Sleep Paralysis: Causes, Symptoms, and Treatment
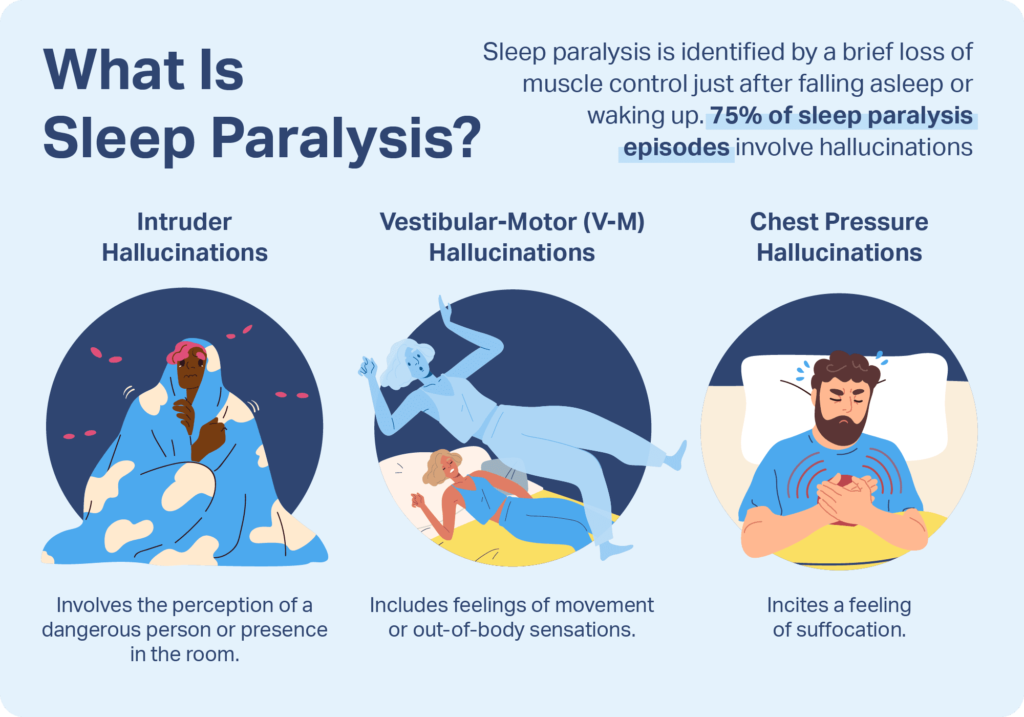
Sleep paralysis is a phenomenon characterized by a temporary inability to move or speak while transitioning between sleep stages. Typically occurring during the onset of sleep or upon waking, it is often accompanied by vivid hallucinations and a sense of pressure on the chest. Paralysis is temporary and is not a sign of a major medical problem.
Pinpointing the source of your symptoms and managing them can help you avoid future attacks. Momentary loss of motor control right after going to sleep or right before waking up is called sleep paralysis. Suffocation or hallucinations are common symptoms of sleep paralysis.
Sleep paralysis is associated with sleep difficulties and some mental health concerns, while its specific cause is unknown. Individuals who work shifts or experience jet lag that interferes with their sleep-wake cycles may be more susceptible to sleep paralysis.
What is Sleep Paralysis?
Sleep paralysis is a condition in which you are awake but immobile. It happens when a person goes from one state of wakefulness to another. You might be unable to move or speak for a few seconds to many minutes throughout these transitions.
Some folks could also experience choking or pressure. Narcolepsy and other sleep disorders may be accompanied by sleep paralysis. An issue with the brain’s ability to regulate sleep is the cause of narcolepsy, which is an overwhelming urge to sleep.
Types of Sleep Paralysis
- Isolated sleep paralysis: The underlying diagnosis of narcolepsy, a neurological condition that impairs the brain’s ability to regulate alertness and frequently results in sleep paralysis, is unrelated to these isolated episodes of sleep paralysis.
