and behaviors. Issues may be an outcome of problems dealing with the disease itself as well as drug side effects, but even patients with well-controlled epilepsy are at raised risk.
Further life-threatening difficulties of epilepsy are uncommon, but may occur, like:
Status epilepticus. This situation happens if you’re in a state of continuous seizure activity staying more than five minutes or if you have regular recurrent seizures without recovering full consciousness in between them. Patients with status epilepticus have a raised risk of permanent brain injury and death.
Sudden unexpected death in epilepsy (SUDEP). Patients with epilepsy also have a little risk of sudden shocking death. The reason is unknown, but some analysis indicates it may happen due to heart or respiratory diseases.
Patients with frequent tonic-clonic seizures or patients whose seizures aren’t managed by drugs may be at higher risk of SUDEP. Altogether, approximately 1% of patients with epilepsy die of SUDEP. It’s most familiar in those with extreme epilepsy that doesn’t react to the therapy.
How to Prevent Epilepsy?
A calculated 25% of epilepsy patients are preventable.
Preventing head injury is the most useful manner to control post-traumatic epilepsy.
Good perinatal care can decrease new issues of epilepsy induced by birth injury.
The use of medications and further ways to lower the body temperature of a feverish kid can decrease the possibility of febrile seizures.
The prevention of epilepsy associated with stroke is concentrated on cardiovascular risk factor decrease, eg. steps to prevent or maintain diabetes and obesity, high blood pressure, and the avoidance of tobacco and extreme alcohol use.
Central nervous system diseases are familiar reasons for epilepsy in tropical regions, where many low- and middle-income nations are concentrated. Elimination of parasites in these atmospheres and instruction on how to avoid infections can be useful ways to decrease epilepsy worldwide, for instance, those patients due to neurocysticercosis.
FAQ
Can you live a normal life with epilepsy?
Most patient with epilepsy lives a complete life. Yet, the risk of earlier death is more elevated for some. We know that the best likely seizure management and living safely can decrease the risk of epilepsy-related death.
Is epilepsy a serious illness?
Epilepsy is a chronic noncommunicable condition of the brain that involves patients of all ages. About 50 million patients worldwide have epilepsy, creating it one of the most familiar neurological conditions globally. Almost 80% of patients with epilepsy live in low- and middle-income nations.
Can epilepsy be cured?
But unlike with different brain-related diseases, nearly two dozen drugs can successfully manage many patients of epilepsy. Although there is no treatment, these anti-seizure medications turn the condition into a chronic, but well-managed situation for many to the moment where it slightly interrupts life.
What is the last stage of epilepsy?
Ending (post-ictal) phase
This is the healing phase and during this stage, any physical after-effects of the seizure are felt. The variety of seizures and the region of the brain include will choose how long it brings for a patient to return to their normal self. Some familiar signs of this stage contain Confusion.
How long can a person with epilepsy live?
A decrease in life expectancy can be up to 2 years for a patient with an analysis of idiopathic/cryptogenic epilepsy, and the deduction can be up to 10 years in patients with symptomatic epilepsy. Declines in life expectancy are most elevated at the duration of analysis and reduce with time.





3 Comments