- Recurrent sleep paralysis: Multiple episodes of sleep paralysis occur over time in this syndrome. Narcolepsy and recurrent sleep paralysis are linked.
Recurrent isolated sleep paralysis (RISP) is a condition that involves recurring episodes of sleep paralysis in an individual who does not have narcolepsy. These two distinguishing features are frequently combined to identify this condition.
The symptoms include:
- Paralysis in your limbs.
- Inability to speak.
- Sense of suffocation
- Hallucinations.
- Fear.
- Panic.
- Helplessness.
- Tightening around your throat.
According to research on sleep, sleep paralysis is typically only an indication that your body is not progressing through the phases of sleep as it should. Sleep paralysis rarely has a deep underlying psychological cause. The old hag from Shakespeare’s Romeo and Juliet, unseen night demons from antiquity, and alien abductors are just a few examples of the various “evil” entities linked to sleep paralysis symptoms over the ages.
Tales of sinister, demonic monsters that terrorize defenseless people at night have been told in almost every culture throughout history. People have long searched for answers to this enigmatic paralysis during sleep and the horror that goes along with it.
Sleep Paralysis Causes
The condition has many causes, including:
- Narcolepsy.
- Shift work.
- Sleep deprivation.
- Obstructive sleep apnea.
- Difficulty breathing.
It’s unclear exactly why or how it occurs. Because sleep paralysis typically occurs as a person enters or exits REM sleep, researchers think that disruptions in the rapid eye movement cycle are the cause of sleep paralysis. They don’t act out their dreams at that point because their brains usually paralyze their muscles regardless. However, the sufferer of sleep paralysis is aware that they are immobile since they are either fully or partially awake.
According to studies, 25% to 50% of Americans have experienced sleep paralysis at least once. Many of those who suffer from it also have narcolepsy, a condition that causes them to fall asleep randomly. Sleep specialists speculate that sleep paralysis may have some hereditary roots. Additional factors include stress and irregular sleep patterns (e.g., jet lag, staying up late). Studies have also discovered connections between sleep paralysis and panic disorders or social anxiety. Breathing difficulties, loud buzzing noises, and feeling pulled out of bed or in midair are frequently experienced in conjunction with the experience. According to some studies, the reason behind reports of extraterrestrial abductions is sleep paralysis.
What does sleep paralysis feel like?
The inability to move or talk is known as atonia, and it is the defining sign of sleep paralysis. During episodes of sleep paralysis, people also describe breathing difficulties, chest pressure, and unpleasant feelings like panic or powerlessness.
The day following sleep paralysis, it’s typical to feel overly tired or sleepy. Differentiated hallucinations from ordinary dreams are reported to occur in approximately 75% of sleep paralysis episodes. These may appear as hypnagogic hallucinations during sleep or as hypnopsychic hallucinations upon awakening.
Three types of hallucinations occur during sleep paralysis.
- Intruder hallucinations: These hallucinations include the impression that someone or something is threatening in the space.
- Chest pressure hallucinations: These episodes, also known as incubus hallucinations, might cause you to feel as though someone is sitting on your chest or that you are being suffocated. These often coexist with hallucinations of intruders.
- Vestibular-motor (V-M) hallucinations: Feelings of movement, such as flying, or an out-of-body experience are common in V-M hallucinations.
How common is sleep paralysis?
Although prevalence varies, experts estimate that 20% of adults Around the world, more than 2 million healthcare professionals decide to support appropriate care decisions and promote improved health outcomes. offers concise, actionable, and richly insightful evidence-based clinical decision support. have paralysis from sleep at some point in their lives.
The frequency of recurrence of episodes in this group is not well documented. Although sleep paralysis can strike at any age, the initial signs and symptoms typically appear in early childhood, adolescence, or early adulthood. Episodes may begin in adolescence and become more common throughout a person’s 20s and 30s.
When does Sleep Paralysis usually occur?
Sleep paralysis usually occurs one of two times. If it occurs while you are falling asleep, it’s called hypnagogic or preorbital sleep paralysis. It is referred to as post-digital sleep paralysis or hypnopompic if it occurs when you are waking up.
What happens with hypnagogic sleep paralysis?
Your body relaxes gradually as you go off to sleep. Usually, you lose awareness and fail to recognize the shift. But if you stay awake or wake up during sleep, you might realize that you’re speechless and unable to move.
What happens with hypnopompic sleep paralysis?
Your body cycles between NREM (non-rapid eye movement) and REM (rapid eye movement) sleep while you sleep. A typical REM and NREM sleep cycle lasts for roughly ninety minutes. Your total sleep time can be up to 75% of NREM sleep, which happens first.
In a non-REM dream state, your body relaxes and repairs itself. When NREM ends, your sleep shifts to REM. Your body remains perfectly comfy, but your eyes dart quickly and you start to dream. You might discover that you are immobile and unable to talk if you awaken before the REM cycle is complete.
Who develops sleep paralysis?
Up to 40% of people may suffer from sleep paralysis. Sometimes teens are the first to notice this common illness. On the other hand, it can impact people of any age. Sleep disorders can run in families. The following are other possible causes of sleep paralysis:
- Lack of sleep
- Sleep schedule that changes
- Sleeping on your back
- Additional sleep issues like narcolepsy or leg cramps at night
- Substance abuse
- Poor sleep quality
- High-stress levels
- Disorders related to the mind, such as panic disorder (recurrent panic attacks, frequently without obvious explanation) and bipolar disorder, a mental illness that can lead to fluctuations in energy and mood
- A family history of sleep paralysis
- Excessive use of alcohol, especially near bedtime
- Use of certain medications, such as stimulants for attention deficit hyperactivity disorder (ADHD) or beta-blockers (a class of medications used to reduce blood pressure), like Inderal LA (propranolol)16
Diagnosis
You probably have isolated recurring sleep paralysis if you notice that you are immobile or unable to speak for a few seconds or minutes when you go to sleep or wake up. This ailment usually doesn’t require treatment.
If you have any of these worries, consult your physician:
- You feel anxious about your symptoms.
- You feel extremely exhausted during the day as a result of your symptoms.
- You can’t sleep at night because of your symptoms.
Any of the following procedures could be used by your doctor to get more details regarding the quality of your sleep:
- Request that you detail your symptoms and that you maintain a sleep diary for a few weeks.
- Talk about your medical history, taking note of any sleep disorders that you may have had or that may run in your family.
- A sleep specialist should be seen for a more thorough assessment.
- Make sure you don’t have another sleep issue by doing sleep studies during the night or during the day when you snooze.
Will I need tests to confirm my diagnosis?
If your doctor thinks you may have a sleep condition, they might suggest testing. You may need:
- Overnight sleep study (polysomnogram): The test tracks your heart rate, respiration, and mental activity as you sleep. It could let medical professionals spot conditions like sleep apnea or witness an episode of paralysis during sleep.
- Multiple sleep latency test (MSLT): This test determines the type of sleep you get during a nap and how quickly you fall asleep. The most prevalent cause of sleep paralysis, narcolepsy (abnormal daytime drowsiness), is one of the conditions the test helps identify.
How is sleep paralysis treated?
For most people, sleep paralysis does not need therapy. If you have trouble falling or staying asleep, treating any underlying medical conditions, such as narcolepsy, may be useful. The following therapies could be part of these:
- Altering your sleeping patterns, such as confirming that you get between six and eight hours a night
- Abusing antidepressant drugs according to instructions to assist control of sleep cycles
- Managing any mental health issues that might be a factor in sleep paralysis
- Treating any further sleep disorders, like leg cramps or narcolepsy
- Avoiding blue light before sleep
- Ensuring the room temperature is kept low
- You can improve the quality of your sleep at night by following these nighttime routines.
Sleep paralysis symptoms usually go away in a few minutes and don’t result in trauma or long-term bodily damage. it may be an unpleasant and terrifying experience. When isolated sleep paralysis occurs, it usually doesn’t need to be treated. However, people who additionally exhibit narcolepsy symptoms ought to see a physician. This is crucial if symptoms affect one’s ability to function at work or home.
If narcolepsy is the underlying cause of your sleep paralysis, your doctor may prescribe certain medications to help control the condition. Stimulants and selective serotonin reuptake inhibitors (SSRIs), like fluoxetine (Prozac), are the most often prescribed drugs. Using stimulants prolongs your sleep. A polysomnography, a type of sleep study, may be prescribed by your doctor.
Your doctor can diagnose you with narcolepsy if you have sleep paralysis or other symptoms based on the study results. A hospital or sleep center stay of the night is necessary for this kind of research. Electrodes will be applied to the chin, scalp, and outer corners of your eyes by a medical professional as part of this study. Your brain waves and muscle electrical activity are measured by the electrodes. They’ll also keep an eye on your heart rate and respiration. Sometimes as you sleep, a camera records your motions.
Physiotherapy management
When it comes to treating sleep paralysis effectively, physiotherapy and the condition are closely related. To fully understand sleep paralysis and the function of physiotherapy in treating it.
Physiotherapy in healing sleep paralysis:
Should it be a one-night occurrence, you will ultimately forget about it. But if you find yourself in this situation every night or often, you might require some effective treatments. While some people may not respond well to medications, physiotherapy is a safe therapeutic option appropriate for patients of all ages. For this reason, attempt physiotherapy for sleep paralysis at home or by visiting the closest physiotherapy facility or professional. Physiotherapy exercises for relaxation, for strength and to improve circulation to the body.
Physiotherapy has some unique benefits:
- It improves blood circulation throughout the body, which lowers blood pressure, elevates mood, eases tension, and improves blood flow to the brain and body’s organs, all of which contribute to a restful night’s sleep.
- Physiotherapy-induced exercise has two effects on the body. It causes the muscles to contract and also has a massaging effect. This increases tissue temperature and increases muscular elasticity. Because of this, working on exercise before bed can promote a very restful sleep devoid of nightmares and episodes of paralysis.
- Because of the improved blood circulation and the sensation of well-being that results from having flexible, well-trained muscles, you feel happier. The hormones that make you happy and satisfied, known as serotonin, are released into the body and brain after a satisfying physical therapy session, just before bed. This prevents sleep paralysis by promoting stress-free and happy sleep.
What can I do about sleep paralysis?
If you have periodic sleep paralysis, you can take steps at home to prevent this condition. Start by:
- Make sure you get sufficient sleep.
- Do what you can to relieve stress in your life, particularly just before bedtime.
- Try new sleeping situations if you sleep on your back. Sleep specialists have found a correlation between sleeping on your back and sleep paralysis.
Prevention
You can’t do anything to stop yourself from experiencing sleep paralysis. However, there are actions you may take to reduce your risk. Increasing the quality of your sleep is one of the best strategies to prevent sleep paralysis. You can reduce symptoms or the frequency of episodes with a few easy lifestyle changes, such as:
- keeping a regular sleep routine that includes built timings for bedtime and wake-up.
- generating a peaceful, black, and dark sleep space.
- putting electronics such as computers, tablets, e-readers, and phones away before bed.
- having a bath, reading, or enjoying some relaxing music before going to bed.
- Decrease stress in your life.
- Exercise regularly but not close to bedtime.
- Get adequate rest.
- Keep track of medications you take for any diseases.
- To prevent possible adverse effects, such as sleep paralysis, be aware of the interactions and side effects of the many medications you are taking.
- Avoid sleeping on your back by switching to a lateral position.
These suggestions could help in preventing sleep paralysis:
- Therapy
- Trauma counseling
- yoga and breathing practices to reclaim this sense of agency over your body
If you have a mental health disorder, such as anxiety or depression, taking an antidepressant may reduce episodes of sleep paralysis. Antidepressants can help lower the number of dreams you have, which lessens sleep paralysis.
Prognosis
In your lifetime, you might only go through one episode. It could, however, also appear and disappear. You’re more likely to have an episode when you’re sleep-deprived and under a lot of stress. Your healthcare practitioner should be consulted if you experience intermittent sleep loss.
After experiencing an episode of sleep paralysis, how can I take care of myself?
After recovering from sleep paralysis, it’s normal to feel worn out, terrified, and emotional, and for good cause. It is terrible when you get sleep paralysis. Treat yourself with kindness, which includes obtaining more sleep if necessary. If you need consolation, speak with a loved one or visit your doctor.
Note
Paralysis during sleep is uncommon. However, many people have fear following an incident. You could have wondered if anyone would believe what happened because the encounter felt so bizarre.
Don’t allow these emotions to prevent you from getting the care and assistance you require. To reduce the risk of recurrence, a healthcare professional can identify the underlying causes, prescribe medication, or provide advice on self-care.
FAQ
What is the cause of sleep paralysis?
This is a result of your brain being engaged even when you are sleeping. Although the exact cause of sleep paralysis is unknown, it has been connected to insomnia. When you are waking up or going asleep and your muscles are immobile, it is called sleep paralysis.
How can sleep paralysis be stopped?
Increasing the quality of your sleep is one of the best strategies to prevent sleep paralysis. One way to achieve this is to establish a regular sleep pattern that includes precise times for bedtime and wake-up. making a peaceful, dark, and comfy sleeping space.
Which postures cause you to have sleep disorders?
Sleeping in the supine position has been found an especially prominent instigator of sleep paralysis. The high concurrent incidence of sleep paralysis in monozygotic twins is another reason for the belief that RISP may have a genetic component.
Which three sleep paralysis hallucinations are the most common?
In addition to being unable to move or talk, sleep paralysis symptoms can also include a strong terror and a feeling that someone is watching you. But this invader is a delusion. All of us are susceptible to auditory, visual, and sensory hallucinations throughout sleep and in the morning.
Does sleep paralysis cause injury?
When you’re waking up or going to sleep, you may experience temporary paralysis that prevents you from moving or speaking. Though it can be alarming, it shouldn’t be harmful and should pass shortly. Although it can afflict anyone, young adults are most frequently affected. If you are prone to sleep paralysis, consult your physician.
Who can develop sleep paralysis?
While it may appear at any age, teens are typically the first to experience it. Episodes that first surfaced throughout adolescence could occur more frequently in later years if you experience episodes of sleep paralysis that make you feel anxious or if you have repeated episodes of sleep paralysis, speak with your doctor.
References
- Roybal, B. (2008, July 24). Sleep paralysis. WebMD. https://www.webmd.com/sleep-disorders/sleep-paralysis
- Professional, C. C. M. (n.d.-f). Sleep paralysis. Cleveland Clinic. https://my.clevelandclinic.org/health/diseases/21974-sleep-paralysis
- Suni, E., & Suni, E. (2023, December 8). Sleep paralysis: symptoms, causes, and treatment. Sleep Foundation. https://www.sleepfoundation.org/parasomnias/sleep-paralysis
- O’Connell, K. (2021, July 1). Sleep paralysis. Healthline. https://www.healthline.com/health/sleep/isolated-sleep-paralysis
- Restivo, J. (2023, October 20). Sleep paralysis: Causes, symptoms, and treatments. Harvard Health. https://www.health.harvard.edu/diseases-and-conditions/sleep-paralysis-causes-symptoms-and-treatments
- Bradley, S. (2023, May 24). What is sleep paralysis? Health. https://www.health.com/sleep-paralysis-7369673




2 Comments